The healthcare delivery and services landscape in India has evolved significantly over the years. However, India’s healthcare system suffers from various issues like high costs, inconsistent quality, inaccessibility to timely care etc. In this section, we will provide you with the updates, concepts and issues related to health care system in India.
Contents
- 1 Health and related issues in news for UPSC/IAS Examination
- 1.0.0.0.1 Introduction
- 1.0.0.0.2 What are the issues with the current vaccination policy of India?
- 1.0.0.0.3 Suggestions to improve vaccination policy of India
- 1.0.0.0.4 What is the news?
- 1.0.0.0.5 About the Crash Course Programme for Covid-19 Frontline Workers
- 1.0.0.0.6 Key Features of the Scheme
- 1.0.0.0.7 Background
- 1.0.0.0.8 How new technologies can improve the hospital ecosystem?
- 1.0.0.0.9 Challenges in developing Digital health strategy
- 1.0.0.0.10 Introduction:
- 1.0.0.0.11 Delayed vaccination drives for Polio:
- 1.0.0.0.12 Other examples of delayed vaccination drives:
- 1.0.0.0.13 India’s vaccination drive at present:
- 1.0.0.0.14 Background:
- 1.0.0.0.15 Issues associated with 25% quota:
- 1.0.0.0.16 Way Forward:
- 1.0.0.0.17 Introduction:
- 1.0.0.0.18 What is an equity-focused vaccination plan?
- 1.0.0.0.19 Challenges in providing equity-focused vaccination plan
- 1.0.0.0.20 How to improve the equity-focused vaccination plan?
- 1.0.0.0.21 Conclusion:
- 1.0.0.0.22 Synopsis:
- 1.0.0.0.23 Background:
- 1.0.0.0.24 About the Delta Variant:
- 1.0.0.0.25 Data shown by various studies on vaccines:
- 1.0.0.0.26
- 1.0.0.0.27 What is the news?
- 1.0.0.0.28 About Surakshit Hum Surakshit Tum Abhiyaan:
- 1.0.0.0.29 About Transformation of Aspirational Districts programme (TADP):
- 1.0.0.0.30
- 1.0.0.0.31 What is the News?
- 1.0.0.0.32 About the Research:
- 1.0.0.0.33 Inflammatory bowel disease(IBD):
- 1.0.0.0.34
- 1.0.0.0.35 What is the News?
- 1.0.0.0.36 How does Aducanumab drug work?
- 1.0.0.0.37 About Alzheimer’s Disease:
- 1.0.0.0.38 Why mental healthcare situation is bad in India?
- 1.0.0.0.39 Why Mental Health needs to be given priority?
- 1.0.0.0.40 Government measures on mental health care
- 1.0.0.0.41 What more steps can be taken?
- 1.0.0.0.42 Synopsis:
- 1.0.0.0.43 Background:
- 1.0.0.0.44 Understanding the Downward Trajectory of Second Wave:
- 1.0.0.0.45 Suggestions to capitalise the downward Trajectory of Second Wave:
- 1.0.0.0.46 Background:
- 1.0.0.0.47 About Reproduction number (R):
- 1.0.0.0.48 What led R to increase earlier this year resulting in a second wave?
- 1.0.0.0.49 Suggestions for Mitigating the third wave:
- 1.0.0.0.50
- 1.0.0.0.51 What is the news?
- 1.0.0.0.52 Mechanism of Coronavirus Infection:
- 1.0.0.0.53 Global studies on vulnerability of animals to Covid-19:
- 1.0.0.0.54 A study by PNAS, a research journal of US:
- 1.0.0.0.55 A study by the University of Bologna regarding vulnerability of animals to Covid-19:
- 1.0.0.0.56
- 1.0.0.0.57 What is the News?
- 1.0.0.0.58 About Revised Vaccine Procurement Policy:
- 1.0.0.0.59 Free for All Vaccine:
- 1.0.0.0.60 Extension of Pradhan Mantri Garib Kalyan Yojana:
- 1.0.0.0.61 Reasons for announcing revised Vaccine Procurement Policy
- 1.0.0.0.62 Introduction-
- 1.0.0.0.63 What is behavioural science?
- 1.0.0.0.64 How behavioural science methods can be used in COVID-19 prevention?
- 1.0.0.0.65 Way forward
- 1.0.0.0.66 Introduction
- 1.0.0.0.67 What are the challenges India is likely to face?
- 1.0.0.0.68 What should India do to prevent the third wave?
- 1.0.0.0.69 Background
- 1.0.0.0.70 Arguments in support of lab leak theory of Coronavirus
- 1.0.0.0.71 Introduction
- 1.0.0.0.72 Impact of the pandemic in Rural India
- 1.0.0.0.73 Need to give attention to Rural India during the Pandemic
- 1.0.0.0.74 Government Initiatives towards the betterment of Rural India during the pandemic
- 1.0.0.0.75 Challenges in vaccination and controlling the pandemic in rural India
- 1.0.0.0.76 Suggestions to tackle the pandemic in Rural India
- 1.0.0.0.77 Conclusion
- 1.0.0.0.78 What is the news?
- 1.0.0.0.79 About the effectiveness of vaccines:
- 1.0.0.0.80 Key Findings regarding the effectiveness of vaccines:
- 1.0.0.0.81
- 1.0.0.0.82 What is the news?
- 1.0.0.0.83 What is the Delta Variant of Covid-19?
- 1.0.0.0.84 What is Variant of Concern (VOC)?
- 1.0.0.0.85 Why is Delta Variant more dangerous than other variants?
- 1.0.0.0.86 What is a mutation?
- 1.0.0.0.87
- 1.0.0.0.88 What is the News?
- 1.0.0.0.89 About Corbevax Vaccine:
- 1.0.0.0.90 What are Spike Proteins?
- 1.0.0.0.91 Different types of Covid-19 vaccines:
- 1.0.0.0.92 How is the Corbevax Vaccine different from these vaccines?
- 1.0.0.0.93 Inadequate and poor health infrastructure in the rural areas
- 1.0.0.0.94 Significance of rural health infrastructure in effective delivery of health Services
- 1.0.0.0.95 Suggestions to improve rural health infrastructure:
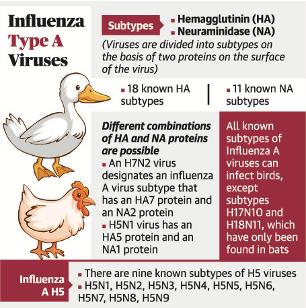
- 1.0.0.0.96 About H10N3 strain of Bird Flu:
- 1.0.0.0.97 Synopsis:
- 1.0.0.0.98 Background:
- 1.0.0.0.99 Understanding the issue:
- 1.0.0.0.100 Lessons from this episode:
- 1.0.0.0.101 Introduction
- 1.0.0.0.102 Previous such examples of mental health issues
- 1.0.0.0.103 What is Mental illness?
- 1.0.0.0.104 India and Mental health
- 1.0.0.0.105 Challenges in improving mental health in India
- 1.0.0.0.106 Global steps to improve mental health
- 1.0.0.0.107 Indian initiatives to improve mental health
- 1.0.0.0.108 Suggestions to improve Mental health in India
- 1.0.0.0.109 Conclusion
- 1.0.0.0.110 Introduction
- 1.0.0.0.111 Implications of Secrecy
- 1.0.0.0.112 Way forward
- 1.0.0.0.113 Introduction-
- 1.0.0.0.114 What is India’s NCD strategy?
- 1.0.0.0.115 Suggestions to tackle the twin challenges of the COVID pandemic and NCD morbidities
- 1.0.0.0.116 Way forward-
- 1.0.0.0.117 Background
- 1.0.0.0.118 What are the challenges facing India’s Covid Diplomacy 2.0?
- 1.0.0.0.119 Way forward
- 1.0.0.0.120
- 1.0.0.0.121 What is the News?
- 1.0.0.0.122 What is the New System for Quick Clearance of Claims?
- 1.0.0.0.123 About Pradhan Mantri Garib Kalyan Package Insurance Scheme for health workers Fighting Covid-19:
- 1.0.0.0.124 About the Resolution to End Malaria:
- 1.0.0.0.125 About WHOs Global Malaria Program:
- 1.0.0.0.126 Global Technical Strategy for malaria 2016–2030
- 1.0.0.0.127 About Malaria:
- 1.0.0.0.128
- 1.0.0.0.129 What is the News?
- 1.0.0.0.130 About World No Tobacco Day:
- 1.0.0.0.131 Tobacco Consumption in India:
- 1.0.0.0.132 What are the issues raised by the Supreme Court?
- 1.0.0.0.133 Different Criteria for Age Groups:
- 1.0.0.0.134 Digital Divide and COWIN registration.
- 1.0.0.0.135 About World Neglected Tropical Diseases (NTD) Day:
- 1.0.0.0.136 About Neglected Tropical Diseases(NTD):
- 1.0.0.0.137 About London Declaration:
- 1.0.0.0.138 WHO’s New Roadmap for NTDs for 2021-30:
- 1.0.0.0.139 Introduction
- 1.0.0.0.140 What are the adverse effects of the pandemic on young healthcare workers?
- 1.0.0.0.141 The conclusion
- 1.0.0.0.142 Introduction
- 1.0.0.0.143 Pre-conditions to supply Vaccine to India:
- 1.0.0.0.144 What needs to be done in order to increase procurement?
- 1.0.0.0.145 How real-time data on public health can help fight against the Pandemic?
- 1.0.0.0.146 Challenges in generating real-time data on public health
- 1.0.0.0.147 Introduction
- 1.0.0.0.148 What is AYUSH?
- 1.0.0.0.149 Institutional Framework for AYUSH
- 1.0.0.0.150 Role of AYUSH medicines used during pandemic
- 1.0.0.0.151 Challenges faced by AYUSH medicines and practitioners
- 1.0.0.0.152 Suggestions to improve the role of AYUSH
- 1.0.0.0.153 Conclusion
- 1.0.0.0.154
- 1.0.0.0.155 What is the News?
- 1.0.0.0.156 What did the Global Study on the Origin of Covid-19 found?
- 1.0.0.0.157 India’s stand on WHO’s study:
- 1.0.0.0.158 What is the News?
- 1.0.0.0.159 About Ayush Clinical Case Repository(ACCR):
- 1.0.0.0.160 Significance of this Portal:
- 1.0.0.0.161 About Ayush Sanjivani app:
- 1.0.0.0.162
- 1.0.0.0.163 What is the News?
- 1.0.0.0.164 About Paediatric Inflammatory Multisystem Syndrome(PIMS-TS):
- 1.0.0.0.165 About the Lancet Study:
- 1.0.0.0.166
- 1.0.0.0.167 What is the News?
- 1.0.0.0.168 About Mucormycosis:
- 1.0.0.0.169 Preventive steps to avoid Mucormycosis:
- 1.0.0.0.170 What is the News?
- 1.0.0.0.171 About Yellow Fungus:
- 1.0.0.0.172 Why is Yellow Fungus more dangerous than black and White Fungus?
- 1.0.0.0.173
- 1.0.0.0.174 What is the News?
- 1.0.0.0.175 Key Highlights of the Summit: During the Summit:
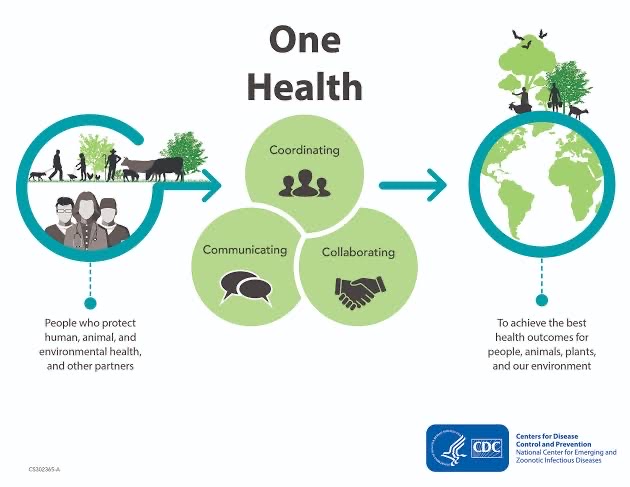
- 1.0.0.0.176 About European Union(EU):
- 1.0.0.0.177 About One Health High-Level Expert Panel:
- 1.0.0.0.178 What is One Health Approach?
- 1.0.0.0.179 What are Zoonotic Diseases?
- 1.0.0.0.180 Background
- 1.0.0.0.181 What are the issues in the Liberalised and Accelerated Phase 3 Strategy of COVID-19 Vaccination?
- 1.0.0.0.182 What needs to be done?
- 1.0.0.0.183 Introduction
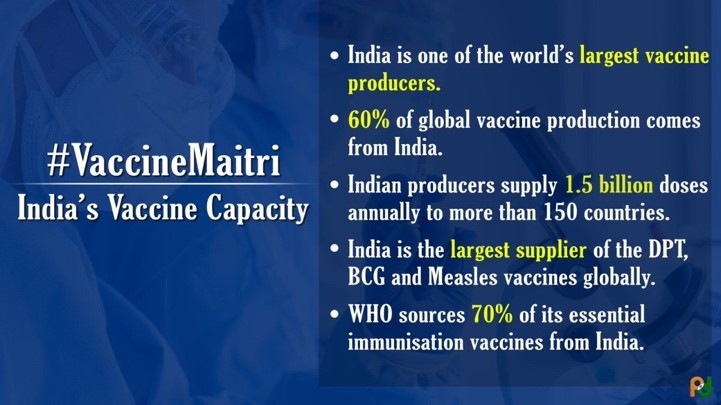
- 1.0.0.0.184 Present status of vaccine manufacturing in India
- 1.0.0.0.185 Global Vaccine sources and producers
- 1.0.0.0.186 Government initiatives in vaccine procurement
- 1.0.0.0.187 Challenges in Vaccine procurement
- 1.0.0.0.188 Suggestions
- 1.0.0.0.189 Way forward
- 1.0.0.0.190
- 1.0.0.0.191 What is the News?
- 1.0.0.0.192 About Global Health Summit 2021:
- 1.0.0.0.193 Rome Declaration:
- 1.0.0.0.194 Key Features of the Rome Declaration:
- 1.0.0.0.195 What is the News?
- 1.0.0.0.196 About Point-of-Care Test:
- 1.0.0.0.197 Significance of Point of Care Test:
- 1.0.0.0.198 About Kyasanur Forest disease:
- 1.0.0.0.199 Background
- 1.0.0.0.200 Why the allocation for the health sector should be increased?
- 1.0.0.0.201 Why Centre government should procure vaccines?
- 1.0.0.0.202 Background
- 1.0.0.0.203 How voluntary licensing can make medical drugs affordable?
- 1.0.0.0.204 What are the issues in other alternative mechanisms?
- 1.0.0.0.205 Way forward
- 1.0.0.0.206 Background
- 1.0.0.0.207 Why IIT’s demands should not be encouraged?
- 1.0.0.0.208 Introduction:
- 1.0.0.0.209 Two underlying principles behind longer vaccine gaps:
- 1.0.0.0.210 Challenges with longer vaccine gaps:
- 1.0.0.0.211 Way forward:
- 1.0.0.0.212 About Pradhan Mantri Swasthya Suraksha Yojana(PMSSY):
- 1.0.0.0.213 Significance of the Scheme:
- 1.0.0.0.214 About White Fungus:
- 1.0.0.0.215 Introduction
- 1.0.0.0.216 Biomedical waste generation during the pandemic
- 1.0.0.0.217 What is biomedical waste?
- 1.0.0.0.218 Biomedical waste management rules in India
- 1.0.0.0.219 Biomedical waste management practice in India
- 1.0.0.0.220 Effects of biomedical waste in India
- 1.0.0.0.221 Suggestions to improve biomedical waste management
- 1.0.0.0.222 Conclusion
- 1.0.0.0.223 What is the News?
- 1.0.0.0.224 Government Advisory:
- 1.0.0.0.225 Background:
- 1.0.0.0.226 Concerns regarding vaccine policy:
- 1.0.0.0.227 Way Forward:
- 1.0.0.0.228
- 1.0.0.0.229 What is the News?
- 1.0.0.0.230 What is Mucormycosis?
- 1.0.0.0.231 What is Epidemic, Pandemic, and Endemic?
- 1.0.0.0.232 What measures should be taken to prevent future waves of pandemic disaster?
- 1.0.0.0.233 Background
- 1.0.0.0.234 What needs to be done?
- 1.0.0.0.235 Introduction
- 1.0.0.0.236 Status of brain drain in the health sector in India
- 1.0.0.0.237 Reasons for brain drain in the health sector
- 1.0.0.0.238 Government measures to tackle the brain drain in the health sector
- 1.0.0.0.239 Suggestions to reduce brain drain in the health sector
- 1.0.0.0.240 Conclusion
- 1.0.0.0.241
- 1.0.0.0.242 What is the News?
- 1.0.0.0.243 About SAMVEDNA:
- 1.0.0.0.244 About National Commission for Protection of Child Rights(NCPCR)
- 1.0.0.0.245 Background
- 1.0.0.0.246 What do the global estimates reveal about the Covid deaths?
- 1.0.0.0.247 What needs to be done?
- 1.0.0.0.248 Introduction:
- 1.0.0.0.249 Lockdown and prerequisites:
- 1.0.0.0.250 Lessons from Kerala model to tackle the pandemic:
- 1.0.0.0.251 Suggestions:
- 1.0.0.0.252
- 1.0.0.0.253 What is the News?
- 1.0.0.0.254 About the Covid-19 guidelines for rural areas:
- 1.0.0.0.255 Other Key Covid-19 guidelines for rural areas:
- 1.0.0.0.256
- 1.0.0.0.257 What is the News?
- 1.0.0.0.258 About the CDC Guidelines:
- 1.0.0.0.259 Places where the persons need to wear masks:
- 1.0.0.0.260 Introduction-
- 1.0.0.0.261 Key issues with the current technocratic based vaccination drive
- 1.0.0.0.262 What are the key principles forgone by the government?
- 1.0.0.0.263 Introduction-
- 1.0.0.0.264 How can the state bring down vaccine prices?
- 1.0.0.0.265 Suggestions to reduce Vaccine price and provide universal vaccination
- 1.0.0.0.266 Background of Pandemic in rural India
- 1.0.0.0.267 Challenges in tackling Pandemic in rural India:
- 1.0.0.0.268 Suggestions to tackle Pandemic in rural India
- 1.0.0.0.269 What is the News?
- 1.0.0.0.270 About Categorisation of diseases:
- 1.0.0.0.271 What is the category of the Sporadic case?
- 1.0.0.0.272 What is the Cluster of Cases category?
- 1.0.0.0.273 What is Community Transmission(CT)?
- 1.0.0.0.274 Countries classified under Community Transmission:
- 1.0.0.0.275 Government policy based on Categorisation:
- 1.0.0.0.276 Background:
- 1.0.0.0.277 About the Vaccine Policy:
- 1.0.0.0.278 Issues with vaccine policy that demands a relook:
- 1.0.0.0.279 Way Forward:
- 1.0.0.0.280 What is the News?
- 1.0.0.0.281 About Ivermectin Drug:
- 1.0.0.0.282 Facts on Digital inequality in India
- 1.0.0.0.283 Reasons behind Digital inequality in education
- 1.0.0.0.284 Reasons behind Digital inequality in health
- 1.0.0.0.285 Way forward
- 1.0.0.0.286 Background
- 1.0.0.0.287 Issues in the Indian health care system
- 1.0.0.0.288 How the British National Health Service function?
- 1.0.0.0.289 What is the News?
- 1.0.0.0.290 e-ICU Platform:
- 1.0.0.0.291 Introduction:
- 1.0.0.0.292 The Situation of India during the 1960s:
- 1.0.0.0.293 Advantages for present India vis-à-vis 1960s:
- 1.0.0.0.294 Suggestions:
- 1.0.0.0.295 Introduction
- 1.0.0.0.296 Benefits of a lockdown
- 1.0.0.0.297 Way forward
- 1.0.0.0.298
- 1.0.0.0.299 What is the News?
- 1.0.0.0.300 About 2-deoxy-D-glucose (2-DG):
- 1.0.0.0.301 Significance of this drug:
- 1.0.0.0.302 What is the News?
- 1.0.0.0.303 About Project MediCAB:
- 1.0.0.0.304
- 1.0.0.0.305 What is the News?
- 1.0.0.0.306 About Ayush 64:
- 1.0.0.0.307 About Black Fungus Infection:
- 1.0.0.0.308 What are the reasons for the current Covid crisis?
- 1.0.0.0.309 Further steps to take?
- 1.0.0.0.310 Background
- 1.0.0.0.311 Validation on the effectiveness of CT scan test for Covid
- 1.0.0.0.312 Way forward
- 1.0.0.0.313 What is the News?
- 1.0.0.0.314 About Ayush-64:
- 1.0.0.0.315 SUTRA Model:
- 1.0.0.0.316 Why Scientists are calling the SUTRA model flawed?
- 1.0.0.0.317 What did the scientists working on the SUTRA model said?
- 1.0.0.0.318 Background:
- 1.0.0.0.319 About Malaria:
- 1.0.0.0.320 About the Previous Version:
- 1.0.0.0.321 About the new version:
- 1.0.0.0.322 Need of New Malaria Vaccine:
- 1.0.0.0.323 What’s next?
- 1.0.0.0.324 Background
- 1.0.0.0.325 What is the One Health Approach?
- 1.0.0.0.326 Steps taken by India towards ‘One Health’:
- 1.0.0.0.327 Challenges hindering the success of one health approach:
- 1.0.0.0.328 Way Forward:
- 1.0.0.0.329 Introduction:
- 1.0.0.0.330 Vaccine shortage:
- 1.0.0.0.331 How India expected to tackle the vaccine shortage?
- 1.0.0.0.332 Interval between two doses:
- 1.0.0.0.333 Present condition of vaccination in India:
- 1.0.0.0.334 Suggestions to avoid vaccine shortage:
- 1.0.0.0.335
- 1.0.0.0.336 What is the News?
- 1.0.0.0.337 Background:
- 1.0.0.0.338 Key observations on seeking medical help for COVID-19:
- 1.0.0.0.339 World Immunisation Week:
- 1.0.0.0.340 About Immunisation Agenda 2030(IA2030):
- 1.0.0.0.341 Key Features of Immunisation Agenda 2030:
- 1.0.0.0.342 Targets:
- 1.0.0.0.343 Significance:
- 1.0.0.0.344
- 1.0.0.0.345 What is the News?
- 1.0.0.0.346 About Emergency Financial Powers to Armed Forces:
- 1.0.0.0.347 Who has these powers?
- 1.0.0.0.348 Duration:
- 1.0.0.0.349 Other Organizations contribution during the pandemic:
- 1.0.0.0.350 Introduction:
- 1.0.0.0.351 How does the government regulate the pricing of drugs?
- 1.0.0.0.352 What prices the government cannot regulate?
- 1.0.0.0.353 Various ways to regulate the pricing of vaccines:
- 1.0.0.0.354 Way forward:
- 1.0.0.0.355 Background
- 1.0.0.0.356 How the possibility of a third wave can be Prevented?
- 1.0.0.0.357 How to persuade people to wear masks?
- 1.0.0.0.358 How India can replicate this model to Nudge Mask wearing?
- 1.0.0.0.359 Introduction
- 1.0.0.0.360 What are the other issues in the COVID-19 management guidelines?
- 1.0.0.0.361 What changes are needed?
- 1.0.0.0.362 What is the News?
- 1.0.0.0.363 About Trachoma:
- 1.0.0.0.364 SAFE Strategy:
- 1.0.0.0.365 Background:
- 1.0.0.0.366 What is Herd immunity?
- 1.0.0.0.367 What is a Serological Survey?
- 1.0.0.0.368 Understanding the current spread: –
- 1.0.0.0.369 Future Trajectory:
- 1.0.0.0.370 Background
- 1.0.0.0.371 What are the issues with the new vaccine strategy?
- 1.0.0.0.372 Way forward
- 1.0.0.0.373 Introduction
- 1.0.0.0.374 India’s vaccination policy so far
- 1.0.0.0.375 Salient features of India’s new vaccination policy
- 1.0.0.0.376 Other steps taken towards universal vaccination in India
- 1.0.0.0.377 Need for achieving universal vaccination in India
- 1.0.0.0.378 Challenges to universal vaccination in the Covid-19
- 1.0.0.0.379 Suggestions to improve universal vaccination in India
- 1.0.0.0.380 Conclusion
- 1.0.0.0.381 Background
- 1.0.0.0.382 Steps Taken to Accelerate India’s Vaccination drive?
- 1.0.0.0.383 What needs to be done?
- 1.0.0.0.384 What is it?
- 1.0.0.0.385 Possible Reasons for Breakthrough Infections:
- 1.0.0.0.386 India’s Breakthrough Infections Data:
- 1.0.0.0.387 Concerns:
- 1.0.0.0.388 Introduction
- 1.0.0.0.389 How the new Vaccine policy could result in vaccine failure?
- 1.0.0.0.390 What is the solution?
- 1.0.0.0.391 Background
- 1.0.0.0.392 What are the reasons for the spurt in Covid 19 infection?
- 1.0.0.0.393 What needs to be done?
- 1.0.0.0.394 Steps to minimise the number of lockdown days:
- 1.0.0.0.395 What is the News?
- 1.0.0.0.396 About Harlequin ichthyosis:
- 1.0.0.0.397 Who conducted the study?
- 1.0.0.0.398 Key Findings from the study:
- 1.0.0.0.399 About Virafin Drug:
- 1.0.0.0.400 Background
- 1.0.0.0.401 How the China Model functioned?
- 1.0.0.0.402 About Residential Committees
- 1.0.0.0.403 Role of Central Leadership
- 1.0.0.0.404 How the China Model can be replicated in India?
- 1.0.0.0.405 Earlier Three Phases:
- 1.0.0.0.406 Fourth Phase of Covid-19 Vaccine Policy:
- 1.0.0.0.407 Changes in Distribution:
- 1.0.0.0.408 Imported Vaccines:
- 1.0.0.0.409 Background
- 1.0.0.0.410 What are the roadblocks to achieve universal vaccination for all?
- 1.0.0.0.411 Background:
- 1.0.0.0.412 Reactive approach:
- 1.0.0.0.413 Concerns associated with Reactive approach:
- 1.0.0.0.414 New Approach of using Secondary Level Health Services:
- 1.0.0.0.415 Benefits of the Secondary Level Health Services:
- 1.0.0.0.416 Way Forward:
- 1.0.0.0.417 About Global Diabetes Compact Initiative:
- 1.0.0.0.418 About Diabetes:
- 1.0.0.0.419 Types of Diabetes:
- 1.0.0.0.420 Potential of India’s vaccine exports:
- 1.0.0.0.421 Why India need to export vaccine?
- 1.0.0.0.422 How India calculates the number of Vaccines that it exports?
- 1.0.0.0.423 Questions surrounding quantum of exporting vaccine:
- 1.0.0.0.424 Introduction
- 1.0.0.0.425 How did the first wave lead to uneven growth?
- 1.0.0.0.426 Suggestions
- 1.0.0.0.427 The conclusion
- 1.0.0.0.428 About MANAS App:
- 1.0.0.0.429 About Office of the Principal Scientific Adviser(PSA):
- 1.0.0.0.430 About PM-STIAC:
- 1.0.0.0.431 Introduction
- 1.0.0.0.432 How the clinical trials helped in finding the best treatment?
- 1.0.0.0.433 What are the drugs that have been proven to benefit COVID-19 patients?
- 1.0.0.0.434 About National Commission for Allied and Healthcare Professions [NCAHP] Bill, 2020
- 1.0.0.0.435 Key provisions of the NCAHP bill 2020
- 1.0.0.0.436 Way forward-
- 1.0.0.0.437 India’s vaccination strategy:
- 1.0.0.0.438 Concerns with India’s vaccination strategy:
- 1.0.0.0.439 Suggestions to improve India’s Vaccine strategy:
- 1.0.0.0.440 What is the News?
- 1.0.0.0.441 What are Zoonotic Diseases?
- 1.0.0.0.442 Key Guidelines issued by WHO:
- 1.0.0.0.443 About ICMR’s International Symposium
- 1.0.0.0.444 About One Health:
- 1.0.0.0.445 Importance of Approach:
- 1.0.0.0.446 Application areas of One Health
- 1.0.0.0.447 Examples of Approach:
- 1.0.0.0.448 What is a Rare Disease?
- 1.0.0.0.449 What are the key highlights of the policy?
- 1.0.0.0.450 Concern with the Policy-
- 1.0.0.0.451 Way forward-
- 1.0.0.0.452 What is the News?
- 1.0.0.0.453 About National Policy For Rare Diseases,2021:
- 1.0.0.0.454 Objections to the Policy:
- 1.0.0.0.455 What is the News?
- 1.0.0.0.456 About Tribal TB Initiative:
- 1.0.0.0.457 Why was this initiative launched?
- 1.0.0.0.458 Other Tribal Health-Related Initiatives:
- 1.0.0.0.459 What is the News?
- 1.0.0.0.460 What is Double Mutation?
- 1.0.0.0.461 Is this double Mutant COVID Variant Harmful?
- 1.0.0.0.462 About INSACOG:
- 1.0.0.0.463 Global Initiative on Sharing All Influenza Data(GISAID) Initiative
- 1.0.0.0.464 What is the News?
- 1.0.0.0.465 About Parosmia:
- 1.0.0.0.466 What is the News?
- 1.0.0.0.467 About Candida Auris:
- 1.0.0.0.468 Origin of Candida Auris:
- 1.0.0.0.469 Symptoms of C.Auris:
- 1.0.0.0.470 Vulnerable Population:
- 1.0.0.0.471 Treatment:
- 1.0.0.0.472 Introduction-
- 1.0.0.0.473 Data on Blood Clot:
- 1.0.0.0.474 Suggestions to improve vaccination programmes
- 1.0.0.0.475 What is the News?
- 1.0.0.0.476 About Stop TB Partnership:
- 1.0.0.0.477 India’s Initiatives against Tuberculosis:
- 1.0.0.0.478 Background:
- 1.0.0.0.479 About Gestational Diabetes:
- 1.0.0.0.480 Impact of Gestational Diabetes:
- 1.0.0.0.481 Challenges in Managing Gestational Diabetes:
- 1.0.0.0.482 Way Forward:
- 1.0.1 Introduction:
- 1.0.2 What is dry run of Vaccines?
- 1.0.3 India’s vaccine distribution infrastructure
- 1.0.4 Some of the important facts and figures
- 1.0.5 What are the challenges in vaccine distribution in India?
“Health infrastructure” has increased 45-fold during the pandemic: Centre
What is the News?
The Government of India has informed the Supreme Court about the status of India’s Healthcare infrastructure to tackle the Covid-19 pandemic.
India’s Healthcare Infrastructure Status:
- India’s Health Infrastructure has increased up to 45-fold to tackle the successive waves of the COVID-19 pandemic.
- The total cumulative vaccine coverage was 27.23 crore doses as of June 19, 2021.
- The total intensive care unit(ICU) beds had increased by 45-fold from a baseline of 2,500 to around 1.13 lakh.
- The total isolation beds (excluding ICU beds) had climbed 42-fold, from 41,000 to 17.17 lakh.
- Oxygen-supported beds have multiplied 7.5-fold from 50,000 to around 3.81 lakh.
- Around 1.5 lakh health personnel had been engaged on the ground to tackle the Covid-19 pandemic.
- The insurance coverage was given to 22.12 lakhs health care workers, including ASHA workers fighting COVID-19.
- Testing capacity had been increased from 30,000 tests a day in April 2020 to a high of 22 lakh tests daily.
Source: The Hindu
Read Also :-Revitalizing Coal Bed Methane in India
Vaccination policy of India – Issues & Suggestions
Synopsis: The vaccination policy of India should maintain a balance between the achievement of health goals and demands of supply constraints.
Introduction
Vaccines are a proven shield against the SARS-CoV-2 virus. They have prevented serious illness and death. A study of data from the UK collected between December 1, 2020, and April 30, 2021, showed that the AstraZeneca vaccine had an effectiveness of 64% after one dose and 79% after two doses, in protecting against severe illness and death.
- Effectiveness of AstraZeneca vaccine: A report by Public Health England showed that the AstraZeneca vaccine had an effectiveness of 71% after one dose and 92% after two doses in guarding against hospitalization due to the delta variant.
- Effectiveness of COVISHIELD in India: The first report of vaccine effectiveness from India, told an analysis of 8,991 staff who had been vaccinated between January 21, 2021, and April 30, 2021, mostly with Covishield. The protective effect of vaccination was 92% against the need for oxygen and 94% against the need for intensive care.
- No deaths were reported, but about 10% of those who had received one or two doses were infected.
- These data from the United Kingdom and India show that the Covishield vaccine is working against the delta variant.
What are the issues with the current vaccination policy of India?
- Too much focus on herd immunity. When vaccines seemed to be somewhere in the future with doubts over timing or supply, discussions on the pandemic focused on ‘herd immunity’ (the percentage of the population that needed to be infected or vaccinated in order to slow the spread of infection)
- The opening of age tiers led to issues of supply. A road map of the availability of vaccines and their supply to individual States is not clear.
- The Swedish strategy of limited restrictions and the Great Barrington declaration attracted much criticism. Many scientific commentators considered it is cruel to follow a strategy that meant that a lot of people would get infected with the virus.
- Anti-science statements made by some people have led to a situation where the public is confused as to how best to cope with the coronavirus. Uncertainty on vaccine availability, doubt, fear, anxiety and depression are widespread.
Also read: What is herd immunity? Suggestions to improve vaccination policy of India
Different needs at different levels require policy approaches that balance the achievement of health and societal goals with the potential impact and the needs of supply constraints.
- Vaccinating a large number of people: The strategy needs to achieve maximum impact. We need to vaccinate a large proportion of the population and extend it at a later stage to children to both prevent disease and slow spread.
- Plan for children as well: The advent of the delta variant made it clear that the previous plan to vaccinate a smaller part of the population is not right, and reaching up to 85% of the population might be required. This means that along with all adults, we should be planning for children as well to achieve Universal Vaccination.
- Vaccinating the high-risk group first: We must vaccinate those most at risk from serious illness and death first based on the principles of public health. The high rates of previous waves in India may make it possible to immunize a large part of our population with a single dose, at least initially.
- Ensuring expansive reach of the vaccine: The vaccine should reach every village. Community leaders should be empowered with information and tools to broadcast the message that the vaccine saves lives.
- The central government has centralized vaccine purchase, but it must revisit the private sector allocation and give distribution to States, providing support when requested. The CoWIN app must not be a limiting factor in access to the vaccine.
- An adaptive vaccination policy: The vaccination policy must be adapted quickly to changing circumstances. We must create models to find a suitable vaccination strategy for younger populations.
- If cases are climbing in a particular region, we should direct vaccine doses there to protect as much of the population. High vaccination coverage in cities may protect rural areas. The Government must trust its citizens and share the information as it is a notable aspect of the pandemic.
- Open sharing of the data: The Government must trust its citizens and share the information that is solely available to it. A notable aspect of the pandemic is the absence of credible data from the government. This has led to speculative ideas based on poor or poorly understood information and misinformation.
Conclusion
Addressing the pandemic must include a strategy that ensures maximum impact. This can be done with an expansive vaccination policy that adapts itself on the go and covers the needs of every section of our society.Source: Click here
PM launches crash-course program to train 1 lakh Covid-19 frontline workers
What is the news?
Prime Minister has launched a “customized crash course programme for Covid-19 frontline workers”.
About the Crash Course Programme for Covid-19 Frontline Workers
- Aim: The programme aims to create skilled non-medical healthcare workers to fill the present and future needs of manpower in the health sector.
- This will be done by providing fresh skills and upskills to over one lakh Covid warriors across the country.
- Nodal Scheme: The course has been designed under the Central Component of Pradhan Mantri Kaushal Vikas Yojana 3.0.
Key Features of the Scheme
- Firstly, the programme would be available at 111 training centers across 26 states in the country.
- Secondly, the Covid warriors will be trained under six modules. These modules include:
- Home Care Support
- Basic Care Support
- Advanced Care Support
- Emergency Care Support
- Sample Collection Support and
- Medical Equipment Support.
- Lastly, the trained workers will then assist doctors in the treatment of COVID 19 patients.
Source: India Today
- Aim: The programme aims to create skilled non-medical healthcare workers to fill the present and future needs of manpower in the health sector.
Role of disruptive technologies in improving the health sector
Synopsis: Application of future Digital technologies in the health sector can lead to accessible, affordable, and quality health care. Further, it can reduce human involvement in risky functions.
Background
- Human involvement in diagnosis, treatment, and hospital care of infected patients puts them at greater risk of contracting the disease. For instance, many frontline warriors fighting COVID-19 have lost their lives.
- In this context, technologies such as artificial intelligence (AI), autonomous systems, blockchain, cloud and quantum computing, data analytics, 5G can help in addressing the issue.
- The new technologies can improve the welfare of societies and reduce the impact of communicable diseases. Further, it can reduce the chances of hospital staff contracting the infection.
Recent developments regarding the use of disruptive technologies for hospital care
- One, according to global media reports, some established innovative field hospitals are using robots to care for COVID-19 affected patients.
- Two, hospitals in China, are using 5G-powered temperature measurement devices at the entrance to flag patients who have fever-like symptoms.
- Three, some robots are being used to measure heart rates and blood oxygen levels through smart bracelets.
- Four, In India too, the Sawai Man Singh government hospital in Jaipur held trials with a humanoid robot to deliver medicines and food to hospitalized COVID-19 patients
How new technologies can improve the hospital ecosystem?
- One, Blockchain technology can help in addressing the interoperability challenges that health information and technology systems face.
- The health blockchain will contain a complete indexed history of all medical data, including formal medical records and health data. Data will be sourced from mobile applications and wearable sensors. This will help in seamless medical attention.
- Further, it allows for storing of data in a secured and authenticated network. Thereby, it will prevent erosion of Individuals’ privacy and ensure data security.
- Two, Big data analytics can help improve patient-based services such as early disease detection.
- Three, AI and the Internet of Medical Things, or IoMT can support medical care delivery in dispersed and complex environments through Medical autonomous systems.
- Four, Cloud computing can facilitate collaboration and data exchanges between doctors, departments, and even institutions and medical providers. It will enable the best treatment.
Read Also :-Digital nation: On delivery of citizen services
How Digital technologies can be utilized to achieve “Universal health coverage” in India?
- India needs to own its digital health strategy that works and leads towards universal health coverage and person-centered care.
- India’s digital health strategy should emphasize the ethical appropriateness of digital technologies, across the digital divide, and ensure inclusion across the economy.
- Online consultation through video conferencing should be made a key part of India’s digital health strategy.
- Moreover, digital health strategy should utilise available local knowledge. Primary health centres in India should examine traditional knowledge and experience and then use it along with modern technology.
- There are many instances where traditional knowledge has been utilised for preventing diseases.
- For example, in Indonesia, where the experience of backyard poultry farmers was used to tackle bird flu.
- Another example is the Ebola virus outbreak in Africa, where communities proactively helped curtail the spread much before government health teams arrived.
Challenges in developing Digital health strategy
- Standardisation of health data,
- Information sharing between Organisations
- Data security and data privacy, and
- High investments.
India’s efforts in this direction should involve synchronization and integration, developing a template for sharing data, and reengineering many of the institutional and structural arrangements in the medical sector.
Source: The Hindu
Read Also :-Making Education Accessible and Affordable
Achievements of India’s Vaccination Drive
Synopsis: The COVID-19 vaccination drive demonstrates that India has become Atmanirbhar in vaccination campaigns of the future.
Contents
Introduction:
Recently, the Indian Prime Minister talked about the past vaccination campaigns in India. He mentioned that earlier India has to wait for decades to procure vaccines from foreign countries. As they need to complete their vaccination programs first before selling vaccines to countries like India.
Furthermore, indigenous manufacturing of vaccines not only started late but also fell short of the demand in India for a long time. This forced the government to continue relying on imports.
Delayed vaccination drives for Polio:
Infectious diseases posed an enormous challenge to Independent India. This along with the delayed vaccination drives took countless lives. For example,
- The Inactivated Polio Vaccine (IPV) and Oral Polio Vaccine (OPV) were licensed abroad in 1955 and 1961, respectively. But it took two decades for India to start polio vaccination drives.
- The OPV was introduced in India through the Expanded Programme on Immunisation (EPI) in urban and rural populations in 1978 and 1981, respectively.
- Prior to this EPI programme, India witnessed more than 10,000 officially recorded cases of polio annually.
- Moreover, India had to rely on imports for both OPV and IPV.
- The OPV was produced by the Pasteur Institute of India, Tamil Nadu, but the Health Ministry closed down this unit in 1974.
- The IPV could not be manufactured as it was licensed only in 2006.
Other examples of delayed vaccination drives:
This is just one example. But the majority of Indian vaccination drives followed this pattern only.
- Delayed vaccination drives for Hepatitis B
- India started mass vaccination for Hepatitis B two decades after commercial availability of the vaccine in the U.S. in 1982.
- The Hepatitis B vaccination was introduced in India’s Universal Immunisation Programme in 2002 only. Even then also, it was introduced only in 14 cities.
- Delayed vaccination drives for smallpox
- In 1962, almost a decade after North America and Europe eradicated smallpox, India launched the National Smallpox Eradication Program.
- India had an adequate stock of domestically produced low-potency liquid vaccine. But for the highly potent freeze-dried vaccine, India completely depended on the Soviet Union and the World Health Organization (WHO)
- Further, India also had to rely on the WHO for bifurcated needles required for the smallpox vaccine.
- This led to higher disease outbreak in certain regions. For example, States like Bihar and West Bengal witnessed a smallpox outbreak in 1974 which led to the death of close to 31,000 people.
India’s vaccination drive at present:
India drastically reduced the shortage of indigenously manufactured vaccines. This led to reduced dependence on other countries for India’s Covid-19 vaccination drives.
- Increased manufacturing capability: In a single day, up to 4.3 million beneficiaries received the COVID-19 vaccines and India already administered more than 25 crores of Covid-19 doses.
- India is one of the few countries across the globe with an indigenously developed vaccine.
- Indian companies not only fulfill the domestic demand for bifurcated needles but also supplying syringes for COVID-19 vaccination to countries.
- Reduced geographical limitation: At present, India’s Covid-19 vaccination drives not focused on a particular region. Instead, citizens across the country are simultaneously getting vaccinated.
- Eliminated global-domestic time gap: India started its vaccination drives at par with the developed countries. Covishield and Covaxin, manufactured in India, have been available to the people since January 16, 2021.
COVID-19 vaccination drive demonstrates that India has become Atmanirbhar in vaccination against infectious diseases. Further, the government also decided to conduct free of cost vaccination drives. This marks a complete shift in India’s future vaccination drives.
Source: The Hindu
Read Also :-Atmanirbhar Bharat Rozgar Yojana
Issues in Vaccine Procurement Policy
Synopsis:
The recent decision of the Centre to solely procure the vaccines for the states has been welcomed by experts and healthcare professionals. However, retaining a 25% quota towards the private sector seems inappropriate and should be reconsidered.
Background:
- The union government has again taken the responsibility for procuring vaccines for the states under the liberalised vaccine policy.
- Nonetheless, experts have objected to retaining the 25% procurement quota for the private sector.
Read Also :-Issues faced by Nursing sector in India
Issues associated with 25% quota:
- First, the private sector possesses fewer vaccination centres than its approved procurement quota. This may create a demand-supply mismatch and result in inequitable distribution.
- Second, the quota is based on a mistaken assumption of an inflated ‘middle class’. The assumption is that 25% of the population is willing and able to pay for a commodity for which social benefits exceed private benefits.
- However, in reality, the affluent form only a small fraction of the uppermost 25% of our population.
- Third, markets tend to under-produce commodities having significant positive externalities. This is true for preventive measures like vaccines which have lower private demand than curative services.
- Hence, it would be very difficult to generate demand for vaccinating in private hospitals.
- Fourth, the top 25% have better access to government vaccination centres. They may choose to get free vaccination, which may have a ‘crowding out’ effect for the poorer sections.
- Fifth, it would not be possible to attain herd immunity even if 60-80% of the population gets vaccinated. As there would be the existence of grave disparities along geographic and socioeconomic lines.
Read Also :-Right to Education is set to expand its horizon
Way Forward:
- The government should increase its share of procurement by reducing the 25% quota for the private sector.
- The loss of revenue to vaccine producers from differential pricing of the private sector can be compensated by increased support through Government subsidies.
- The government should refrain from an ‘all or none approach’ towards the private sector. Where some governments often impose unreasonable and unfavorable pricing restrictions and other governments give too much freedom. There is a need for a balanced approach.
- The focus must be on creating a strategic purchasing framework that could utilize the strengths of the private sector which includes innovative processes and efficiency.
- It must engage with both small and big private players, and create a more decentralized and accountable procurement system.
Source: Click Here
Read Also :-Centre Should Relook its Vaccine Policy
Need for Equity-focused Vaccination Plan in Vaccine Drive
Synopsis:
To control the Covid-19 pandemic, India needs an equity-focused vaccination plan and a road map to provide equity and justice in vaccination.
Contents
Introduction:
According to WHO’s strategic advisory group of experts on immunisation, prioritizing socio-demographic groups is essential for universal vaccination. So, an equity-focused vaccination plan is essential for controlling the pandemic.
What is an equity-focused vaccination plan?
Instead of focussing on vaccinating the public, the plan facilitates vaccinating vulnerable sections of society. This plan should include the following sectors of people to prevent disease and death among them. Such as, prioritizing the poor, religious minorities, socially disadvantaged castes, Adivasi communities, those living in remote areas, urban slums, and women.
- For example, the Chhattisgarh government prioritised ration cardholders in vaccination.
- Under this, the Chhattisgarh government vaccinated high-risk persons such as the poor, people who live in multi-generation for the same house, larger household.
- Further, these are the people who lack access to mobile phones and the Internet (Crucial for registering vaccines).
Challenges in providing equity-focused vaccination plan
- Lack of data on various parameters: India’s Covid-19 impact data does not provide the impact of virus infection among gender, caste, religious, and indigenous identities. Though crowd-sourced data is available, they too lack geographic and other meta-data for tests conducted in India.
- Vaccination through digital registration: Digital technologies can create a digital divide among age, gender, economic dimensions, rural-urban differences. The government’s CoWIN data also shows inequitable vaccination between tribal and non-tribal areas.
- Role of developed countries: The developed countries do not always help other countries in vaccination drives. For example, During the 2009 H1N1 flu pandemic, wealthy countries secured more doses than they need to vaccinate every member of their population. Similar such behavior is also observed in the Covid-19 pandemic also. Poor countries in the world depend on the mercy of the European Union and the United States for vaccinating their population.
Read Also :-India Needs an Effective Vaccine Policy
How to improve the equity-focused vaccination plan?
- Trying out vaccination camps or door-to-door campaigns: Vulnerable sections of people often have poor access and low levels of trust in the healthcare system. So, the camps and campaigns can provide the following advantages. Such as,
- Older adults can get the vaccine from their homes.
- Essential workers will not face any interruption in their service delivery.
- Similarly, the poor and vulnerable people will not face any loss in daily wages
- The government can try women-only vaccine days to ensure that women are getting equal importance in vaccination. Women are often neglected in vaccine drive for reasons such as, they are not the breadwinner of the family, historically marginalized stature of women, etc. But this might lead to gender inequities in vaccine uptake. This will only lead to more Covid-19 infection among women
- For example, During the 1918 influenza pandemic in India, the mortality rate of women is higher than men.
- The government has to ensure vaccinating older people completely before opening vaccination to younger adults.
- In Indian villages, Accredited Social Health Activists (ASHAs) and Auxiliary Nurse-Midwives (ANMs) have enough experience and expertise with pulse polio vaccination and newborn vaccination. So, the government has to utilize its expertise to vaccinate Indian villages.
- Local governments and municipalities should prioritise vaccines for historically marginalised persons in the locality. Such as,
- Adivasi’s communities often live in remote and forested areas. The government should prioritize these regions.
- Religious minority areas such as Muslim-dominated tier-3 cities and villages should also get priority on vaccination drive.
- At the global level: WHO is consistently highlighted vaccine equity at global level. The COVAX facility can play a greater role in the equity distribution of vaccines around the world. The world leaders also need to follow the lead of WHO in vaccination and ensure global solidarity in this pandemic.
Conclusion:
The central procurement of vaccines and providing free vaccines are not alone enough to vaccinate the entire population. So, refocused rejuvenated local, national, and global vaccination campaigns alone can provide equity-focused vaccination in the world.
Read Also :-Why IITs Demand for Priority Vaccination is not Justified?
Source: The Hindu
- For example, the Chhattisgarh government prioritised ration cardholders in vaccination.
Single dose of vaccine can’t control Delta Variant: Global Study on vaccines
Contents
Synopsis:
The data from clinical trials and post-vaccination study on vaccines shows that the Dominant delta variant of Covid-19 can’t be easily controlled by a single dose of vaccine. The countries must administer two doses of vaccine and should reduce the time gap between them.
Background:
- The WHO has recently given a new classification to SARS-CoV-2 variants of interest (VOI) and variants of concern (VOC) on the basis of Greek letters. The objective was to create easy-to-pronounce and non-stigmatising labels for VOI and VOC.
- However, the established nomenclature systems for naming and tracking of SARS-CoV-2 genetic lineages by GISAID, Nextstrain and Pango will remain in use for scientific research.
- The new classification is as follows:
- VOC B.1.1.7 will be called Alpha Variant. It was the earliest documented in the United Kingdom (September 2020).
- VOC B.1.351 will be called Beta Variant. It was the earliest documented in South Africa (May 2020).
- VOC P.1 will be called Gamma Variant. It was the earliest documented in Brazil (November 2020).
- VOC B.1.617.2 will be called Delta Variant. It was the earliest documented in India (October 2020).
About the Delta Variant:
- It was first identified in Maharashtra and is believed to be responsible for the severe second wave in India.
- It has now spread to most parts of India and also been identified in many other countries.
- The rapid expansion has induced the WHO to graduate it from a “variant of interest” (VOI) to a “variant of concern” (VOC) category.
Scientists have undertaken various studies to address 3 major questions surrounding the delta VOC –
- Is it more infectious than the prevalent virus?
- Is it more lethal than the previous virus?
- Does the delta variant is more resistant to the effect of vaccines?
Data shown by various studies on vaccines:
Read Also :-What are “Variants of Concern” (VoC)?
- Results of Study conducted by Indian SARS-CoV-2 Genomic Consortia (INSACOG) and the National Centre for Disease Control (NCDC):
- The Delta variant is the “prime reason” behind the second wave, though the wave may have been initiated by the Alpha variant.
- The Delta Variant has become dominant even in Britain, where scientists have recently noted that it is 50% more infectious than the Alpha variant.
- Results of study on vaccines conducted by Public Health England:
- A single dose of the AstraZeneca vaccine provided 33% efficacy against the Delta variant, while it was 51% against the Alpha variant.
- The second dose improved the efficacy to 60% against the Delta variant and to 66% against the Alpha variant.
- Further, two doses of Pfizer-BioNtech vaccine provided much higher levels of protection than two doses of the AstraZeneca vaccine.
- Results of a British study on vaccines published in Lancet Journal:
- Merely 32%of the vaccinated individuals had adequate antibody levels against the Delta variant after the first dose of the Pfizer vaccine. It was 25% against the beta variant.
- The antibody levels rose after the second dose. However, they were far below the levels obtained against the initial variant of the Covid-19 virus.
- Results of a study on vaccines conducted by the Pasteur Institute, France:
- The Delta variant showed reduced response to both the vaccines (Pfizer and Astrazeneca). It was resistant to neutralisation by some monoclonal antibodies targeting the Spike protein.
- The study concluded that a single dose of the Astrazeneca vaccine will not display optimal protection against the delta variant.
Lessons learnt from the various study on vaccines:
- First, the Delta variant is the most infectious variant in circulation. However, there is not much convincing evidence to prove it is more deadlier than the previous variants.
- Second, vaccines have diminished efficacy against the delta variant. Further, a single dose of either the AstraZeneca or the Pfizer-BioNTech vaccine does not provide adequate protection against the Delta variant.
- Third, a shortened dosing interval is recommended to deal with the Delta variant. Britain has already reduced the interval to 8 weeks from earlier 12 weeks.
Source: The Indian Express
India’s response to shocks – 1962 war to COVID pandemic
Synopsis- The article distinguishes between the Center’s reaction to the current pandemic and its responses to shocks in Indian History.
Three criteria to analyze Indian government’s response
- The team
- The science
- The organizational innovations put together
List of previous shocks and the India’s response
- First, 1962’s Sino-India War-
- Response- Defence reform
- The new defence minister was appointed.
- The financial allocation for the defence was increased
- Alters India’s understanding of the world and foreign policy in a fundamental way.
- Response- Defence reform
- Second, 1966 Severe Drought – In 1966, due to drought, food grain production fell by 20 per cent. Foreign food aid came to the rescue of the starving population.
- Team- Indira Gandhi (PM), C Subramaniam (agriculture minister) and M S Swaminathan (scientist).
- Response-
- Start of Green Revolution.
- Science and technology were relied on and organizational innovations like the Food Corporation of India [FCI] were made.
- Third, 1975 National Emergency, political shock
- Team- Indira Gandhi (PM) and Sanjay Gandhi.
- Response-
- The harsh family planning programme was launched by PM Indira Gandhi on her son’s insistence. Despite the efforts to create awareness and support for sterilization [surgery to make a person or animal unable to produce offspring], the camps were receiving a lukewarm response.
- Fourth, 1991, External sector shock
- Team- P V Narasimha Rao (PM), Manmohan Singh (FM), M S Ahluwalia (finance secretary) and S S Tarapore (from the RBI).
- Response-
- S S Tarapore played a key role by not acceding to the capital account convertibility requirement of the IMF.
- Response to the shock, in this case, was that both policy and organizational change was brought about slowly, without disrupting the economy.
- Lastly, India’s response to the COVID-19 Pandemic
- Team- No clarity about who is in the team.
- Response-
- Not clear if the Covid-19 task force and control room in the Niti Aayog are the same.
- Mismanagement in providing information regarding Covid-19 response.
- There are some vaccine-related issues such as the gap between the two shots and taking two different vaccines. This contributes to vaccine hesitancy.
- Confusion related to vaccine procurement.
- Allowing huge gathering such as Kumbh Mela, election rallies were obvious cases of not following science.
- Few cases of which reveal the unimportance the government gives to science.
Conclusion
There is a drastic difference between the handling of COVID-19 pandemic shock from the previous shocks. The government needs to improve on all three criteria.Source- The Indian Express
NITI Aayog launches “Surakshit Hum Surakshit Tum Abhiyaan”
Contents
What is the news?
Surakshit Hum Surakshit Tum Abhiyaan’ has been launched by NITI Aayog and Piramal Foundation.
About Surakshit Hum Surakshit Tum Abhiyaan:
- Surakshit Hum Surakshit Tum Abhiyaan has been launched in 112 aspirational districts.
- Aim: To assist district administrations in providing home-care support to COVID-19 patients who are asymptomatic or have mild symptoms.
- Features of the initiative:
- Firstly, the initiative will be led by district magistrates in partnership with local NGOs.
- Secondly, the NGOs will help mobilise local volunteers. They shall be trained so that they can provide support to affected families by educating them to follow Covid-19 protocols. They shall also be trained to provide psycho-social support and timely updates about patients to the administration.
- Thirdly, local leaders, civil societies and volunteers will also work with district administrations to address emerging problems across key focus areas of the Aspirational Districts Programme.
- Significance of the campaign: The Surakshit Hum Surakshit Tum Abhiyaan campaign is expected to contribute to district preparedness for managing nearly 70% of COVID cases at home. Hence, it shall reduce pressure on the healthcare system and curbing the spread of fear among the people.
Read Also :-What is National Nutrition Mission?
About Transformation of Aspirational Districts programme (TADP):
- The TADP programme was launched in 2018. It is coordinated by Niti Aayog with support from Central Ministries and the State Governments.
- Aim: To quickly and effectively transform underdeveloped districts. This will be done by focusing on the strength of each district, identifying easily achievable areas for immediate improvement, measuring progress and then ranking them.
- Features: it is based on three broad principles:
- Convergence (of Central & State Schemes),
- Collaboration (of Central, State level ‘Prabhari’ Officers & District Collectors), and
- Competition among districts driven by a mass Movement.
- Themes: The programme focuses on 5 main themes:
- Nutrition
- Education
- Agriculture & Water Resources
- Financial Inclusion & Skill Development
- Basic Infrastructure.
- Ranking: Each district is ranked based on 49 performance indicators identified across the above 5 core themes. The main objective of the rankings is to measure progress and rank districts to spur a sense of competition among states.
Source: The Hindu
Covid-19 vaccines are safe for “inflammatory bowel disease” patients: New research
What is the News?
According to a study published in the American Journal of Gastroenterology, Pfizer or Moderna Covid-19 vaccines are safe for patients with inflammatory bowel diseases(IBD). They do not appear to have an increased risk of side effects from Covid vaccines.
About the Research:
- Researchers evaluated the post-vaccination side effects in 246 adult inflammatory bowel diseases(IBD) Covid-19 vaccine patients.
- These patients most often reported pain and swelling at the injection site after vaccination. This is followed by reasons such as fatigue, headache and dizziness, fever and chills and gastrointestinal symptoms.
- However, most of these side effects were mild and lasted only a few days.
Inflammatory bowel disease(IBD):
- Inflammatory bowel disease(IBD) represents a group of intestinal disorders that cause prolonged inflammation of the digestive tract.
- Types: The two most common IBDs are ulcerative colitis (UC) and Crohn’s disease:
- Ulcerative Colitis(UC) involves inflammation of the large intestine.
- Crohn’s disease can cause inflammation in any part of the digestive tract. However, it mostly affects the tail end of the small intestine.
- Causes of IBDs: Family history and genetics, Weak Immune System, Smoking, Ethnicity, Age and Environmental Factors among others.
- Treatment: Treatment may include immunosuppressive drugs to control the inflammation.
Source: Indian Express
“Aducanumab” approved by USFDA for “Alzheimer’s disease”
What is the News?
“Aducanumab”, a new drug for the treatment of Alzheimer’s disease, has been approved by the US Food and Drug Administration (FDA)
How does Aducanumab drug work?
- Aducanumab is a monoclonal antibody drug that aims at altering the course of Alzheimer disease by slowing the deterioration of brain function.
- Monoclonal Antibodies are man-made proteins that act like human antibodies in the immune system. They are made by cloning a unique white blood cell.
- The drug does this by reducing the presence of amyloid-beta, a protein that forms plaques in the brain.
- Significance: Since there is no treatment so far, the drug that can slow down Alzheimer’s disease holds much promise and is a ray of hope.
- Concerns:
- High Cost: The company has said that the average wholesale cost of the drug would be $56,000 (over Rs 40 lakh) per year.
- Ineffective Studies: The studies on the drug didn’t clearly show that people were likely to have fewer symptoms of Alzheimer’s disease if they were taking the drug. Hence, not all experts agreed that Aducanumab deserved approval.
About Alzheimer’s Disease:
- Alzheimer’s disease is a progressive neurologic disorder that causes the brain to shrink (atrophy) and brain cells to die.
- The disease is the most common cause of dementia — a continuous decline in thinking, behavioural and social skills that affect a person’s ability to function independently.
- Caused by: Alzheimer’s disease is thought to be caused by the abnormal build-up of proteins in and around brain cells.
- One of the proteins involved is called amyloid, deposits of which form plaques around brain cells.
- The other protein is called tau, deposits of which form tangles within brain cells.
- Vulnerability: Alzheimer disease most commonly affects older adults, but it can also affect people in their 30s or 40s.
- Cases:
- According to WHO estimates for 2017, dementia affects approximately 50 million people worldwide, a number that is projected to grow to 82 million by 2030.
- In India, it is estimated that 5.3 million people (1 in 27) above the age of 60 have dementia in 2020. This is projected to rise to 7.6 million by 2030.
Source: Indian Express
- Aducanumab is a monoclonal antibody drug that aims at altering the course of Alzheimer disease by slowing the deterioration of brain function.
How can India address its mental healthcare problem?
Synopsis: Evaluation of India’s state of mental health care and suggestions to improve them.
Background
- Recent reports published in Lancet revealed that one in seven people in India had a mental disorder ranging from mild to severe in 2017.
- Mental illnesses include anxiety disorders, psychotic disorders, mood disorders, substance use disorders, personality disorders and eating disorders.
- Despite having the necessary components to address the mental healthcare issues, more needs to be done in the context of COVID-19 that has exacerbated mental illnesses.
The mental healthcare situation in India
- The situation is bad especially in the southern states as compared to the northern states due to the nature of development, modernization, urbanization etc.,
- Sharp gender divide: Depressive disorders are more prevalent among females than males due to sexual abuse, gender discrimination, stress due to antenatal and postnatal issues etc
Contents
Why mental healthcare situation is bad in India?
- Inadequate public spending on Mental Health: India spends around 1.3% of total health expenditure on mental health, whereas, in developed countries, it ranges from 3% to 15%.
- Inadequate infrastructure for Mental Health: For Instance, the share of mental hospitals per 1,00,000 population is as low as 0.01 according to the WHO.
- Similarly, India fares poorly in the distribution of mental health units, mental health outpatient facilities, community residential facilities etc.,
- Inadequate Mental health resources: Nurses, social workers and psychologists working in the mental health sector in India are way less compared to other countries. For instance, leading countries have 222.6 psychologists per 1,00,000 population whereas India has only 0.069, per 1,00,000 population.
Why Mental Health needs to be given priority?
- One, Causative factor for suicides. The majority of suicides in the world are related to psychiatric problems or mental illnesses. India’s suicide rate was 16.3 per 1,00,000 in 2016 that is very high compared to the Global suicide rate of 10.6 per 1,00,000 population.
- Two, a significant contributor to the total disease burden in India. For instance, the proportional contribution of mental disorders to the total disease burden had doubled between 1990 and 2017.
- Three reduces longevity. According to the World Health Organization (WHO), there is a 10-25-year life expectancy reduction in patients with severe mental disorders.
Government measures on mental health care
- India has rightly enacted the following policies to cater to the needs of the population suffering from Mental illness:
- The National Mental Health Policy (NMHP) in 2014,
- Rights-based Mental Healthcare Act in 2017,
- National Adolescent Health Programme
- Ayushman Bharat
More needs to be done.
What more steps can be taken?
In order to further address mental health issues and promote mental healthcare, India needs to do the following,
- One, reduce the treatment gap for mental disorders. For instance, Telemedicine can be promoted to reduce the gap.
- Two, increase the number of personnel in the mental healthcare sector.
- Three, remove stigmatization by reducing discriminatory attitudes.
- Four, devise an integrated approach for detecting, treating, and managing patient needs.
- Five, increase counselling facilities, especially in rural areas, with special support for women through the provision of women doctors.
- Six, leverage the benefits of technology. The application of big data and crowdsourcing ideas can help to make informed decision-making.
- Seven, focus on community-based programmes. For Instance, School-based programmes on mental health can improve the mental health of children.
- Eight, create mental health awareness through traditional media, government programmes, the education system, industry, and social media.
Source: The Hindu
- Recent reports published in Lancet revealed that one in seven people in India had a mental disorder ranging from mild to severe in 2017.
Prudent Approach towards the Downward Trajectory of Second Wave
Contents
Synopsis:
India has witnessed a decline in Covid-19 cases since the last month, thereby indicating a downward trajectory of the second wave. It presents an opportunity to effectively prepare for the upcoming third wave through universal vaccination and accommodative reforms.
Background:
- The second wave of pandemic left a more brutal impact on India than the first wave, with cases touching the 4 lakh/day mark. Rural India was hurt significantly and many districts reported higher fatality rates than the national average.
- However, the cumulative Covid-19 cases have now declined by 72 % from the peak in May.
Understanding the Downward Trajectory of Second Wave:
- The decline is mainly caused by a decrease in urban cases while the rural cases are still on the rise as shown by the 14-day moving average of the top 20 districts.
- The percentage of daily new cases from rural areas is still at 52.8 percent. A high prevalence of cases in the rural area indicates that:
- The GDP loss due to the current wave will be much lower than that in the first wave. This is because these rural districts account for a lower share of economic activity.
- There is also a subtle change in India’s vaccination policy. Now India is prioritising people receiving the first dose.
- This would bring down the magnitude of serious cases in the country and ensure better preparation for the 3rd wave.
Read Also :-Measures to Control the Covid-19 Second Wave
Suggestions to capitalise the downward Trajectory of Second Wave:
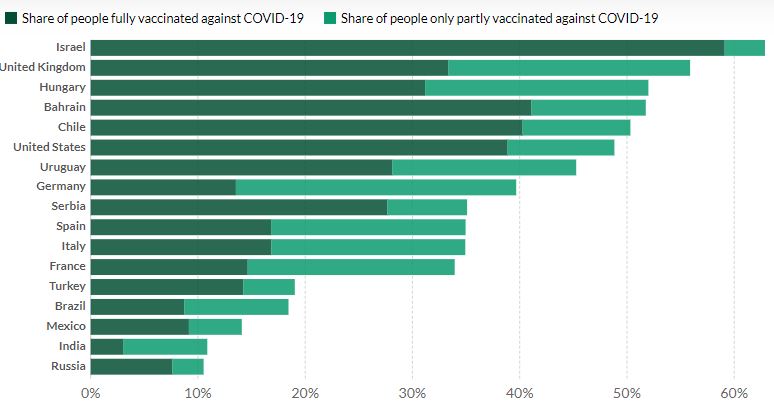
- The government should step up the vaccination drive as currently, around 16% of people have received the first dose and only 3% have been fully vaccinated. For the US, these numbers are 89.4 and 44.1 respectively.
- India must opt for an advanced procurement strategy like that adopted by developed nations to inoculate its remaining population, especially the 12-17 age bracket.
- There should be a centralised vaccine procurement along with a centralised pricing strategy.
- The rollout of a compassionate fiscal policy at both the central and state levels is also desired for reducing the stress of the common man and businesses. This would include rationalisation of fuel prices, tax holidays, electricity rebates for MSMEs etc.
- There should be prudent adoption of the best administrative practices at state and local level. The Centre should now collect and collate such systems and make them available to state governments to strengthen the health infrastructure. This includes:
- “Mumbai model” of oxygen distribution under the able administrator, Iqbal Chahal.
- “Ernakulam’s war room model” that oversees the entire city and allows for resources to be shifted swiftly between hotspots.
- Telephone-based triaging systems of Tamil Nadu and Karnataka.
- Triage systems are methods for systematic prioritizing of patients’ treatment according to how urgent they need care.
- The operations of local bodies should be digitalised to ensure better resource allocation and greater accountability.
Source: The Indian Express
Mitigating the third wave requires a focus on DOTS
Synopsis:
India is witnessing a softening of the second wave. Nonetheless, the anticipation of the 3rd wave is quite high. Therefore, it is imperative for India to focus on reducing the reproduction number (R). This in turn calls for focusing on its determinants i.e. DOTS for Mitigating the third wave
Contents
Background:
- India witnessed a brutal impact of the second wave of the pandemic in May 2021, with cases crossing the 4 lakh mark in one day.
- The situation has now eased and the number of cases has come down below the 1.5 lakh mark. The second wave appears to be abating due to a reduced reproduction number.
About Reproduction number (R):
- It refers to the average number of new infections arising from one infected individual.
- R greater than 1 implies that infected individuals infect more than one person on average, and we observe increasing cases. When it is less than 1, cases are declining.
- It is dependent on Four Factors, summarised by the acronym DOTS:
- Duration a person is infectious
- Opportunities for infected individuals to spread the infection to others;
- the probability of Transmission of infection if given an opportunity
- the average Susceptibility of a population or subpopulation
What led R to increase earlier this year resulting in a second wave?
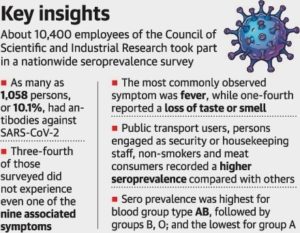
- Susceptibility: It was quite high at the start of the year. This is evident from the results from a national seroprevalence survey done in December 2020 and January 2021. They indicate roughly 25% of the population had antibodies to the virus that causes COVID-19.
- Further, less than 1% of the total population had received two doses of the vaccine till March 2021.
- Opportunity for Transmission: By January 2020, people perceived that they had won the battle over the pandemic. They were eager to get back to life and work. Eventually, this increased the social mixing and the occurrence of large gatherings that might have facilitated a second wave.
- Probability of Transmission: A fall in Covid-19 appropriate behaviour was witnessed in early 2021 like not wearing masks in public, not properly sanitizing oneself etc. Further new variants with higher transmissibility potential emerged.
- For instance, B.1.617.2 (the delta variant) is known to possess higher transmissibility potential, twice than the Covid-19 variants circulating in 2020. It has emerged as the dominant variant in India and UK during their second wave.
- Duration of infectiousness: It may have enhanced with the emergence of new variants however more research is needed on this front.
Read Also :-War against tuberculosis in India: an overview
Therefore, it is now imperative that we need to focus on DOTS for Mitigating the third wave.
Suggestions for Mitigating the third wave:
- The government must build well-designed seroprevalence surveys to understand how much of the population remains susceptible and where they reside. These should accommodate the complexities of new variants and the occurrence of reinfections.
- The focus should be on increased use of face masks and improved ventilation for reducing the transmission. The country can learn from the Bangladesh model in which the distribution of free masks coupled with community monitors delivered positive results.
- Temporary solutions like lockdowns and a ban on mass gatherings should be used to focus on slowing the transmission rate.
- The magnitude of the susceptible population can be brought down by substantially increasing the immunisation coverage. Currently, only 3% of the population has received both doses.
- The isolation and quarantining guidelines should be revised periodically as per the changing duration of infectiousness.
Source: The Hindu
Global studies on “vulnerability of animals to Covid-19”
Contents
What is the news?
A lion at Chennai’s Vandalur Zoo has died of suspected coronavirus infection. Similarly, a tiger died at Jharkhand’s Bhagwan Birsa Biological Park after suffering from fever. This sparked the debate regarding the study of the vulnerability of animals to Covid-19.
- The coronavirus initiates infection using the spike protein on its surface. On the surface of the human cell are proteins called ACE2 receptors. The spike protein binds with the ACE2 receptor, then invades the cell and goes on to replicate.
- Different species express ACE2 to different extents and this plays a key role in determining how much a species is susceptible to coronavirus infection.
Global studies on vulnerability of animals to Covid-19:
A study by PLOS Computational Biology regarding vulnerability of animals to Covid-19:
- Research: In December 2020, researchers looked at the ACE2 receptors of 10 different species and compared their affinity for binding with the virus spike protein.
- Method: The researchers used computer modelling to test this. They compared the “codon adaptation index” which is a measure of how efficiently the virus replicates after entering the cell.
- Findings: The most vulnerable species to coronavirus infection next to humans are ferrets followed by cats and civets.
Read Also :-National Climate Vulnerability Assessment Report
A study by PNAS, a research journal of US:
Researchers studied a detailed genomic analysis of the relative coronavirus risks faced by 410 species.
- Method: In humans, 25 amino acids of ACE2 are important for the virus to bind with the cell. The researchers used modelling to evaluate how many of these 25 are found in the ACE2 of other species. The more the matches with the human ACE2, the lower the risk of infection.
- Findings:
- At very high risk are primates such as chimpanzee, rhesus macaque.
- At high risk are species such as blue-eyed black lemur.
- Cats were found to have medium risk, while dogs had a low risk.
Read Also :-Reducing the vulnerabilities of urban employment
A study by the University of Bologna regarding vulnerability of animals to Covid-19:
- Researchers at the University of Bologna collected tissues from six cats and a tiger. They found wide expression of ACE2 in their gastrointestinal tracts. This was more prominent in the cats than in the tiger.
Source: Indian Express
“Revised Vaccine Procurement Policy” allows central procurement of vaccines
Contents
What is the News?
The government of India has announced a revised Vaccine Procurement Policy and also several relief measures to tackle the Covid-19 pandemic.
About Revised Vaccine Procurement Policy:
- The Central Government will go back to a system of centralised procurement of vaccines against COVID-19.
- Under this, the central government will now buy 75% of the total production of the vaccine producers and provide it to the states free of cost.
- However, the system of 25% vaccines being procured directly by the private hospitals will continue.
- State governments will monitor that only ₹150 service charge is levied by the private hospitals over the decided price of the vaccines.
Free for All Vaccine:
- Until now, the Central Government used to provide free vaccines to everyone aged 45 and above.
- However, from now on, the Centre will give free vaccines to all in the 18-44 age group starting June 21.
Extension of Pradhan Mantri Garib Kalyan Yojana:
- The government of India has announced the extension of the free ration distribution scheme for 80 crore beneficiaries under the Pradhan Mantri Garib Kalyan Yojana till November 2021.
Reasons for announcing revised Vaccine Procurement Policy
- These new announcements came after the Supreme Court had asked the Centre to file an affidavit on how the sum of ₹35,000 crores allocated in the Union Budget for vaccines has been spent so far.
- The apex court also asked why these funds cannot be used for giving free vaccination for those in the age group of 18 to 44 years.
- Moreover, the court observed that the Centre’s policy of not providing free vaccines to this particular age group was prima facie arbitrary and irrational.
Source: The Hindu
How COVID -19 can be addressed via COVID-19 appropriate behaviour?
Synopsis- Adoption of COVID-19 appropriate behaviour is the best way to reduce transmission of the Covid-19 pandemic.
Contents
Introduction-
- One of the key causes of COVID-19’s second wave in India has been the carelessness and reckless behaviour of few people. They have consistently violated Covid-19 guidelines of wearing masks and social distancing.
- According to KAP [knowledge, attitudes and practices] survey, from July 2020 to March 2021, India witnessed a 5% drop in mask-wearing.
- Relying entirely on medical science, especially treatment, is not a viable strategy for dealing with the epidemic.
Therefore, Covid-19 appropriate behaviour is a must to reduce transmission.
Read Also :–How to Prevent 3rd Wave of Covid-19?
What is behavioural science?
Behavioural science is a field of study that blends findings from social and cognitive psychology, neuroscience, and behavioural economics to make sense of human behaviour.
- With an evidence-based approach, behavioural scientists unpack what makes individuals tick: from motivations and aspirations to cognitive biases and social influences.
How behavioural science methods can be used in COVID-19 prevention?
- Create awareness about masks
- Provide basic information regarding who should wear them, when and where.
- Also, provide clarity on what types of masks are most effective, how to wear a mask correctly, and when to double mask.
- Information should be tailored accordingly to people-The government has to communicate with each group of people and provide information accordingly. But it should not discount or put down people’s beliefs or misconceptions. The government has to counter them with credible facts.
- Need to communicate the benefits of mask-wearing – The state should share testimonials, infographics and statistics that explain how masks have prevented infection transmission.
- The government can share testimonials from people who wear masks regularly and explaining how they have managed to avoid getting infected could help.
- Role model leadership – Leaders at every level should play their role in influencing people for mask-wearing and vaccinations.
- Need of responsible media–
- The media needs to maintain a high standard and report on much more than just struggling hospitals, the oxygen crisis and vaccine and drug shortages. Instead, they have to participate in fighting misinformation and disinformation.
Way forward
- People have to be aware and sensitive about COVID-19 appropriate behaviour. Till everyone will not get vaccinated, behaviour change is the most effective measure to deal with COVID-19.
- Stringent implementation of public health and social measures remain the key to stop virus transmission.
Source- The Hindu
How can India tackle the third wave of COVID?
Synopsis: To control the third wave, the decision-making on vaccines should be filled by a spirit of cooperative federalism and guided by scientists.
Introduction
Vaccines have become the focus of pandemic policy. Effective vaccine policy over the next few months will require huge efforts to boost vaccine supply. Distribution of existing supplies, helped by science, data and cooperation, can also play an important role.
What are the challenges India is likely to face?
India is going to face major vaccine shortages over the next 6-12 months. However, distributing the limited vaccine supply in a balanced, targeted way could help India save many lives and help prevent a deadly third wave.
- Vaccine supply and allocation are disordered currently. There are multiple decision-makers, rules are uncertain, messages are contradicting. Such conditions worsen the problem of a vaccine shortage.
- Challenges in continuing the current policy:
- Serious shortage in vaccine availability.
- Higher infections rates in India.
- At the end-December 2020, the third national seroprevalence survey suggested that the actual infection rate was 21.5 per cent, that is over 1 in 5 people in India had been exposed to the virus by the end-2020. Thus, a possible infection rate of over 50% or above 700 million people in June.
Advanced countries with successful vaccine programmes like Israel, the US and UK had adopted a similar strategy. They first vaccinated essential workers and then used age as parameters to decide vaccination in the initial stages.
What should India do to prevent the third wave?
Centralization of the vaccine policy is a must. Vaccines should be free for all and the costs must be borne by the Centre. However, these measures may not be sufficient in the short run.
- Focus on uninfected and vulnerable: Latest research suggests that prior infection offers protection for some time. This immunity increases strongly with at least one dose of the vaccine. This gives the government some time to focus on the uninfected and vulnerable as the immediate priority.
- Widespread testing: Vaccinating the uninfected will require detailed data on infection rates, demography and vaccination status. Widespread testing needs to be done.
- A larger share of the limited vaccines could be devoted to geographies that currently have less infection rates.
- Partial dosing or vaccine mixing could also be explored.
- Expert guidance: A technical team of scientists, epidemiologists, statisticians etc should design a plan to decide on the most effective allocation of existing vaccines.
- The team should report to a group involving the prime minister and all the chief ministers.
Decision-making on vaccines should be filled with a spirit of cooperative federalism and be guided by scientists. Trust, transparency and technical reason must guide this process.
Conclusion
The government should make efforts to increase the supply of vaccines. Once the supply of vaccines becomes sufficient, the need for allocation and prioritization will decline. Until then, it is vital to use data and science to reduce the magnitude and costs of vaccine shortagesSource: click here
Lab leak theory of Coronavirus needs credible investigation
Synopsis: The theory that Coronavirus could have been man-made from Wuhan Institute of Virology is increasing. So, adequate studies are necessary regarding the Lab leak theory of Coronavirus.
Background
- When the Covid-19 became a pandemic, China promoted the narrative that the virus had a natural origin, and it got spread from a wet market in Wuhan. This was done to avoid any scrutiny on researches being carried out in the Wuhan Institute of Virology (WIV).
- Soon, the idea of a Lab leak theory of Coronavirus was discredited as a conspiracy theory and most experts embraced the natural spread narrative.
- Even the findings of the WHO on the origins of the SARS-CoV-2 virus (coronavirus) dismissed the lab leak as “extremely unlikely”.
- However, recent developments point out the possibility that coronavirus could have originated from a lab leak, either intentionally or unintentionally.
- Recently, the U.S. President made an appeal to the U.S. intelligence community “to collect and analyse information so that, a definitive conclusion regarding the origin of the virus could be made.
- Further, the publication by Nicholas Wade, titled the origin of COVID: Did people or nature open Pandora’s box at Wuhan?” has laid out a strong case for a fuller investigation into this event.
Read Also :-India – China Informal Summit
- First, advancement in biotechnology had made it possible to genetically engineer existing pathogens to make them more lethal and difficult to treat.
- Second, in 2019, the head of corona virus-related research at WIV lab, in an interview, talked about the research carried out involving the creation of novel, life-threatening and pandemic-creating viruses.
- Third, though The WIV operates a Biosafety level-4 (BSL-4) facility, many times the deficient safety standards had been reported by U.S. inspectors but no remedial measures were taken.
- Fourth, China’s reluctance to share data, covering up facts and impeding investigation raises suspicion.
- Fifth, the findings of WHO is also being discarded on the account that the inquiry team had persons with vest interests in the WIV experimentation.
- Sixth, there are instances when Smallpox and other viruses have escaped from secured laboratories before.
Read Also :-NGT Action On Vishakapatnam Gas Leak
Suggestions
To prevent future pandemics or an event of Biowarfare, the 1972 Biological and Toxin Weapons Convention (BWC) needs to be strengthened by resolving the following drawbacks. Such as,
- The convention has no systems to verify compliance with its prohibitions. So, the global countries have to come together to build such a system
- The convention lacks enforcement mechanisms to penalize infringement of its provisions. So, the enforcement system has to be strengthened.
Source: The Hindu
Tackling pandemic in Rural India – Explained, pointwise
Contents
- 1 Introduction
- 2 Impact of the pandemic in Rural India
- 3 Need to give attention to Rural India during the Pandemic
- 4 Government Initiatives towards the betterment of Rural India during the pandemic
- 5 Challenges in vaccination and controlling the pandemic in rural India
- 6 Suggestions to tackle the pandemic in Rural India
- 7 Conclusion
Introduction
The impact of the pandemic in Rural India is quite high, especially the second wave. The positivity rate is quite high due to which India has witnessed the loss of many human lives. The situation becomes even more concerning when one looks at the dismal state of rural health infrastructure that is devoid of quality infrastructure and a sufficient number of healthcare professionals.
The time is ripe for the government to focus on rural India and rural healthcare in particular if it seriously wants to defeat the pandemic and prepare the region for future challenges. For this, a host of new measures are desired including greater devolution of funds towards rural healthcare and robust training of healthcare functionaries in the rural region.
Impact of the pandemic in Rural India
- Loss of Human Lives: The first wave didn’t reach smaller towns and hinterland regions. However, this situation was reversed in the second wave.
- Health ministry data for the last two weeks of May found that 66 percent of the districts having a test positivity rate of 10 percent or more were rural. This automatically resulted in greater deaths in these regions.
- Increasing Unemployment: Many rural people lost their jobs amongst the second wave of the Pandemic. According to the Centre for Monitoring Indian Economy (CMIE) data, the unemployment levels in rural India touched 14% in May 2021.
- Reduction in Non-Farm activities: The pandemic didn’t brutally impact the agricultural output, but it left an impact on non-agricultural activities of the rural region.
- A rise in medical expenses: The poor state of the health care system induced a heavy financial burden on the rural masses. They had to travel long distances and pay hefty fees for getting treatment facilities.
- Many non-infected people created a buffer for future medical emergencies by reducing their demand for other products.
- Psychological Stress: The first wave of the pandemic forced the migrants to travel 500-1000 km barefoot towards their homes. In the second wave, a lesser quota of vaccines was allocated to rural regions that created a feeling of being second class citizens in their own country.
- Education Divide: The pandemic enhanced the pace of digitalisation in the country. Both the teachers and students shifted towards the online medium. However, this progression enhanced the education divide in the country due to the poor availability of the internet, electricity and electronic gadgets in the rural regions.
- Prevalence of Hunger and Malnutrition: Both of them are rising in rural regions as schemes like Mid-day meal have come to a halt in many states. Further loss of income has reduced access to quality food.
Need to give attention to Rural India during the Pandemic
- Population Size: Around 65% of the population resides in rural areas. If the country wants to control the pandemic and achieve herd immunity, then adequate vaccination in rural regions is the need of the hour.
- Greater Vulnerability: The region comprises people who are not as affluent and resilient as their urban counterparts. Their ability to absorb extreme situations like a pandemic is very less due to inadequate financial cushions.
- Many in rural regions are hand to mouth workers who barely possess emergency funds of 2-4 days.
- Inadequate Health Care System: The rural health care system in India is not adequate or prepared to contain COVID-19 transmission. This can be seen more evidently in densely populated regions of northern states. As they face a shortage of doctors, hospital beds, and equipment.
- As of March 2018, there was a shortfall in health care facilities in rural regions. It was 18% at the Sub-Centre level, 22% at the PHC (Primary Health care) level and 30% at the CHC (Community Health Care) level
- Country’s Economic Revival: The rural sector provides human resources for sectors such as retail, construction, manufacturing, hospitality, education and transportation. Further, continued consumption expenditure by the rural population creates demand for multiple goods and boosts the overall economy.
- This is worrisome as India’s economy contracted by 7.3 percent in 2020-21, marking its worst performance in over four decades.
- Reducing expenditure on healthcare: Robust Rural health infrastructure will help in treating the disease at the primary level. It will help us save a lot of money and resources that are further spent at secondary and tertiary level health care.
Government Initiatives towards the betterment of Rural India during the pandemic
- The E-Sanjeevani platform provides virtual consultations to patients including patient-to-provider and provider-to-provider consultation.
- Under this a hub and spoke model was used which connected smartphone equipped rural wellness centres to specialist doctors located in cities.
- The government announced additional grains for the poor under the Pradhan Mantri Garib Kalyan Yojana.
- The Centre had allocated 73,000 crore rupees for 2021-22 for MGNREGS (Mahatma Gandhi National Rural Employment Guarantee Scheme) and notified an annual increment of about 4% in wages.
Challenges in vaccination and controlling the pandemic in rural India
- Supply of Vaccines: The supply of vaccines has been biased towards the urban centres.
- The government allowed private sales of vaccines for adults aged under 45 years, this favoured residents of cities with larger private hospital networks.
- For the first four weeks of May, nine big cities (Delhi, Mumbai, Hyderabad etc.) gave 16 % more doses than all the combined rural districts.
- Vaccine Hesitancy: It refers to delay in acceptance of vaccines or refusing vaccines despite their availability. The rate of vaccine hesitancy is higher in rural regions due to lower literacy levels.
- Infrastructure Deficit: The rural regions have a scarcity of testing services, weak surveillance system and poor medical care. This creates an impediment in taking relevant measures towards the pandemic.
- Human Resource Constraints: Many health care providers in rural areas are unregistered and untrained and do not know what to do in such an emergency.
- There is a shortfall of 81.8% specialists as compared to the requirement for existing CHCs.
- Poor Approach: The State has focused more on curative care rather than preventive care. This enhances the burden on the rural healthcare system and puts a greater economic impact on the masses in terms of higher medical bills.
- Sharing of Burden: The central government is taking lesser responsibility towards easing the situation arising from state lockdowns. Some states (such as Kerala and Tamil Nadu) have announced relief measures, but others have not done much. The latter ones are not in a position to do much because of their financial situation.
Suggestions to tackle the pandemic in Rural India
- The central government should ensure robust development of the rural health network (SHCs, PHCs and CHCs) by providing a greater amount of funds.
- The government should take active support from public-spirited citizens. For instance, Swasthya Kalyan Samitis, or SKSs were constituted for all CHCs and PHCs in haryana.
- It allowed health providers to engage with all kinds of rural community organisations (panchayats, municipal bodies, non-governmental organisations etc.) and minimise the adverse impact of the pandemic on rural life.
- Rural health networks should have access to the health data of people in their respective areas. This will enable them to identify those likely to slip into the secondary or tertiary care zone.
- There is also a need to conduct Regular health camps. It will help us to identify those on the verge of developing tuberculosis, hypertension, diabetes or any diseases owing to their socio and economic conditions.
- India can establish an independent team of experts under the aegis of the WHO. They will ensure adherence to recruitment standards, consent conditions, adverse event record management, and compensation standards.
- This will improve public confidence and provide enough data for the future policies of the government.
- The center should do the bulk purchase of vaccines rather than leaving the states at their own mercy. Further voluntary licencing of patents must be encouraged to boost the production in a lesser time and attain the goal of universal vaccination.
- The country should also adopt new methods like Remote shared medical appointments. This would allow virtual interaction of a doctor with multiple patients having similar issues, thereby saving cost and time.
Conclusion
The government should take immediate steps to control the pandemic in Rural India. They must use this as an opportunity to strengthen and improve the primary health care system in rural India, thereby preventing it from becoming the next Covid-19 hotbed.
A study on “effectiveness of vaccines” found more anti-bodies from Covishield
What is the news?
A study was conducted by the healthcare workers (HCW) in India to understand the effectiveness of vaccines in India.
About the effectiveness of vaccines:
- The study involved 515 healthcare workers from 13 states and 22 cities, 305 male of whom were male.
- These healthcare workers have been administered either of the two vaccines, Covishield and Covaxin. Further, they are chosen with or without a past history of Covid-19 infection.
Read Also :-India approves COVID-19 vaccines Covishield
Key Findings regarding the effectiveness of vaccines:
- Higher Seropositivity: Among the 515 healthcare workers, 95% showed seropositivity (higher antibodies) after two doses of both vaccines.
- Seropositivity: It refers to the presence of specific antibodies in an individual.
- Higher Antibodies: Covishield vaccine has produced more antibodies than the Covaxin doses.
- Antibody: It is a protein produced by the body’s immune system when it detects harmful substances called antigens.
- Breakthrough infections: A total of 27 breakthrough infections (4.9%) were recorded among the respondents. However, there were relatively fewer instances of ‘breakthrough infections’ after taking Covaxin than Covishield.
- Breakthrough infection: It is a case of illness in which a vaccinated individual becomes sick from the same disease for which the vaccine was administered.
- Side Effects: There were mild to moderate adverse events associated with both the vaccines, but there were no serious side effects observed during the study.
Source: The Hindu
What is the “Delta variant of Covid-19”?
Contents
What is the news?
As per a study carried out by INSACOG (the consortium of labs undertaking genome sequencing in India), Delta variant of Covid-19 is the primary cause of the second Covid-19 wave gripping the country presently.
What is the Delta Variant of Covid-19?
- The World Health Organization (WHO) has named B.1.617.1 variant as ‘Kappa‘ and B.1.617.2 variant as ‘Delta‘
- These variants are sub-lineages of B.1.617 which was detected in India in 2021.
- This new nomenclature for the various variants of the coronavirus using Greek alphabets was introduced to simplify public discussions and also help remove the stigma from the names.
- Moreover, WHO has also categorized the Delta variant as a Variant of Concern (VOC).
What is Variant of Concern (VOC)?
WHO classifies a variant as a VOC when it is associated with
- An increase in transmissibility or detrimental change in Covid-19 epidemiology or
- Increase in virulence (Ability to cause severe/life-threatening disease)
- Decrease in the effectiveness of public health measures or available diagnostics, vaccines and therapeutics.
Why is Delta Variant more dangerous than other variants?
- This variant has multiple mutations that appear to give it an advantage over other strains.
- The most important advantage is that the mutations may make the strain more transmissible.This will make the delta variant the most dangerous variant yet.
- One study indicated that the Delta variant may be up to 50% more transmissible than the B.1.1.7 (U.K./Alpha) variant.
What is a mutation?
- A mutation means a change in the genetic sequence of the virus.
- In the case of Covid-19, which is a Ribonucleic acid (RNA) virus, a mutation means a change in the sequence in which its molecules are arranged.
- A mutation in an RNA virus often happens when the virus makes a mistake while it is making copies of itself.
Source: Indian Express
- The World Health Organization (WHO) has named B.1.617.1 variant as ‘Kappa‘ and B.1.617.2 variant as ‘Delta‘
“Corbevax Vaccine” and its difference from other Covid-19 vaccines
Contents
What is the News?India has placed an advance order to block 300 million doses of a new Covid-19 vaccine, Corbevax from Hyderabad-based company Biological E.
About Corbevax Vaccine:
- Corbevax is a recombinant protein subunit vaccine. The vaccine is being indigenously produced by Biological E, Hyderabad-based Pharmaceutical company.
- Made up of: The Corbevax vaccine is made up of a specific part of SARS-CoV-2 — the spike protein on the virus’s surface.
- Administration of Vaccine: The vaccine will be administered in two doses. It is expected to be among the cheapest available in the country.
What are Spike Proteins?
- The members of the coronavirus family have sharp bumps that protrude from the surface of their outer envelopes. Those bumps are known as spike proteins.
- These spike proteins allow the virus to enter the cells in the body so that it can replicate and cause disease.
- However, in Corbevax Vaccine the spike protein alone is given to the body. So, it is not expected to be harmful as the rest of the virus is absent. The body is expected to develop an immune response against the injected spike protein.
- Therefore, when the real virus attempts to infect the body, it will already have an immune response ready that will make it unlikely for the person to fall severely ill.
Note: The technology to inject spike protein to develop immunity against a disease is not new. It has been used previously in making hepatitis B vaccines. However, Corbevax is the first vaccine made for COVID-19 to use this technology.
Different types of Covid-19 vaccines:
Vaccines are categorised on the basis of the development process adopted by scientists. For example:
- Pfizer and Moderna vaccines developed in the US are mRNA vaccines. In this type, vaccines will carry the molecular instructions to make the protein in the body through a synthetic RNA of the virus. The host body uses this to produce the viral protein that is recognized and thereby making the body mount an immune response against the disease.
- Johnson & Johnson, Sputnik V and AstraZeneca-Oxford University vaccine is a kind of viral vector vaccine. In this type, a modified version of other viruses (for example, adenovirus) is used. The virus can enter human cells but not replicate inside. A gene for the coronavirus vaccine was added into the adenovirus DNA, allowing the vaccine to target the spike proteins that SARS-CoV-2 uses to enter human cells.
- Bharat Biotech’s Covaxin and Sinovac-CoronaVac is categorised as an inactivated vaccine. In this type, an inactivated live virus is used to create an immune response against the disease.
How is the Corbevax Vaccine different from these vaccines?
- Inactivated vaccines attempt to target the entire structure of the virus.
- On the other hand, Corbevax like the mRNA and viral vector Covid-19 vaccines targets only the spike protein but in a different way.
- Viral vectors and mRNA vaccines use a code to induce our cells to make the spike proteins against which the body has to build immunity.
- On the other hand, in the case of Corbevax is actually giving the spike protein alone.
Source: Indian Express
India needs to strengthen the rural health infrastructure
Synopsis: Rural health infrastructure (SHCs, PHCs and CHCs) needs to be Modernised to cater to the health needs of the 65% of the population living in rural areas
Background
- According to info, out of 139 crore population of India, at least 91 crore people are living in 649,481 villages.
- The second wave of Covid-19 had impacted the rural community the most.
- Further, there is a growing incidence of non-communicable diseases (NCDs) such as hypertension, diabetes, cancer and cardiovascular diseases in rural India. As per WHO, NCDs cause nearly about 5.87 million (60%) of all deaths in India.
- Accordingly, there is a need to focus on strengthening the existing rural health infrastructure.
- Prioritising the development of the rural health network (SHCs, PHCs and CHCs) will help in the effective delivery of Health services to rural people.
Inadequate and poor health infrastructure in the rural areas
According to the fact shared by the Union Minister of State for Health and Family Welfare in the Rajya Sabha. India is having inadequate PHCs, CHCs, specialists, etc.
- Inadequate primary health centres (PHCs): India has only 25,743 primary health centres (PHCs) though the estimated requirement of PHC’s in rural India is 29,337. (Shortfall of 3,594 units).
- Inadequate community health centres (CHCs): Against the requirement of 7,322 CHC’s, rural India has only 5,624 community health centres (CHCs).
- Inadequate specialists in CHC’s: Data on CHCs, show that, overall, there is a shortfall of 81.8% specialists as compared to the requirement for existing CHCs.
- Inadequate infrastructure: According to the Human Development Report 2020, India has eight hospital beds for a population of 10,000 people, while China has 40 beds for the same number of people.
Significance of rural health infrastructure in effective delivery of health Services
- Rural health networks will help to treat the diseases at the primary level. Further, it will also help us save a lot of money and the resources being spent at tertiary level health care.
- For instance, if our Sub-HCs work effectively, there will be less pressure on PHCs. If the PHCs function well, then there will be minimal pressure on CHCs and so on.
- It will enable people’s participation in ensuring better functioning of rural health services.
- For example, in case of Haryana, Swasthya Kalyan Samitis, or SKSs were constituted for all CHCs, PHCs.
- It helped health providers to engage with all kinds of rural community organisations (panchayats, gram Sabha, notified area committees, municipal bodies and non-governmental organisations) in minimising the adverse impact of the pandemic on rural life.
Suggestions to improve rural health infrastructure:
- Rural health networks should have access to the health data of people in their respective areas. It will enable them to identify those likely to slip into the secondary or tertiary care zone.
- Need to conduct Regular health camps. It will help us to identify those on the verge of developing tuberculosis, hypertension, diabetes or any diseases owing to their socio and economic conditions.
- A CHC or referral centre should be modernized with effective and adequate health infrastructure. For example, A single CHC should have least 30 beds for indoor patients, operation theatre, labour room, X-ray machine, pathological laboratory, standby generators’ etc.,
WHO states that ensuring accessibility, affordability and Quality are Key to achieve Universal Health Coverage. The government should strive to provide regular and comprehensive healthcare needs in rural areas guided by the World Health Organization (WHO)’s principle of Universal Health Coverage.
Source: The Hindu
“H10N3 strain of Bird Flu” – China reports first human case
What is the News?
A man in China’s eastern province has been confirmed as the first human case of infection with the H10N3 strain of bird flu.
About H10N3 strain of Bird Flu:
- H10N3 strain of bird flu is a subtype of the Influenza A virus which is commonly known as the bird flu virus.
- The virus is normally fatal to wild birds and poultry because among animals it can be spread through respiratory droplets.
- Risk: H10N3 is a low pathogenic or relatively less severe strain of the avian flu in poultry. Its risk of spreading on a large scale is very low.
- Human-Human Transmission: There was no indication or cases of human-to-human transmission of the H10N3 virus.
- Is it a Common Virus? H10N3 is not a very common virus and only around 160 isolates of the virus were reported in the 40 years to 2018.
- However, still, flu viruses can mutate rapidly and mix with other strains circulating on farms or among migratory birds. This is known as reassortment. This reassortment can make genetic changes that pose a transmission threat to humans.
Source: The Hindu
Lessons from Naomi Osaka Episode
Synopsis:
The withdrawal of Naomi Osaka from the French Open has raised the issue of the mental well-being of the athletes. The situation exposes the deep pressure through which an athlete has to go for fulfilling its commercial obligations.
Background:
- The world number 2 tennis player (Naomi Osaka) has withdrawn from the recent French Open tournament.
- The withdrawal was on account of extreme mental stress and anxiety through which the athlete was going since the 2018 US Open tournament.
Understanding the issue:
- Naomi wrote about the compulsion to attend post-match press conferences four days before the onset of the French open tournament.
- Later, she skipped her first post-match conference and was fined $15000.
- Subsequently, a joint statement of 4 great slams threatened her with defaults and suspensions in future tournaments.
- However, this statement backfired, and she withdrew from the tournament on account of severe mental stress posed by press conferences.
Lessons from this episode:
- First, the issue of mental stress and anxiety is present in almost every sporting event.
- Second, the organizers’ insistence on media interaction may leave a deep impact on the mental well-being of an athlete.
- The media doesn’t shy away from asking personal questions for raising the TRPs in their interview. This generates higher revenues but impairs the mental health of athletes.
- Third, there are many athletes who are not as wealthy as Naomi. They are unable to quit the tournament and continue to face repeated mental stress.
- Fourth, the instance shows the existence of a disconnect between how critics and spectators interpret the sport’s nature and what it actually is. The instance has once again proved that all that glitters is not gold.
Way Forward:
- The rules pertaining to press conferences should change in an ever-evolving sport.
- The focus should be on making the process more player-friendly and nurturing a connection with journalists based on trust and empathy.
- Further, the issue presents an opportunity to augment conversation surrounding players’ mental health.
Source: Click Here
Naomi Osaka Episode and Mental health in India – Explained, pointwise
Contents
- 1 Introduction
- 2 Previous such examples of mental health issues
- 3 What is Mental illness?
- 4 India and Mental health
- 5 Challenges in improving mental health in India
- 6 Global steps to improve mental health
- 7 Indian initiatives to improve mental health
- 8 Suggestions to improve Mental health in India
- 9 Conclusion
Introduction
According to the World Health Organization (WHO) estimate, mental health illness makes about 15% of the total disease conditions around the world. Mental illness needs psychological, emotional, and social well-being initiatives to get a cure. If not treated properly, it might even lead to suicidal behaviour among the individual.
Recently, Japanese Tennis player Naomi Osaka’s decision to withdraw from the French Open citing depression put mental health issues in the spotlight once again. Earlier she issued a statement saying that she would not do press conferences at the French Open and ready to pay a fine for that. Committing to her statement, she refused to give an interview after the match. But the tennis officials issued a statement to give interview in future. The officials also mentioned that she might face expulsion from the present tournament and other Grand Slam events in case of failure to abide. Following that, she took a decision to withdraw from the current event altogether.
Emotional and mental health is more important, as it impacts the thoughts, behaviours and emotions of an individual. But mental health issues generally don’t receive much attention unless some extreme events occurred. Both the individual and the government have to take the necessary steps to improve mental health.
Previous such examples of mental health issues
- Norwegian Prime Minister diagnosed with depression in 1998. After that he revealed his illness to the public and went on medical leave for three weeks, leaving an acting Prime Minister to carry out the national duty.
- Bollywood actor Sushant Singh Rajput’s tragic death has triggered a much-needed conversation around mental health in India.
- In recent years, several celebrities open up about their mental health concerns. Such as Deepika Padukone, J.K. Rowling, Beyonce and Meghan Markle.
What is Mental illness?
Mental illnesses are health conditions involving changes in a person’s emotion, thinking, or behavior (or a combination of these). Mental illnesses are associated with distress and/or problems of functioning in social, work, or family activities. For example, people with bipolar disorder and schizophrenia are significantly disturbed, dangerous to themselves and others.
Major factors contributing to mental health problems include,
- Biological factors, such as genes or brain chemistry
- Life experiences, such as trauma or abuse
- Family history of mental health problems
India and Mental health
According to The Lancet report published in February 2020, there were 197.3 million people with mental disorders in India in 2017. The report also explains the following things,
- The top mental illnesses were depressive disorder and anxiety disorder, impacting 45.7 million and 44.9 million respectively.
- The contribution of mental health disorders to the total Disability-Adjusted Life Years (DALYs) in India increased from 2.5% in 1990 to 4.7% in 2017.
- The Southern states namely Tamil Nadu, Kerala, Telangana, Karnataka, and Andhra Pradesh accounted for a higher prevalence of mental disorders.
According to an estimate by the World Health Organization (WHO), India has one of the largest populations affected by mental health illness. So, in 2018 the WHO labelled India as the world’s ‘most depressing country’.
Challenges in improving mental health in India
- Lack of resources:
- The low proportion of mental health workforce: According to the WHO, there were 0·301 psychiatrists and 0·047 psychologists for every 100,000 patients suffering from a mental health disorder in India. This is a very low number compares to the number of mental health patients.
- Low Budgetary allocation: India is barely spending 0.5% of the health budget on the mental health sector. For example, in the recent budget only Rs 40 crore has been allocated for the National Mental Health Programme among the total health sector allocation of Rs. 2.23 lakh crore.
- Lack of awareness and sensitivity about mental health issues: This is the first and foremost reason for high mental health illness in India. Apart from that, there is also a high prevalence of social stigma and abandonment of being mentally ill in India.
- Loss to Economy: According to WHO, the burden of mental disorders is maximal in young adults. As most of the population is young, delayed or non-treatment of mentally ill persons will result in economic loss in terms of man-days.
- Treatment gap: Most of the mental healthcare facilities are located in urban areas. According to estimates, nearly 92% of the people who need mental health care and treatment do not have access to any form of mental health care.
- High out-of-pocket expenditure: The Majority of mental health issues tend to increase during economic downturns. The insurance schemes also cover only physical injuries, not mental ones. This results in high out-of-pocket expenditure during economically distress time.
- Prone to abuse: Mentally ill patients are vulnerable to and usually suffer from physical abuse, sexual abuse, wrongful confinement, etc.
Impact of Covid-19 on Mental Health
Many Surveys have indicated that the pandemic is increasing mental health problems in India.
- An integrated health care company, Practo reported a 665% jump in the number of mental health consultation.
- Further, More than two-thirds of these consultations belongs to the age of 21-40.
- Most commonly consulted mental health topics are anxiety, stress and panic attacks.
Global steps to improve mental health
- The Mental Health Atlas was launched by WHO in 2017.
- WHO Special Initiative for Mental Health: It was launched in 2019. It aims to bring attention to the high global burden of disability arising from disorders of mental health. Further, the initiative also aims to accelerate a multi-sectoral response to improve care for mental health problems.
- Target 3.4 and 3.5 of the Sustainable Development Goals talk about reducing mental health illness for the global community.
Indian initiatives to improve mental health
- National Mental Health Programme (NMHP): India launched NMHP in 1982 to improve the status of mental health in India. It has three important components. Such as Treatment of the Mentally ill, Rehabilitation and Prevention and promotion of positive mental health.
- The Mental Health Care Act (MHCA) 2017: This Act repealed the Mental Health Act, 1987. The Act seeks to ensure the rights of the person with mental illness to receive care and to live a life with dignity. Few salient provisions of the Act are,
- Central and State Mental Health Authorities: The Act established these authorities for regulation & coordination of mental health services in India.
- Right to make an Advance Directive: Under this, every person can state how to be treated or not be treated for the illness during a future mental health situation.
- Right to appoint a Nominated Representative: Every person also has the right to appoint a nominee to take, on his/her behalf, all health-related decisions.
- Changes in Section 309 of the Indian Penal Code: This section of IPC criminalized the attempt to commit suicide. After the enactment of the Act, a person who attempts to commit suicide will be presumed as a person “suffering from severe stress’’. The person will also not subject to any investigation or prosecution.
- KIRAN helpline: It is a 24/7 toll-free helpline launched by the Ministry of Social Justice and Empowerment. This helpline provides support to people facing anxiety, stress, depression, suicidal thoughts, and other mental health concerns.
- Manodarpan Initiative: It is an initiative launched by the Ministry of Education under Atmanirbhar Bharat Abhiyan. The initiative provides psychosocial support to students, family members, and teachers for their mental health and well-being during the times of Covid-19.
- RAAH app: It is a mobile application that provides free information to the public on mental health care professionals and mental healthcare centres. The National Institute of Mental Health and Neuro-Sciences(NIMHANS) has compiled a one-stop source online mental health care directory.
- MANAS App: MANAS stands for Mental Health and Normalcy Augmentation System. It is a comprehensive, scalable, and national digital wellbeing platform. It has been developed to promote the mental well-being of Indian citizens.
Suggestions to improve Mental health in India
- Increasing Awareness: The government has to increase mental health awareness and also take necessary steps to reduce social stigma. This will improve the timely undertaking of treatment.
- Increase budgetary allocation: The government has to increase the budgetary allocation to the mental health sector. The government also has to train the ground level (ASHA, ANM, AWW) workers to improve mental health among the public.
- Better coordination between Center-States: Healthcare is a state subject, so both Center and State should have better coordination
- Reducing out-of-pocket expenditure: The government has to provide financial support to reduce out of the pocket expenditure. Further, the government and private insurance policies should include mental health care in their insurance benefits.
Conclusion
According to the WHO, the countries have to act swiftly to improve mental health. Else in 2030, depression will be the leading illness globally. So, India has to take the necessary steps to improve the state of mental health. Increasing budgetary spending and creating awareness is the key to reduce mental illness.
Need of Transparency in Covid related Policies
Synopsis: Government should ensure transparency in the policies related to the Covid-19 pandemic in India. Official privacy on pandemic policies intensifies a crisis.
Introduction
The government created the National Expert Group on Vaccine Administration for COVID-19 (NEGVAC) in August 2020. It is a central agency to take decisions on all matters related to vaccine administration and rollout.
- The details of the NEGVAC’s meetings were asked under the Right to Information (RTI) Act The Health Ministry responded that it does not know where the concerned documents are.
- The information about the dates and minutes of meetings of other task forces constituted to deal with the pandemic was denied. The reason stated was “The information is not in the public domain”.
- The Memorandum of Understanding (MoU) between the ICMR and Bharat Biotech for the rollout of Covaxin was also not provided.
- Such privacy runs through the full range of COVID-19- related matters. This includes vaccine manufacturing, pricing decisions, lockdown planning and running of the ₹10,000 crore-plus PM CARES fund. The officials are keeping the pandemic and vaccine policies a secret by avoiding the RTIs.
Implications of Secrecy
- The government is denying information on important policies and decisions. Opacity serves as a cover for over-centralization and misgovernance.
- Effective planning and management cannot happen in an opaque setting. As per experts, the Covid-19 related death toll also increased because of mismanagement and lack of preparation.
- Confidentiality is reducing the ability of scientists, public health, and policy experts to give feedback and suggestions to the government. Over 900 scientists have appealed to the Prime Minister for access to information and data.
Amartya Sen wrote about famines in colonial India that mass hunger and death do not occur where information flows freely.
Way forward
- Sections 4 and 7 of the RTI Act provide for proactive and urgent disclosures where there are consequences for life and liberty.
- The Supreme Court should order the government to suo motu reveal information related to COVID-19 policies under the above provisions.
Source: click here
Twin challenge of COVID-19 Pandemic and Non-communicable diseases
Synopsis – There is a correlation between Non-Communicable Diseases [NCD] mortality rates and COVID-19 case fatalities. Government should focus on reducing the impact of Non-Communicable Diseases(NCD).
Contents
Introduction-
- Studies showed that over 70 per cent of mortalities associated with COVID are due to underlying non-communicable diseases (NCD) like diabetes, cardiovascular ailments, and cancer.
- Prevention and control of NCDs have played a crucial role in the COVID-19 response.
- For example- India’s previous efforts to minimize NCD-related deaths have resulted in lower Covid-19 case fatality rates.
- At 1.16 percent, India’s COVID case fatality rate is approximately half that of the world average of 2.17 percent.
- Every 10% reduction in the underlying NCD mortality rate results in a 20% reduction in COVID fatality rates.
What is India’s NCD strategy?
India developed a multi-sector NCD action plan to reduce the number of global premature deaths from NCDs by 25% by 2025.
Major initiatives-
- Strengthening health care system–
- Atmanirbhar Swasth Bharat scheme – The government would invest around Rs 64,000 crore in rural and urban health and wellness Centers [HWC] as part of this programme.
- Around 1,20,000 PHCs being converted into HWCs to provide primary care for NCD.
- Providing financial protection –
- PM’s health insurance scheme – The initiative covers 100 million of the most vulnerable population. It reduces out-of-pocket expenditures on health by expanding the scope of primary healthcare to include screening and diagnosis of NCD like CVD, cancer, and chronic respiratory diseases.
- To address household air pollution –
- PM Ujjwala Yojana – The use of LPG instead of polluting wood in 90 million households has reduced the risk of the chronic lung diseases and cancer that women were exposed to.
Suggestions to tackle the twin challenges of the COVID pandemic and NCD morbidities
- Ensuring universal access to screening for NCDs.
- Using Artificial Intelligence with telemedicine to continue healthcare for NCD patients during lockdown.
- Need to put focus on enhancing care policies for prevention and treatment, particularly in low- and middle-income countries to meet their UN SDGs to reduce NCD mortality by a third by 2030.
Way forward-
Achieving the SDG target by reducing one-third of premature mortalities due to NCD will make India more resilient to future viral pandemics. Thus, India must strengthen its health infrastructure through the Atmanirbhar Swasth Bharat programme.
Source- The Indian Express
Challenges of India’s COVID Diplomacy 2.0
Synopsis: India’s Covid Diplomacy 2.0 is focused on managing many challenges. The majority of these challenges arise due to Covid mismanagement.
Read– Proactive Diplomacy
Background
- During the first wave of the pandemic, India’s Covid-19 diplomacy was focused on coordinating exports of COVID-19 medicines. Further, it focussed on the repatriation of Indians from abroad under ‘Vande Bharat Mission’ and exporting vaccines worldwide under ‘Vaccine Maitri’.
- However, now, during the 2nd wave, the focus of India’s diplomacy or Covid Diplomacy 2.0 has changed due to Covid mismanagement.
- Covid mismanagement has been the reason for Vaccine shortages in India. Three factors are responsible for this,
- The failure of the Government to plan and place procurement orders in time.
- The failure of the two India-based companies to produce vaccine doses they had committed to.
- MEA’s focus on exporting, not importing, vaccines
- Owing to Covid mismanagement strategies, The Ministry of External Affairs has had to deal with many challenges.
What are the challenges facing India’s Covid Diplomacy 2.0?
- First, the most urgent task for Indian diplomats was to deal with oxygen and medicine shortages. The Ministry of External Affairs has completed the task of bringing in supplies in a timely manner, and with success.
- Second, the challenge of dealing with vaccine shortages in India.
- Currently, India is looking to the U.S. for help to manage the vaccine shortages in India. Multiple options have been worked out to boost vaccine supply with the help of the U.S.
- One, requesting the U.S. to share a substantial portion of its stockpile of AstraZeneca doses.
- Two, requesting the U.S. to release more vaccine ingredients that are restricted for exports.
- Three, to buy more stock from the three U.S. manufacturers, Pfizer, Moderna, and Johnson & Johns
- Four, to encourage the production of these vaccines in India.
- However, every option has its own challenges. For instance,
- One, The U.S. government is holding up its AstraZeneca exports until it’s own United States Food and Drug Administration approves them.
- Two, the U.S policy on releasing vaccine ingredients and components has not changed. Although it has supplied a small amount of vaccine ingredients and components.
- Three, the Production of Johnson & Johnson single-dose vaccines in India will take time.
- Four, even buying vaccines directly has its own challenges.
- The U.S. companies are seeking a waiver on the need for bridge-trials prior to clearance as well as Emergency Use Authorisation prior to supplying them that goes against India’s principles.
- Further, the U.S. manufacturers want centralised orders, with payments up-front. It will go against the center’s decision to decentralize vaccine procurement.
- Third, Indian diplomats are faced with the challenge of convincing countries for a temporary TRIPS waiver at WTO. But, since WTO works on the basis of consensus, getting a Waiver on Intellectual Property rights will be a time taking process.
- Fourth, regaining trust for India’s vaccine and pharmacy exports among neighbouring countries after the Vaccine collapse is a big challenge ahead. For instance, Bhutan was solely dependent on India for Vaccines was asked to arrange vaccines for themselves. India’s neighbors have now sought help from China and the U.S. to complete their vaccination drives.
- Fifth, understanding the pathways of emergence” of SARS-CoV2 is significant to tackle the future Covid waves.
- WHO has listed four possibilities Direct zoonotic transmission, an intermediate host, cold chain or transmission through food, or a laboratory incident.
- The fourth possibility of being a laboratory incident has gained prominence after scientists and agencies around the world are calling for more research and transparency from China.
- India is one of the largest victims of Covid19. Thus, it should seek for a more definitive answer at the global and demand accountability.
Way forward
- India should raise its voice for a stronger convention to regulate any research that could lead, by accident or design, to a pandemic.
- It is necessary to revamp the 1972 Biological Weapons Convention to institute an implementation body to assess treaty compliance and build safer standards for the future.
Source: The Hindu
Pradhan Mantri Garib Kalyan Package Insurance Scheme for health workers fighting Covid-19
Contents
What is the News?
The government of India has introduced a new system for quick clearance of claims under the “Pradhan Mantri Garib Kalyan Package(PMGKP) Insurance Scheme for health workers Fighting Covid-19”.
What is the New System for Quick Clearance of Claims?
- Under the New System, the District Collector will be certifying that the insurance claim in each case is in accordance with the guidelines of the scheme.
- On the basis of this certificate of the Collector, the Insurance Company will approve and settle the claims within a period of 48 hours.
- Further, the District Collector will also certify the claims even in the case of Central Government hospitals/ AIIMS/ Railways among others.
About Pradhan Mantri Garib Kalyan Package Insurance Scheme for health workers Fighting Covid-19:
- Launched by: It is a Central Sector Scheme launched by the Ministry of Health and Family Welfare in 2020.
- Aim: To provide comprehensive personal accident insurance cover of Rs. 50 lakh to all healthcare providers who
- Lost their life due to Covid-19
- Accidental death on account of COVID-19 related duty.
- Coverage of the Scheme:
- All government health centres, wellness centres and hospitals of Centre as well as States has included under this scheme
- Private hospital staff and retired/volunteer /local urban bodies/contracted/daily wageworker were also included in the scheme.
- Safai karamcharis, ward-boys, nurses, ASHA workers and other health workers were also covered.
- Implementation: The scheme is being implemented through an Insurance policy from the New India Assurance Company(NIACL).
Source: PIB
World Health Assembly Adopts New Resolution to End Malaria
What is the News? The 74th World Health Assembly(WHA) has adopted a new resolution to end malaria. It will accelerate efforts towards this aim.
Contents
About the Resolution to End Malaria:
- The resolution is led by the United States of America and Zambia.
- The aim of the resolution is to urge the Member States to step up progress on containing the disease. It is in line with WHO’s updated global malaria strategy and the WHO Guidelines for malaria.
- The resolution called on countries to expand investment, scale-up funding for a global response. Also, it will boost investment in the research and development of new tools.
About WHOs Global Malaria Program:
- The WHO Global Malaria Program is responsible for coordinating WHO’s global efforts to control and eliminate malaria.
- The work of the program is guided by the “Global technical strategy for malaria 2016–2030”.
Global Technical Strategy for malaria 2016–2030
- The WHO’s global technical strategy was adopted by the World Health Assembly in 2015.
- Aim: The strategy provides a technical framework for all malaria-endemic countries working towards malaria control and elimination.
- Targets: Its global targets for 2030 include:
- Reducing malaria case incidence by at least 90%.
- Reducing malaria mortality rates by at least 90%.
- Eliminating malaria in at least 35 countries.
- Preventing a resurgence of malaria in all countries that are malaria-free.
About Malaria:
- Malaria is a disease caused by Plasmodium parasites that are transmitted to people through the bites of infected female Anopheles mosquitoes.
- The disease claims more than 400,000 lives annually. In 2019, the world reported an estimated 229 million cases of malaria and 409,000 deaths.
- However, an estimated 6 million deaths and 1.5 billion cases had been averted since 2000. But the global gains in combating malaria have leveled off in recent years.
Source: Down To Earth
“World No Tobacco Day” and “Tobacco Consumption” in India
What is the News?
Every year, on 31st May, the World Health Organization (WHO) and global partners celebrate World No Tobacco Day (WNTD). This year, the WHO has honoured the health minister of India with the ‘WHO Director-General Special Recognition Award’ for his effort to control tobacco consumption in India.
About World No Tobacco Day:
- World No Tobacco Day is an annual event organised by the World Health Organisation(WHO) on May 31st.
- Objective: The day aims to raise awareness about the harmful and deadly effects of tobacco use. Thereby, discouraging the use of tobacco in any form.
- Theme: “Commit to Quit“. This theme aims to support 100 million people worldwide to give up tobacco through a range of initiatives and digital solutions.
Tobacco Consumption in India:
- Reduction in Tobacco Use: Due to the efforts of Central and State Governments, the prevalence of tobacco use has decreased by six percentage points from 34.6% in 2009-10 to 28.6% in 2016-17.
- Deaths due to Tobacco Consumption: In India, every year more than 1.3 million deaths are attributable to tobacco use. This amounts to 3500 deaths per day due to tobacco consumption.
- Risk of Covid-19: Tobacco smokers face a 40-50% higher risk of developing severe disease deaths from COVID-19.
- Economic Cost: As per the WHO report, the economic burden of diseases and deaths attributable to tobacco use in India was as high as Rs. 1.77 lakh crores. This amounts to approx 1% of Indian GDP.
Initiatives taken by India to Control Tobacco Consumption:
- Cigarettes Act,1975: The act mandated the display of statutory health warnings in advertisement and on cartons and cigarette packages.
- Cigarettes and other Tobacco Products Act(COTPA),2003: The act replaced the Cigarettes Act of 1975. It aims to provide smoke-free public places and also placed restrictions on tobacco advertising and promotion.
- Prohibition of Electronic Cigarettes Bill, 2019: It aims to prohibit the Production, Manufacture, Import, Export, Transport, Sale, Distribution, Storage and Advertisement of e-Cigarettes.
- National Health Policy 2017: It has set an ambitious target of reducing tobacco use by 30% by 2025.
- Tobacco Quit line service -1800-112-356: It was initiated in 2016 to reach a large number of tobacco users. It aims to provide telephone-based information, advice, support, and referrals for tobacco cessation.
- India has also signed the tobacco control provisions under the WHO Framework Convention on Tobacco Control (WHO FCTC).
Source: TOI
Supreme Court questions govt on its “Covid-19 vaccine policy”
What is the News?
The Supreme Court questioned the Centre on Covid-19 vaccine policy. It has also said that there needs to be a single price for vaccines across the Nation.
What was the case?
- The Supreme Court of India is hearing the suo moto case on Covid-19 issues (In Re-Distribution of Essential Services and Supplies During Pandemic).
What are the issues raised by the Supreme Court?
Vaccines Procurement:
- The Supreme Court has asked the Central Government about the procurement policy of the Covid-19 vaccines adopted by the Central Government.
- Currently, the Central Government procures just 50% of the vaccines while leaving the States to buy their own.
- Further, the court also referred to Article 1 of the Constitution that says that India, that is Bharat, is a Union of States. It said that when the Constitution says that we follow the federal rule. Then the Government of India has to procure the vaccines and distribute them to states.
Dual Pricing of Vaccines:
- The Supreme court asked the Centre on the rationale for the dual pricing of vaccines for the Centre and States.
- It said that there needs to be one price for vaccines across the Nation.
Different Criteria for Age Groups:
- The Supreme Court asked the Central Government about the rationale for giving different treatment to the age group 18-44 years as the Centre is giving free vaccines only to the 45+ age group.
- The court also pointed out that it is the 18-44 age group which got badly affected in the second wave of the Covid-19 pandemic.
Digital Divide and COWIN registration.
- The Supreme court has also raised questions about making COWIN registration mandatory for getting vaccine slots.
- The court asked the government to realise the digital divide prevailing in rural India. It said that the vaccination policy is entirely exclusionary of the rural areas.
Source: The Hindu
Jan 30 Declared World “Neglected Tropical Diseases” Day by WHA
What is the News?
The 74th World Health Assembly has declared January 30 as ‘World Neglected Tropical Diseases (NTD) Day.
Contents
About World Neglected Tropical Diseases (NTD) Day:
- The first World Neglected Tropical Diseases(NTD) Day was celebrated informally in 2020.
- UAE moved the proposal to recognize this day as ‘World NTD Day’
- Significance: World NTD Day commemorates the simultaneous launch of the first NTD road map and the London Declaration on NTDs on 30 January 2012.
About Neglected Tropical Diseases(NTD):
- Firstly, Neglected Tropical Diseases(NTD) are a group of infections. These diseases are most common in the tropical regions of Africa, Asia, and the Americas among marginalized communities. The basic reason behind them is no access to clean water or safe ways to dispose of human waste.
- Secondly, Caused by: A variety of pathogens such as viruses, bacteria, protozoa, and parasitic worms.
- Thirdly, these diseases generally receive less funding for research and treatment than diseases like tuberculosis, HIV-AIDS, and malaria.
- Fourthly, some examples of NTDs include snakebite envenomation, scabies, yaws, trachoma, Leishmaniasis, and Chagas disease.
- Cases: NTDs affect more than a billion people globally. However, the diseases are preventable and treatable.
About London Declaration:
- London Declaration on Neglected Tropical Diseases was a collaborative disease eradication program. It launched on 30 January 2012 in London.
- Based on: World Health Organization 2020 roadmap to eradicate or prevent transmission of neglected tropical diseases.
- This declaration aimed to eliminate or control 10 neglected diseases by 2020 by providing more than US$785 million to support research and development.
- Great progress has been made since 2012, but not all the goals have been met by 2020.
WHO’s New Roadmap for NTDs for 2021-30:
- The World Health Organization(WHO) has launched a new road map to
- prevent, control, eliminate and eradicate a set of 20 diseases termed neglected tropical diseases by 2030.
- Reducing the number of people in need of NTD treatment by 90%.
- Elimination of at least one NTD in more than 100 countries.
- Complete elimination of dracunculiasis (guinea worm) and yaws
- Strategy: The roadmap calls for three strategic changes in approach to end NTDs:
- From measuring process to measuring impact.
- From disease-specific planning and programming to collaborative work across sectors.
- Lastly, From externally driven agendas on programmes that are country-owned and country-financed.
Source: Down To Earth
Effects of Pandemic on Young Healthcare Workers
Synopsis: Need to give attention to the requirements of the most vulnerable members of the caregiving team i.e. young healthcare workers.
Introduction
young medical interns, postgraduates, nurses, physiotherapists, pharmacists, etc are at the lowest steps in the hierarchy of training. It seems fair from an academic view and is according to any professional training path. However, this structure is apathetic for young health care workers.
- Even before the pandemic, duty hour restrictions were not followed for young healthcare workers. Sleep-deprived postgraduates used to work for 100-hours in a week.
- There is inconsistency in stipends rates. For example, Tamil Nadu and Himachal Pradesh offer the lowest monthly stipends to first-year residents at Rs 35-37,000.
What are the adverse effects of the pandemic on young healthcare workers?
During the pandemic, most public hospitals had young interns, postgraduates, nurses, and technicians staff in fever clinics, wards, and ICUs. They were overworked by the huge volume of patients.
- Firstly, they are physically distressed by working for 8-12 hours in a stuffy PPE suit and tightly-fitted face mask. One cannot even take a toilet break.
- It requires a tremendous cognitive effort to manage complex ventilator settings and drug interactions. Especially when the patient is admitted to the Covid-19 ward with multiple co-morbidities.
- Secondly, as the second wave hit, hospitals increased their beds and ICU capacity. But the healthcare workers remained overstretched. The burden further increased by poorly-informed public health measures and an increase in public frustration and indifference.
- Thirdly, the NEET postgraduate exams this year have been delayed. The shortage of workers will continue to overburden them.
- Fourthly, the growing amount of disinformation on social media which adds to distrust against doctors and nurses has left most trainees in an unfortunate position. They are defending their worth and the firmness of scientific evidence that updates medical practice.
- They also have to defend themselves against the several instances of violence and abuse by patient attendees.
- Fifthly, all of these factors have taken a toll on the well-being of young trainees. They are away from their families and the uncertainty about their safety amidst a global pandemic affects their mental health.
- Sixthly, suicide has claimed the lives of students, interns, and postgraduates in the last year across the country. Reasons were the stress of persistent duty hours, (some even suffering from severe conditions themselves).
The conclusion
- It is time we bring an end to our indifference towards young healthcare workers. There should be some amendments to the Epidemic Disease Act to protect frontline workers from exploitation. They should be provided with centrally-sponsored insurance schemes.
- Citizens must now speak out against the exploitation of young trainees. It should be a moral responsibility to end this toxic culture that feeds off public apathy.
Source: click here
Resolving bottlenecks in procuring Pfizer’s vaccine
Synopsis – Pfizer has asked for certain conditions. They are in order to supply 5 million doses to India between July and October this year.
Introduction
- According to reports, Pfizer is ready to supply five crore doses of the mRNA vaccines [developed with the German company BioNTech] between July and October.
- However, the company has requested certain protection from the Centre. It has done this with other 116 governments across the world, including the United States.
- Therefore, to seal the deal, the pharmaceutical giant and the Indian government must quickly resolve their long-standing dispute over the protection.
Pre-conditions to supply Vaccine to India:
- Pfizer said that it will supply vaccine only to the central government, not to individual states. The company also refused to send vaccines directly to local governments citing its policy of dealing only with the Central government of various countries.
- The company has also asked for protection from the Government of India. Such as, slots for testing of their vaccines in CDL (Central Drugs Laboratory).
- The company is also requesting that it should not be liable for compensation in case of an adverse event.
What needs to be done in order to increase procurement?
- Timely vaccination is the need of the hour to protect people against the coronavirus, thus the Centre needs to take charge of all procurement and negotiations with all vaccine suppliers, including domestic and foreign.
- The government has to consider the global situation in decision-making. Such as, around 14.7 crore doses of Pfizer vaccines have already been administered worldwide without any significant reports of adverse effects.
Source-The Indian Express
Need for real-time data on public health
Synopsis: Having access to epidemiological real-time data on public health will help us to fight against the pandemic better by making informed choices.
Background
- The COVID-19 pandemic has highlighted the importance of data to governments in decision-making.
- However, India lacks real-time data on public health and the provision of health services.
- This necessitates the need for data transparency and data sharing in India to make informed decision-making.
- Hence, India needs to create a charter for standardizing digital health data.
How real-time data on public health can help fight against the Pandemic?
- Firstly, it will help in data analysis and modelling. For instance, the epidemiological concept of flattening the curve and its predictions are results of data analysis and modelling.
- Epidemiology refers to the study of medicine which deals with the incidence, distribution, and control of diseases.
- Secondly, it allows us to measure our preparedness, and shape our responses to identify, manage, and care for new cases.
- Thirdly, it will help to understand disease pathogenesis and severity. For example, Epidemic outbreak data like case data, medical and treatment data can be used to understand disease pathogenesis and severity.
- Fourthly, it helps us to understand the transmissibility or infectivity of the virus. For example, comparing genome surveillance data with the magnitude of fatalities or recovery will help us to understand the transmissibility or infectivity of the virus.
- Fifthly, it will help in predicting viral evolution and drug-treatment strategies. Surveillance through studying genome sequencing of the virus, along with epidemiological data allows us to identify the evolution of the virus after the rollout of vaccinations.
Challenges in generating real-time data on public health
- One, standardisation of data collection is the biggest challenge due to many operational constraints.
- Ensuring data availability and quality under operational constraints is critical. This can be addressed by reducing errors and enabling transparency.
- Second, concerns of privacy and security while sharing personal health data.
- There is a need to build a systemic infrastructure with built-in safeguards. This will provide security and ensure privacy.
Source: The Indian Express
Role of AYUSH during pandemic and its challenges – Explained, Pointwise
Contents
Introduction
The COVID-19 pandemic has emerged as a public health challenge. The burden of disease and mortality is steadily increasing in many parts of the country. Several social and economic factors are leading to devastating situations. Effective management to address this infection is still evolving and attempts are being made to integrate traditional interventions along with standard care.
In this regard, India is using the AYUSH system of medicine to provide relief and alleviate some symptoms of COVID-19. The AYUSH system is not seen as a cure, rather it is being used for the management of asymptomatic and mild cases of Covid-19 and for prophylactic (preventive) care. But despite that the Role of AYUSH during the pandemic is indispensable.
What is AYUSH?
- AYUSH stands for Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homoeopathy.
- These systems are based on traditional medical philosophies. They represent a way of healthy living with established concepts on prevention of diseases and promotion of health.
- In 2015, the Ministry of Ayush had also included Sowa Rigpa into the AYUSH system.
- Benefits of AYUSH system:
- It is generally cheap and affordable
- AYUSH medicines have lesser side effects than modern medicine.
- It has proven to be effective in lifestyle diseases like diabetes and hypertension
- It is used to provide healthcare in rural hinterlands where there is a shortage of allopathic doctors.
Institutional Framework for AYUSH
- The Ministry of AYUSH is at the apex. It promotes and propagates Indian systems of Medicine and Homoeopathy.
- The National Medicinal Plants Board (NMPB) coordinates activities relating to conservation, cultivation, marketing, export and policy-making for the development of the medicinal plant’s sector.
- The Central Council of Indian Medicine (CCIM) and the Central Council of Homoeopathy (CCH) are two statutory regulatory bodies. They are responsible for –
- laying down minimum standards of education,
- recommending recognition of medical qualifications,
- registering the practitioners and laying down ethical codes.
- There are five research councils that undertake officially sponsored research activities.
- The country also has eight National Institutes for teaching the AYUSH system. This includes the National Institute of Ayurveda, Jaipur; the National Institute of Siddha, Chennai etc.
- Four different Pharmacopoeia Committees work for preparing official formularies/pharmacopoeias(An official authoritative listing of drugs). They aim to evolve uniform standards in preparation for drugs in Ayurveda, Siddha, Unani and Homeopathy.
Role of AYUSH medicines used during pandemic
The role of AYUSH medicines increased significantly during the pandemic. The AYUSH medicines and techniques used during the pandemic are,
- Ayush-64: It is an Ayurvedic drug developed by the Central Council for Research in Ayurvedic Sciences(CCRAS). It is the apex body for research in Ayurveda under the Ministry of Ayush.
- The drug was originally developed in 1980 for the management of Malaria. It has now been used for Covid-19 as its ingredients showed notable antiviral, immune-modulator, and antipyretic (anti-fever) properties.
- Kabasura Kudineer: It is a Siddha medicine for the treatment of fevers. It is now being used to treat asymptomatic, mild, and moderate COVID-19 infection cases.
- It increases immunity and acts as an immune-modulator as this virus adversely affects the immune response.
- Habb-e-Bukhar: It is an Unani drug given to Covid-19 patients who are undergoing high fever.
- Arsenicum album: It is a homoeopathy drug considered correcting inflammation in the body. It takes care of diarrhoea, cough and cold.
- It is recommended for prophylactic (preventive) use against Covid-19. Further, it is also found to be useful in treating mucormycosis (fungal infection).
- Yogic Protocols: They are used in the Covid-19 treatment centres to improve respiratory and cardiac efficiency, reduce stress and anxiety and enhance immunity. Asanas like Pranayama, Shavasana etc. are extremely beneficial in this regard.
Challenges faced by AYUSH medicines and practitioners
- The tussle with Allopathic care: Many allopathic doctors don’t believe in the traditional system. They question the credibility of AYUSH practitioners and are against their inclusion into the modern health care system.
- For instance, the Indian Medical Association objected to a recent gazette notification by the Central Council of Indian Medicine (CCIM). As it allowed postgraduate Ayurvedic doctors to perform 58 basic surgeries.
- Lacks in Validation: Scientific validation of AYUSH medicines has not progressed despite dedicated government expenditure. There are very few AYUSH treatments that have been successfully validated by well-designed randomised controlled trials (RCTs).
- Poor Quality of Practitioners: The practitioners lack quality as Ayurvedic graduation and post graduation courses are often substandard and of poor quality.
- Most AYUSH institutions would have to shut down if they were subjected to the same stringent norms that MBBS medical colleges are subjected to.
- Further, due to poor economic opportunities, the AYUSH system fails to attract the country’s best talent.
- Overuse of AYUSH medicine: They are sold as over the counter products and nutraceuticals to avoid regulation. Further, Ayurvedic stores do not even have a legal requirement of a pharmacist to dispense the medications unlike pharmacies selling modern medicine. This leads to greater consumption and enhanced self-medication.
- There have been numerous cases of terminal liver failure and irreversible organ damage due to over consumption of herbal preparations.
Suggestions to improve the role of AYUSH
- Firstly, AYUSH practitioners should follow the instructions issued from time to time by the WHO, Ministry of Health & Family Welfare and Ministry of AYUSH. They should mould their advice as per the changing guidelines in order to administer proper treatment.
- Secondly, the AYUSH sanjivani app’s data must be regularly assessed and evaluated in order to include/exclude the usage of traditional medicines in tackling the pandemic.
- Sanjivani is a mobile app for impact assessment of the effectiveness, acceptance and usage of the different AYUSH advisories.
- Thirdly, the AYUSH medicines should be put through rigorous trials in order to be accepted as legitimate medications in the present times.
- Fourthly, the governments must stop treating AYUSH education and practice with an excessively liberal mindset. They should subject them to the same stringent norms and requirements expected from practitioners of modern medicine.
- Fifthly, the government should also focus on Capacity-building of licensed AYUSH practitioners through bridge training to meet India’s primary care needs.
- Sixthly, Cross-pathy between the traditional and modern systems should be allowed to fill the lacunae in respective systems. However, this must be done after due deliberation with experts from the respective systems.
- Seventhly, the government should create courses that produce qualified pharmacists trained in AYUSH pharmacopeia, who can then be placed on thousands of AYUSH stores across the country.
- Lastly, every formulation of AYUSH medicine must carry a label detailing its ingredients, side effects and other important information as is mandated for modern medicines.
Conclusion
The pandemic has made us realize that no single health care system can provide satisfactory answers to all the health needs of modern society. There is a need for an inclusive and integrated health care regime that could guide health policies and programs in the future. Medical pluralism is here to stay and the role of AYUSH sector has a critical role to play in the new and emerging situation.
WHO report on “Origin of Covid-19”: India seeks more studies on virus
Contents
What is the News?
India has welcomed the global study on the origin of Covid-19 convened by the World Health Organisation(WHO). However, India demanded initiating further studies in order to reach robust conclusions.
WHO report on Origin of Covid-19:
The report had listed “four pathways” or possible options that led to the Covid-19 pandemic:
- A direct zoonotic transmission;
- Introduction of the virus through another intermediate host or animal;
- Introduction through the cold chain or food chain;
- Laboratory incident.
What did the Global Study on the Origin of Covid-19 found?
- The study was conducted by the World Health Organisation(WHO) in association with China.
- The study has said that direct zoonotic transmission or the introduction of the virus through another intermediate host or animal are the most likely theories of the origin of Covid-19.
- Moreover, the introduction of the Covid-19 through the cold chain or food chain is also possible.
- However, the lab leak theory of the virus was “extremely unlikely”. But there was a need for further research.
India’s stand on WHO’s study:
- India has called for a comprehensive and expert-led mechanism to investigate the origin of Covid-19 in cooperation with all stakeholders.
- Further, India also demanded that the mechanism should be supported by an additional WHO mission. This mission should have the power to visit the Chinese sites for further studies.
China’s stand on WHO’s study:
- China has denied the theory that there was a leak from the Wuhan lab (research on zoonotic transmissions of coronaviruses was taking place).
Source: The Hindu
“Ayush Clinical Case Repository (ACCR) portal” and “Ayush Sanjivani App”
Contents
What is the News?
The Ministry of Ayush has launched two things. First, the Ayush Clinical Case Repository (ACCR) portal. And second, the third version of the Ayush Sanjivani App.
About Ayush Clinical Case Repository(ACCR):
- Firstly, the Ministry of Ayush has conceptualized and developed the Ayush Clinical Case Repository(ACCR) Portal. It is a platform to support both Ayush practitioners and the public.
- Secondly, Purpose: The portal aims at aggregating information about clinical outcomes achieved by Ayush practitioners on a large scale.
Significance of this Portal:
- Firstly, the portal will help the Ayush practitioners to know approaches adopted by their colleagues in the treatment of various patients.
- Secondly, the public can also go through the portal to understand the strengths of various Ayush systems in the treatment of various diseases.
- Lastly, the portal will not only benefit the Ayush practitioner and the public but will also help widen the research in the field of Ayush.
About Ayush Sanjivani app:
- Ayush Sanjivani app has been developed by the Ministry of Ayush and the Ministry of Electronics and Information Technology (MeitY).
- Purpose: The app intends to generate a significant study and data regarding the efficacy of selected Ayush interventions. The data analyzed will be helpful for the further development of Ayush Systems.
Source: PIB
“Paediatric Inflammatory Multisystem Syndrome”
Contents
What is the News?
According to a study by Lancet, the symptoms of a rare paediatric inflammatory multisystem syndrome(PIMS-TS) associated with SARS-CoV2 are resolved after six months.
About Paediatric Inflammatory Multisystem Syndrome(PIMS-TS):
- PIMS-TS is also known as a multisystem inflammatory syndrome in children (MIS-C). It is a rare condition associated with SARS-CoV-2 infection that was first defined in April 2020.
- Caused by: It is not known what triggers the condition. But it is thought to be a rare immune overreaction that occurs in children approximately four to six weeks after mild or asymptomatic SARS-CoV-2 infection.
- Symptoms: It includes fever, rash, eye infection, and gastrointestinal symptoms (e.g. diarrhoea, stomach ache, nausea). In some rare cases, the condition can lead to multi-organ failure.
- Diagnosis: Currently, MIS-C is diagnosed based on symptoms together with laboratory tests that look for signs of inflammation in the body.
- Treatment: Treatments currently include anti-coagulation to curb blood clotting, IV immunoglobulin and anti-inflammatory drugs.
About the Lancet Study:
- The Lancet study has been conducted on a small group of children affected with PIMS-TS.
- The study has found that most gastrointestinal, heart and neurological symptoms in children are resolved within six months of the COVID-19 infection.
- Moreover, the long-term damage to the organs is thought to be a rare occurrence.
Source: Indian Express
India’s Mucormycosis Threat
Synopsis: There is a high incidence of Mucormycosis in India. Government should urgently look for solutions to limit the incidence of the disease.
Background
- The incidence of mucormycosis (a rare fungal infection) in patients who have been diagnosed and treated for COVID-19 is rising alarmingly in India.
- For instance, according to a study published in Current Fungal Infection Reports the estimated burden of mucormycosis in India is 14 per 100,000. This is almost 70 times higher than what is reported in other countries.
- Even, some States, including Tamil Nadu, have declared mucormycosis as a notifiable disease under the Epidemic Diseases Act.
- Common use of Steroids such as Dexamethasone, methylprednisolone etc., in the treatment of COVID-19 is one of the major reasons for the cause of
- So, to arrest this growing epidemic, Guidelines and protocols need to be adapted and modified rapidly
About mucormycosis
- Causes:
- The most common cause is uncontrolled diabetes mellitus (raised blood sugars).
- Other causes include the treatment of some cancers, steroids, chemotherapy or immunotherapy, and solid organ or stem-cell transplantations.
- Occurrence:
- The common sites of occurrence include rhino-cerebral involvement (i.e., the fungus can damage the nose, paranasal sinuses, the eyes, and the brain), and pulmonary involvement (i.e., the fungus can cause pneumonia).
- Non-contagious:
- Mucormycosis is not transmissible from one individual to the other.
- Symptoms:
- Facial swelling on one side,
- Protrusion of the eyeball,
- New-onset visual disturbances,
- Headache and vomiting,
- New onset swelling or ulcers with blackish discolouration, and prolonged fever.
- Morbidity:
- Mucormycosis have associations with very high morbidity and mortality.
- Treatment:
- It requires a multi-disciplinary team approach that includes microbiology, pathology, radiology, and other disciplines.
- It includes Surgery along with administering of Anti-fungal drugs.
Why mucormycosis is a concern for India?
- First, one of the significant causes for mucormycosis is raised blood sugars and India is home to a large number of Diabetic patients.
- For instance, according to a study in The Lancet, people with diabetes increased to 65 million in 2016 in India,
- The highest prevalence of diabetes was observed in Tamil Nadu, Kerala, and Delhi. Further, there is an underlying higher genetic susceptibility to diabetes in Indians.
- Second, apart from this natural cause of Diabetes, SARS-CoV-2 can potentially multiply in pancreatic cells and contribute to increased blood sugar levels in COVID-19 patients.
- Third, during the treatment for Covid-19, there is administration of steroids to lower death rates by reducing the cytokine storm phase. However, steroids when used excessively or prematurely, and without medical supervision can also increase blood sugar levels.
- Fourth, treatment for mucormycosis requires a multi-disciplinary team approach. However, a multi-disciplinary approach is not feasible on a large scale, especially in areas with limited medical access
- Fifth, drugs available are either costly and out of access for the majority of Indians or produce side effects.
- For instance, the standard drug is liposomal amphotericin B. But the price is exorbitant. Whereas, cheap drugs like Amphotericin B deoxycholate have associations with unfavourable toxicity, including kidney problems.
What needs to be done?
- One, Steroid use at home for COVID-19 should be only under the supervision of a healthcare worker.
- Two, monitoring of capillary blood glucose is essential while administering steroids. Health authorities should arrange for blood glucose monitoring for patients at home on steroids.
- Further, awareness campaigns on the importance of controlled blood sugar levels need to be promoted.
- Three, widespread training of healthcare personnel including Accredited Social Health Activists (ASHAs) to raise awareness on mucormycosis while educating people locally.
Source: The Hindu
Preventive steps to avoid Mucormycosis or Black Fungus infections
What is the News?
Doctors have advised several preventive steps to be taken by Covid-19 patients to prevent Mucormycosis.
About Mucormycosis:
- Mucormycosis or Black Fungus is a rare fungal infection. A group of molds called mucormycetes is the reason behind it, which is abundant in the environment. These are present in the air, water and moist surfaces in damp places.
- Non-Transmissible: Mucormycosis is not a communicable disease. Also, it does not spread from one person to another like Covid-19.
- Vulnerable Group:
- This infection does not usually infect healthy persons. However, it can cause severe infection in an immunocompromised person.
- Moreover, it is also infecting COVID-19 patients prescribed steroids to control the infections or those who have uncontrolled diabetes.
- Types of mucormycosis: Mucormycosis can be categorised depending on the organ of the human body it attacks:
- Rhino orbital cerebral mucormycosis: It infects the nose, the orbit of the eye/eye socket, oral cavity. It can even spread to the brain.
- Pulmonary mucormycosis: This fungal infection affects the lungs and causes fever, chest pain, cough and coughing of blood.
- Gastrointestinal Mucormycosis: This fungus infection affects the gastrointestinal tract.
- Treatment: The infection is often treated with antifungal medicine, usually amphotericin B.
Preventive steps to avoid Mucormycosis:
- Firstly, patients, especially those in the high-risk category for mucormycosis should avoid visiting damp and dusty places post Covid-19 recovery.
- Secondly, it will take around four weeks for the effect of steroids administered to COVID-19 patients to wear off. So, it is important to keep oneself protected during this time.
- Thirdly, patients should wear a three-ply mask and gloves and fully cover their legs and arms.
- Fourthly, COVID-19 patients’ oxygen mask and cannula should be sterile to prevent mucormycosis.
- Fifthly, there should be a regular check on the water used in oxygenation for any possible contamination.
- Lastly, doctors and nurses should check for the symptoms in patients while treating patients with steroids or other immunosuppressive agents.
Source: The Hindu
First Case of “Yellow Fungus” detected in UP
What is the News?
A COVID-19 patient in Ghaziabad has been diagnosed with a Yellow Fungus infection.
About Yellow Fungus:
- Yellow Fungus, also goes by its second name, mucor septic. It is a fungal infection that medical experts say generally does not occur in humans but in reptiles.
- Causes:
- Poor Hygiene
- High levels of humidity beyond the 30-40% range
- Old food and improper disposal also contribute to the growth of the fungus.
- Excess use of steroids is also a possible reason in Covid-19 patients.
- Symptoms:
- Symptoms of yellow fungus are laziness, loss of appetite, or no appetite at all and weight loss.
- In serious cases, yellow fungus can also cause leakage of pus and slow healing of the open wound or necrosis in which cells in living tissue die prematurely.
- Treatment: Antifungal drug Amphotericin-B is being considered as a primary treatment of yellow fungus. The same injection is being used currently to treat black or white fungus cases in the country.
Why is Yellow Fungus more dangerous than black and White Fungus?
- Yellow fungus infections are not like black fungus infection and White Fungus infection. Instead, they are much more dangerous as it starts off internally. Thus, its diagnosis is very difficult.
- Therefore, it remains critical that patients seek help for their infection as soon as they start observing symptoms.
Source: TOI
EU leaders agree to donate 100 million doses of Covid-19 vaccines
Contents
What is the News?
The European Union(EU) countries have gathered in Brussels, Belgium for a two-day summit. During the summit the EU leaders has agreed to donate 100 million doses of Covid-19 vaccines
Key Highlights of the Summit: During the Summit:
- Firstly, the European Union leaders have committed to donate at least 100 million doses of coronavirus vaccines to middle and low-income countries before the end of 2021.
- Secondly, the EU will provide assistance to non-EU countries to help them develop local manufacturing capacity.
- Thirdly, the EU has reiterated their support for the UN-backed COVAX programme.
- COVAX program aims to ensure equitable access to COVID-19 shots for low-and middle-income countries.
- Lastly, the summit did not mention anything about lifting the intellectual property rights of Covid-19 vaccines proposed by countries like India and South Africa.
About European Union(EU):
- European Union (EU) is a political and economic union of 27 member states primarily located in Europe.
- The EU was created by the Maastricht Treaty. The treaty entered into force on November 1,1993.
- The EU has developed an internal single market through a standardised system of laws that apply in all member states.
- Five main bodies run the EU: the European Parliament, the Council of the Union, the European Commission, the Court of Justice, and the Court of Auditors.
- Among EU countries, 19 use EURO as their official currency. 8 EU members (Bulgaria, Croatia, Czech Republic, Denmark, Hungary, Poland, Romania and Sweden) do not use the euro.
- Significance: The EU was awarded the Nobel Prize for Peace in 2012, in recognition of the organization’s efforts to promote peace and democracy in Europe.
- Headquarters: Brussels, Belgium.
Source: The Hindu
“One Health High-Level Expert Panel” – A WHO panel to investigate zoonotic diseases
What is the News?
The World Health Organization(WHO) has formed a One Health High-Level Expert Panel.
About One Health High-Level Expert Panel:
- Purpose: The panel has been formed to study the emergence and spread of zoonotic diseases. Such as H5N1, avian influenza, MERS, Ebola, Zika and possibly the novel coronavirus disease(COVID-19).
- Mandate of the Panel:
- Firstly, to consider the impact of human activity on the environment and wildlife habitats.
- Secondly, to analyse the factors that lead to transmission of a disease from animal to human and vice versa
- Thirdly, to develop risk assessment and surveillance frameworks;
- Fourthly, to identify capacity gaps as well as agreement on good practices that help to prevent and prepare for zoonotic outbreaks.
- Approach: The panel will operate under the One Health Approach. This approach recognizes the links between the health of people, animals, and the environment.
- Advisory Role: The panel will advise four global agencies on how future outbreaks especially due to zoonotic diseases can be averted. These four organisations are:
- Food and Agriculture Organization of the United Nations (FAO)
- World Health Organization(WHO)
- World Organisation for Animal Health(OIE) and
- United Nations Environment Programme(UNEP).
What is One Health Approach?
- It is an approach that recognizes that the health of humans, animals, and ecosystems as interconnected one.
- Hence, it involves applying a coordinated and multidisciplinary approach at the local, regional, national and global levels. It will address potential or existing risks that originate at the animal-human ecosystems interface.
What are Zoonotic Diseases?
- Zoonosis is an infectious disease that spreads from non-human to humans.
- Zoonotic pathogens may be bacterial, viral, or parasitic. They can spread to humans through direct contact or through food, water, and the environment.
- Three of every four infectious diseases are caused by zoonosis. Moreover, scientists across the world suspect COVID-19 is also a zoonosis disease.
Source: Down To Earth
Issues in Present Policy of Vaccine Procurement
Synopsis: Analysis on issues associated with the Liberalised and Accelerated Phase 3 Strategy of COVID-19 Vaccination
Background
- Many State governments have resorted to floating global tenders for COVID-19 vaccines due to Covid vaccine shortage in India.
- The Liberalised and Accelerated Phase 3 Strategy of COVID-19 Vaccination allows states to procure COVID-19 vaccines independently of the global market for people above the age of 18 years.
- However, the Liberalised and Accelerated Phase 3 Strategy of COVID-19 Vaccination has many disadvantages.
- A single global tender for vaccine procurement through the center will be more effective in the fight against the Covid-19 pandemic.
What are the issues in the Liberalised and Accelerated Phase 3 Strategy of COVID-19 Vaccination?
- First, the Liberalised and Accelerated Phase 3 Strategy of COVID-19 Vaccination allows all persons, above 18 years of age to get COVID-19 vaccine doses.
- However, expanding eligibility in the absence of sufficient vaccine supplies will only spread vaccines thinly.
- Second, the burden to procure vaccines for the population of the 18-44 years age group has been shifted to the States. This has many disadvantages,
- One, determination of prices by an oligopolistic market favours unhealthy competition among States.
- Two, States will have to procure doses at higher rates than a single national purchaser. As a result of the new strategy, each vaccine dose will be costlier in India than in any other part of the world.
- All these issues will result in unequal distribution of vaccines among states (Vaccine inequity).
What needs to be done?
- One, government needs to revisit the vaccine policy and use the limited vaccine supply for the adult high-risk and vulnerable group of population.
- Two, vaccination for the 18-44 years age group can be reconsidered when vaccine supply is likely to stabilise.
- Three, Central government should coordinate with the States and make efforts to float a single global tender for vaccine procurement.
- The fact that the federal government has provided vaccines free to all, even in the United States, should be an eye-opener for India.
- Further, procurement of vaccines by the center and administration of vaccines by the states will ensure effective vaccine delivery. For instance, Polio.
- This mechanism of division of labour among centre-state should not be disturbed. The current vaccine strategy burdens States with additional procurement responsibilities that need to be done away with.
Article 21 of the Constitution guarantees the right to health. Right to health encompasses accessible, available, and affordable health care. Hence, it is the duty of the central government to ensure that COVID-19 vaccines are accessible, available, and affordable.
Source: The Hindu
Challenges in Vaccine Procurement in India – Explained, Pointwise
Contents
Introduction
According to the data from the Ministry of Health and Family welfare, so far, India has vaccinated only 417 million people (less than 3.1% of the population has received both doses). The population of India is 1.3 billion. If vaccines require two doses then India needs more than 2 billion doses across the nation. But neither the Covaxin nor the Covishield has that much production capacity to meet the world’s largest Covid-19 vaccination drive in India. So, India needs to do large-scale vaccine procurement to meet India’s ambition towards universal vaccination against Covid-19.
Recently India started procuring Russia’s Sputnik-V vaccine in India. Apart from that, 10 states (Rajasthan, Madhya Pradesh, Uttarakhand, Tamil Nadu, Maharashtra, Karnataka, Andhra Pradesh, Telangana, Haryana, and Delhi) decided to procure vaccines globally as there is a shortage of vaccines in India. In this article, we will explain various issues associated with vaccine procurement in India.
Present status of vaccine manufacturing in India
- Both Serum Institute of India and Bharat Biotech are providing vaccines to India in fight against Covid-19.
- The world’s largest vaccine maker, Serum Institute of India, initially promised to supply 100 million doses of vaccines a month. But in reality, it only provided between 50 million to 60 million doses.
- On the other hand, Bharat Biotech has a planned production capacity of 12.5 million a month. But their current production is somewhere between 1-5 million.
- So, India’s monthly Covid-19 vaccine manufacturing capacity is about 60-65 million doses only.
- The target of vaccination will require more than 1.5 billion doses. As Covaxin and Covishield require two doses. But the present production capacity cannot meet that amount in a short time.
- Moreover, according to the Ministry of External Affairs website, India almost exported vaccines to 95 countries in the world. As of May 11, India exported 663.698 lakh vaccine doses to foreign countries. Out of this, 16% was sent as aid, 54% as commercial supplies, and 30% as part of WHO’s COVAX program.
- So, technically the vaccine availability in India reduced further below the daily requirement of vaccines in India. For example, With only 20 million vaccine shots available for the entire month of May, many State governments have resorted to floating global tenders for COVID-19 vaccines.
- On May 1, the first consignment of the Sputnik V vaccine – 1.5 lakh doses – arrived in India. According to the health ministry’s website, the Vaccine is started administered to people recently.
Global Vaccine sources and producers
- According to the Covid-19 vaccine market dashboard, 14 vaccines are licensed or approved for emergency/conditional use. These 14 vaccine prices range from $2 to $40. So far 12.2 billion doses have been administered. The majority of them occurred in developed countries. So, to achieve a similar feat India needs to procure from global players.
Source: Our World in data
Global Vaccine manufacturers and their type of vaccines
Vaccine Manufacturer Type of Vaccine Coronavac Sinovac (China) Purified inactivated SARS-CoV-2 vaccine Sputnik-V Gamaleya Institute (Russia) Disabled Adenovirus vaccine Pfizer/BioNtech Comirnaty Pfizer/BioNtech(US) mRNA vaccine Covishield AstraZeneca/Oxford/SII Disabled Adenovirus vaccine Janssen Johnson and Jonson(US)/Merck & Co Disabled Adenovirus vaccine Convidecia Cansino Biologics(China) Disabled Adenovirus vaccine Moderna Moderna Inc(USA) mRNA vaccine - Globally developed countries hold huge stocks of Covid-19 vaccines. For example, Rich countries with 14% of the world’s population have secured 53% of the best vaccines. For example, The USA has committed stocks of 1.2 billion doses. Even though the population is around 300 million. But recently the US started to release vaccine stocks after global concerns. India can take opportunities on that and procure vaccines.
- India can negotiate with vaccine manufacturers like Moderna, Pfizer etc for procuring vaccines.
Government initiatives in vaccine procurement
- Changes in vaccination policy: The Government of India recently announced the fourth phase of its New Covid-19 vaccine policy. The policy Liberalised and Accelerated vaccine procurement. Under the new rules, the Centre will procure only 50% of vaccines produced by manufacturers. The remaining 50% can be acquired by the states directly or by private hospitals and industrial establishments at a predecided price.
- Apart from that, The Centre allowed the imported, fully ready-to-use vaccines to be entirely utilized in the other-than-Government of India channel.
- Thus, if a foreign pharma giant brings its vaccine to India, it will be free to directly sell the entire stock in the open market at a competitive price.
- Talks with global manufacturers: According to the Ministry of External Affairs, India is in touch with US entities for procurement of vaccines and manufacturing them in the country to augment vaccine supply.
- Permitting the import of the Sputnik V vaccine: The central government allowed Russia’s Sputnik-V vaccine import into India.
- Raising issues in global forums: As the Intellectual Property Rights hinder the supply of vaccines, both India and South Africa have proposed to waive off IP rights like patents, copyright, and trademarks for prevention, containment, or treatment of Covid-19. Other developing countries started to co-sponsor India and South Africa requests. The TRIPS Council also discussed this issue both formally and informally.
Challenges in Vaccine procurement
- Issues in permitting States to procure vaccines: As the central government left the states to decide the prices from foreign pharma companies, it is leading to various issues in procurement. Such as,
- Unhealthy competition among States: States will compete among each other for the limited vaccines. This will reduce cooperative federalism in India.
- Non-uniform vaccine prices and Higher cost of Vaccines: There is inexperience in States regarding international market and negotiation. Further, the States will have to procure doses at higher rates than a single national purchaser. As there is a competition of states involved. This leads to increased cost of each vaccine dose in India compares to any other part of the world. Also, the prices will essentially increase state government expenditure. For example, Recently Supreme Court noted, states are paying more – between 300 rupees to 400 rupees per dose – while the central government is paying 150 rupees.
- Detrimental to India’s image: As several states floating separate tenders to procure Covid-19 vaccines from abroad, This will be detrimental for India’s image in the world. Also, this will fracture India’s bargaining power.
- The difference in Covid-19 reduction rate among rich and poor states: Richer states will be better positioned in procuring the highest number of vaccine doses from abroad. So, they can reduce the Covid-19 caseload faster. On the other hand, Poor states might suffer more from the present and future Covid-19 waves.
- Against India’s Vaccination policy: In India, the Center procures vaccines and the States administer them. This helped India to deal with public health problems such as polio, etc. The new vaccination policy is a violation of India’s prior vaccination policies.
Challenges in distribution
- Unequal distribution of cold storage facilities among states. Even if states procure vaccines, they cannot distribute the vaccines easily. For example, out of the 28,932 cold chain points, half are in the five southern states, Maharashtra and Gujarat. Whereas the eight states in the North and Odisha that account for over 40 percent of the country’s population have only 28 percent of the cold chain points.
- The Issue of Vaccine wastage: According to the RTI information, India has wasted more than 44 lakh of 10 crore doses(Till April 11). Tamil Nadu wasted over 12 percent, followed by Haryana (9.74%), Punjab (8.12%). Ideally, a vaccination center must have 10 recipients to make optimal use of a single 10-dose vial. If the person is not available then that vaccine vial becomes a waste.
Suggestions
- Conducting a detailed demand-supply analysis: To conduct a calibrated expansion of the eligibility criteria India needs to conduct a detailed analysis including the vaccine manufacturers’ real-time production capability, the supply chain delays, etc.
- Change the vaccination policy: The Centre needs to take charge of all procurement and negotiations with all vaccine suppliers including domestic and foreign suppliers without any exception. Even the Supreme Court also raised issues in state procurement and called the central government to relook its procurement process.
- Work with domestic manufacturers to increase the supply: The Centre should seek clarity from Serum Institute of India and Bharat Biotech regarding their weekly schedule of supplies, production capacity, etc. This will help India to know the amount of vaccine shortage and plan India’s future procurements.
- Signing business deals with foreign manufacturers: India can also sign agreements with global vaccine manufacturers like Pfizer, Moderna, etc. The government can include prior purchase agreements to strike a better and lower price in vaccine procurements.
Way forward
In conclusion, the government not only needs to focus on vaccine procurement. But also has to focus on monitoring the progress of domestic and foreign vaccines, tracking adverse events of vaccination, reviewing the performance of vaccine and sharing it with people to ensure public confidence. Further, it will also make India a step closer to Universal vaccination.
Types of Vaccines: - mRNA vaccines: It is a new type of vaccine to protect against infectious diseases. It does not use the conventional model to produce an immune response. mRNA vaccine carries the molecular instructions to make the protein in the body through a synthetic RNA of the virus. The host body uses this to produce the viral protein that is recognized and thereby making the body mount an immune response against the disease.
- Adeno Virus vaccines: In this type, a modified version of adenovirus is used. The virus can enter human cells but not replicate inside. A gene for the coronavirus vaccine was added into the adenovirus DNA, allowing the vaccine to target the spike proteins that SARS-CoV-2 uses to enter human cells.
- Inactivated SARS-CoV-2 vaccine: In this type, an inactivated live virus is used to create an immune response against the disease.
“Global Health Summit 2021” adopted “Rome Declaration”
Contents
What is the News?
The Virtual Global Health Summit 2021 is being held in Rome, Italy.
About Global Health Summit 2021:
- Global Health Summit was organised by Italy in its role as president of the G20 in partnership with the European Commission.
- Purpose: The summit seeks to empower and enable stakeholders to address the challenges in the third sustainable development goal(SDG) of Health and Wellbeing for all.
Rome Declaration:
- The Rome Declaration was adopted at the Global Health Summit 2021.
- Principles: The declaration is made up of 16 mutually agreed principles. These principles aim at guiding joint action to prevent future health crises and to build a safer, fairer and more equitable and sustainable world.
Key Features of the Rome Declaration:
- Firstly, to support and enhance the existing multilateral health architecture.
- Secondly, to promote the multilateral trading system and global supply chains related to Health emergencies,
- Thirdly, to enable equitable, affordable, timely global access to high-quality, safe, effective prevention, detection and response tools.
- Fourthly, to support low and middle-income countries to build expertise and develop local and regional manufacturing capacities for tools.
- Fifthly, to facilitate data sharing, capacity building, licensing agreements among stakeholders. Further, it aims to facilitate voluntary technology and know-how transfers on mutually agreed terms.
- Sixthly, to invest in the worldwide health and care workforce
- Seventhly, to increase the effectiveness of preparedness and response measures by promoting inclusive dialogue with local communities,
- Lastly, to seek to ensure the effectiveness of financing mechanisms.
Source: WHO
” Kyasanur Forest Disease” – ICMR-NIV Develops a New Point-of-Care Testing
Contents
What is the News?
A new point-of-care test has been developed for the rapid diagnosis of Kyasanur Forest Disease (KFD).
About Point-of-Care Test:
- Firstly, the Point-of-Care Test has been developed by the Indian Council of Medical Research (ICMR)-National Institute of Virology.
- Secondly, the test kit includes a battery-operated Polymerase Chain Reaction (PCR). The analyser is portable and lightweight. The kit also has a universal cartridge-based sample pre-treatment kit and nucleic acid extraction device that aid in sample processing at the point of care.
Significance of Point of Care Test:
- The Point of Care tests would be beneficial for the diagnosis of KFD. It is because the outbreaks mainly happen in remote areas where there is a lack of well-equipped sample handling and laboratory testing facilities.
- The test kit would also be useful in quick patient management and controlling the further spread of the virus.
About Kyasanur Forest disease:
- Firstly, the Kyasanur Forest disease is caused by a Kyasanur Forest disease virus. The disease primarily affects humans and monkeys.
- Secondly, India: The disease was first identified in the Kyasanur forest of Shimoga district in Karnataka during an investigation of monkey mortalities in 1957.
- Thirdly, Symptoms: The disease is characterized by chills, frontal headache, body ache, and high fever for five to 12 days with a case fatality rate of 3 to 5%.
- Fourthly, Transmission:
- Rodents, shrews, and monkeys are common hosts for KFDV after being bitten by an infected tick.
- Transmission to humans may occur after a tick bite or contact with an infected animal, most importantly a sick or recently dead monkey.
- Fifthly, Diagnosis: Diagnosis can be made in the early stage of illness. It can be done by molecular detection by PCR or virus isolation from blood.
- Sixthly, Treatment: There is no specific treatment for KFD. A vaccine (Formalin inactivated KFDV vaccine) does exist for KFD and is used in endemic areas of India.
Source: Indian Express
Public Expenditure on Health Needs to be Reprioritised
Synopsis: Stimulating Economic growth and Mass vaccination are key to overcome the pandemic-induced economic crisis in India. Increasing public expenditure on health can help India recover from the economic crisis.
Background
- A nominal growth of 14.4% was assumed in the Union Budget. However, because of a prolonged lockdown, India will witness a fall in the nominal GDP numbers assumed in the Budget.
- A reduction in nominal GDP numbers will lead to a lowering of tax and non-tax revenues. Whereas an increase in the fiscal deficit as compared to the budgeted magnitudes.
- Hence, the fiscal projections of Centre’s 2021-22 Budget require recalibration. Further, the center needs to reprioritize expenditures.
- The allocation for the health sector should be increased substantially by reprioritizing expenditures.
Why the allocation for the health sector should be increased?
- Firstly, need to strengthen the health care infrastructure in the country.
- The second wave of the Covid19 has exposed India’s serious under-capacity in health infrastructure.
- Given the possibility of a third COVID-19 wave, there is an urgent need to increase the health and related infrastructure. Such as the number of hospitals and hospital beds, sources of oxygen supplies, and the manufacture of COVID-19 vaccines and drugs.
- Secondly, inadequate budgeting for health care.
- Centre’s 2021-22 Budget for the Department of Health and Family Welfare is ₹7,597 crore less than the 2020-21 budget for Department of Health and Family Welfare.
- The budget 2021-22 for health care is quite inadequate for an economy challenged by COVID-19 for two successive years.
- Hence, the allocation for the health sector needs to be increased substantially by reprioritising expenditures.
- Thirdly, investment in health care will have a multiplier effect on the economy. For example, Construction activities within the health sector will have high multipliers. Will benefit vulnerable groups of the society including migrant labour and the rural and urban unemployed
- Fourthly, Speedy and larger vaccination coverage of the vulnerable population is key to minimise economic damage.
Why Centre government should procure vaccines?
- One, COVID-19 vaccination is characterised by strong inter-State positive externalities. This makes it primarily the responsibility of the central government.
- Two, if the center becomes the sole agency for vaccine procurement, the economies of scale and the Centre’s bargaining power would keep the average vaccine price low.
- Three, some smaller States may find procuring vaccines through a global tender a quite challenging.
The Centre has had allocated ₹35,000 crore for vaccination as an amount to be transferred to the States. Rather than transferring the money to states, the central government should transfer the vaccines by acting as a single procurement agency for India.
Source: The Hindu
Voluntary Licensing Mechanism for Vaccines Will Ensure Social Justice
Synopsis: Other alternatives available to boost Vaccine supply are less effective. But Voluntary licensing Mechanism for Covid 19 vaccines will lead to affordable and accessible vaccines.
Contents
Background
- Affordable vaccination is the key to achieve global herd immunity and to prevent new strains of COVID-19.
- To make vaccines affordable there are multiple arrangements globally. Such as
- Voluntarily licensing: Manufacturers can place their licensing agreements for which they owned patent rights in the UN-affiliated Medicines Patent Pool.
- Compulsory licensing: Through TRIPS Waiver on Patent rights, for Covid-19 vaccines under WTO TRIPS agreement.
- COVAX Program: It was established to purchase vaccine doses and donate them to low-income countries but does not involve modifying patent rights
- WHO’s COVID-19 Technology Access Pool: a patent-sharing pool for Covid-19 products.
- However, a voluntary licensing mechanism will be more effective in achieving the target of affordable and universal vaccination. Further, it has been successfully demonstrated in making AIDS drugs more affordable.
How voluntary licensing can make medical drugs affordable?
- The case study of AIDS drugs can better explain how voluntary licensing can make medical drugs/ vaccines more affordable.
- During the 1990s, the WTO started implementing a global intellectual property regime known as the Trade-Related Aspects of Intellectual Property Rights agreement (TRIPS).
- After that, there was anti-TRIPS activism around the globe due to fear of price rise of essential medicines because of the TRIPS agreement.
- Responding to anti-TRIPS activism from low-income countries, some manufacturers who owned patent rights to produce AIDS drugs placed their licensing agreements in the UN-affiliated Medicines Patent Pool.
- This allowed Several India-based companies to use the voluntary licences to manufacture these drugs on a massive scale and sell them at prices they determine.
- This effort brought down the price of key AIDS medications in low-income countries. For instance, tenofovir, the first-line treatment for HIV/AIDS, has come down in price from $200-$500 per person per year to $39 per person per year in low-income countries.
What are the issues in other alternative mechanisms?
- First, the Voluntary licensing mechanism will reduce the cost and time taken to manufacture vaccines compared to producing vaccines through a ‘Compulsory licensing agreement’.
- Voluntary licensing enables goodwill among Patent right holding companies and general manufacturers.
- It will enable easy flow of “technology transfer” thereby reducing the cost and time taken to manufacture vaccines.
- About Compulsory licensing:
- Compulsory licenses is a mechanism to override patent rights. It allows local production or import of drugs by generic manufacturers in the event of a public health crisis.
- This right has been enshrined in the Doha Declaration addendum to the WTO’s TRIPS agreement.
- This is what India and South Africa are lobbying for in the WTO, having recently been joined by the United States.
- Second, COVAX Programme faces the issue of underfunding. Also, Similar attempts like COVAX Programme during the AIDS crisis were chronically underfunded and had only minor effects on that pandemic compared to the voluntary licensing.
- Third, the WHO’s COVID-19 Technology Access Pool too faces issues similar to COVAX Programme. For instance, no patent holders have joined this effort. This is the reason why India and South Africa called on the WTO to temporarily waive patent protections for COVID-19.
Way forward
- Patents are not absolute ownership rights. They are a temporary contract that balances the public interest with the claims of the innovator.
- Further, billions of dollars are spent through public money to develop COVID-19 vaccines.
- Considering the above facts, patent owners should enable the mass production of affordable vaccines by granting voluntary licensing for Covid-19 vaccines.
Source: The Hindu
Why IITs Demand for Priority Vaccination is not Justified?
Synopsis: IITs are demanding priority vaccination. Their demand for vaccinating their staff and students against Covid-19 on a should not be encouraged.
Background
- In a recent meeting with the Union education minister, the IIT directors have demanded for vaccinating their staff and students against Covid on a priority basis, so that they can resume classes.
Why IIT’s demands should not be encouraged?
- First, no person’s right to life is bigger than other persons. Though IITs are largely residential institutions, there are many other similar institutions. The risk of community infection is the same for all.
- Second, IITs cannot demand priority on grounds of the nature of their work. They are not a frontline sector. Also, equally, everyone’s work is essential for the functioning and well-being of the community.
- Third, to grant priority to a single interest group would open the floodgates to more such demands. With India facing a shortage of vaccines, such demands will reduce our vaccine distribution to complete chaos.
- Fourth, vaccination is not a private but a public good. Vaccination protects not only the individual receiving it but everybody around them. India can be Pandemic free only when every individual is safe from the threat of the virus.
- Fifth, it will deepen the endemic divisions of our society. For instance, distribution and administration of Covid vaccines are already heavily skewed in favour of the urban over the rural, the affluent over the poor, the digitally-enabled over the digitally-deprived. Any decision to promote subgroup interest will widen this gap further.
IITs need to employ their combined expertise and authority more effectively to guide the nation’s struggle against Covid to general benefit, thus lessening the need for sectarian demands.
Source: Indian Express
Issues and Significance of Longer Vaccine Gaps
Synopsis: Recently, the government introduced longer vaccine gaps for few reasons. But it fails to take other things into account.
Contents
Introduction:
Recently the Indian government recommended a higher interval between two doses of the Covishield vaccine. Apart from that, the government also introduced few other changes. Such as,
- Encouraging lactating women to take vaccines
- 3-month waiting period before taking vaccines for the Covid-19 recovered persons (earlier it was four to eight weeks).
- If the person gets Covid-19 infections after the first dose, s/he also needs to go through a three-month waiting period before taking the second dose of Covid-19 vaccine.
- Increasing the vaccine gap between two doses from 12-16 weeks for Covishield.
Two underlying principles behind longer vaccine gaps:
- To tackle the shortage in the vaccine:
- Prior to second-wave, the government focussed on vaccinating vulnerable sections and frontline workers.
- But during the second wave, the government allowed vaccine manufacturers to ‘free up’ vaccine supply. Under this, they can sell only 50% to Center and the rest on their own. But this policy did not improve access to all citizens.
- So, the government introduced the higher vaccine gap.
- Best timing of the second dose for an optimal boost to the immune system:
- Clinical trials of the AstraZeneca vaccine in the UK (18-55 years) showed that the binding antibodies (the ones that actually block viruses) were nearly twice high for persons who got their vaccine shots after 12 or more weeks.
- Further, the vaccine also appeared to be more protective for persons above 18 with a longer dose interval.
Challenges with longer vaccine gaps:
A general policy for childhood vaccines in India is 4 to 8-week intervals. So, the 12-16 week difference is not a general one. Further, it also has many concerns. Such as,
- Antibody levels are one of the key markers of protection. But, they are not the only ones. Cell-based immunity (immune system confers long-lived immunity) is not considered in scientific studies.
- Duration of protection: At present, there is huge uncertainty about the duration of protection given by vaccines. For example, there are many pieces of evidence that exist for breakthrough infections and Covid-19 related deaths even after the second dose of vaccination. So, only more vaccination will provide greater clarity on the degree of protection.
Way forward:
The death tolls from India’s second wave continue to surpass similar daily figures from the U.S. and Brazil. Further, the policymakers have to remember that many Indians have still not been exposed to the virus and newer threatening variants are on the line.
So the government has to aim for universal vaccination to prevent disease spread and death toll. The government has to accelerate vaccination drives and policy recommendations geared towards that goal.
Source: The Hindu
Pradhan Mantri Swasthya Suraksha Yojana
What is the News? The Government of India has approved the setting up of 22 new regional AIIMS (All India Institute of Medical Sciences) under the Pradhan Mantri Swasthya Suraksha Yojana (PMSSY) so far.
About Pradhan Mantri Swasthya Suraksha Yojana(PMSSY):
- Type: Central Sector Scheme
- Nodal Ministry: The scheme was announced in 2003 by the Ministry of Health and Family Welfare.
- Objective: To correct regional imbalances in the availability of affordable/reliable tertiary healthcare services. Moreover, It will also augment facilities for quality medical education in the country.
- Components: The scheme has two components:
- Setting up of new AIIMS-like Institutions and
- Up-gradation of existing Government Medical Colleges /Institutions in a phased manner.
Total AIIMS established: Total of 22 new AIIMS have been announced so far under this component:-
- 6 AIIMS are already functional at Bhopal, Bhubaneswar, Jodhpur, Patna, Raipur, and Rishikesh.
- 16 more AIIMS are approved by the Cabinet. Among them, 7 AIIMS, have started OPD facility and MBBS classes while in 5 AIIMS only MBBS classes have started.
Significance of the Scheme:
- Setting up new AIIMS would not only transform health education and training. It will also address the shortfall of health care professionals in the region.
- Further, their contribution becomes significant because they will serve areas where the health infrastructure is weak.
Source: PIB
What is “White Fungus” and How Dangerous is it?
What is the News? New Cases of White Fungus from Covid-19 patients have been reported in states such as Bihar and others.
About White Fungus:
- White Fungus is also known as Candidiasis. It is a type of fungal infection caused by a yeast (a type of fungus) called Candida.
- Candida normally lives on the skin and inside the body in places such as the mouth, throat, gut without causing any problems.
- However, candida can cause infections if it grows out of control or if it enters deep into the body (for example, the bloodstream or internal organs like the kidney, heart, or brain).
- Symptoms: Symptoms of white fungus vary depending on the area affected. Most infections result in minimal complications such as redness, itching, and discomfort. However, complications may be severe or even fatal if left untreated in certain populations.
- Vulnerable Group: People with low immunity, pre-existing medical issues, people with diabetes, and people on or using steroids are at a high risk of contracting the infection.
- COVID-19 patients on oxygen support can inhale these fungal spores if their ventilators and oxygen support equipment is not sanitised properly.
- Risk is also increased by overuse of steroids and usage of tap water in the humidifier of oxygen cylinders.
- Prevention:
- Patients who are on oxygen or ventilators should be taken care of in terms of hygiene.
- The tubes and equipment should be thoroughly cleaned. Only sterilized water should be used in oxygen cylinder humidifiers.
- Treatment: It is not life-threatening. The treatment of White Fungus disease is mainly done through antifungal medicines. However, this changes if a person contracts severe disease and lungs are infected.
Read about – Black Fungus
Source: Indian Express
Biomedical Waste Management during pandemic – Explained, Pointwise
Contents
Introduction
Prior to the pandemic, India’s biomedical waste management capacity was already limited. Now, with the advent of the pandemic, biomedical waste generation has increased manifold. CPCB has given guidelines to discard the biomedical waste generated in Covid-19 camps and Covid-related material such as gloves and masks in households. However, the implementation of the guidelines is limited as local bodies are not equipped to handle biomedical waste, and even the public doesn’t have enough knowledge about segregating it. All this is leading to the piling up of biomedical waste.
According to the environment ministry, nearly 146 tonnes of biomedical waste is generated per day in the country due to diagnostic activities and treatment of Covid-19 patients. Since India is fighting with the second wave of Covid-19 and still producing and using numerous masks, Personal Protection Equipments, etc. the medical waste generation is going to increase further. So, India needs practical solutions to tackle this silent menace created by the pandemic.
Biomedical waste generation during the pandemic
- According to the Indian Medical Association (IMA), the quantity of Biomedical wastes generated per day in the country has almost doubled from 7.22 lakh kg in pre-Covid times to nearly 14 lakh kg now. This rise in waste generation is directly related to the number of Covid-19 cases in the country.
- The IMA also noted that the per-bed Biomedical waste generation was 250 grams per day before the pandemic. But today, per-bed Biomedical waste generation is around 400 grams per day.
- The majority of biomedical waste generated during the pandemic is related to Covid-19 treatment. Such as personal protective equipment (PPE), gloves, face masks, head cover, plastic coverall, hazmat suit, syringes, and other medical equipment used by both healthcare providers and patients.
- According to scientists, these biomedical wastes will take thousands of years to biodegrade. During the process, they will also release tonnes of microplastics into our environment.
To tackle this menace the CPCB even launched a COVID19BWM App to track biomedical waste.
What is biomedical waste?
In simple terms, it means any waste generated during diagnosis, treatment, or immunization of human beings or animals or in research activities. Management of biomedical waste is an integral part of infection control and hygiene programs. Without proper treatment, these medical wastes can create an adverse impact on the environment and public health.
Only about 10% – 25% of BMW is hazardous, and the remaining 75%–95% is non-hazardous. So, the segregation of biomedical waste is the key to its management.
Biomedical waste management rules in India
In July 1998 the government of India notified the biomedical waste management rules. There was modification of rules in 2000, 2003, and 2011. But the 2011 medical waste management rules remained as a draft due to a lack of consensus on categorization and standards.
After the consensus and standardization, the Indian government released Biomedical Waste Management rules in 2016. The salient features of this rule are,
- Expansion of the ambit: The scope of the rules have been expanded to include various health camps such as vaccination camps, blood donation camps, and surgical camps
- Role of State governments: The State Government has to provide land for setting up a common biomedical waste treatment and disposal facility (CBMWTF). Apart from that, the State government will also have to set up a district-level committee (This committee shall submit its report to the State Pollution Control Board every 6 months).
- Segregation: Biomedical waste has been classified into 4 categories instead of the earlier 10 categories. This is to improve the segregation of waste at the source.
- Yellow – This includes post-operated body parts, caps, masks, pathological wastes, bedding, placenta, plaster of Paris, etc
- Red – This includes syringe, IV Sets, catheters, gloves, urine bags, blood bags, dialysis kits, etc
- White – This category contains waste sharps including needles, syringes, etc.
- Blue – This category contains glassware and metallic body implants
- Role of health care facilities: The health care facilities have a larger role in medical waste management. Such as,
- Compulsory pretreatment of the laboratory, microbiological waste, and blood bags before disposal
- Phasing out chlorinated plastic bags, gloves, blood bags, etc
- Maintaining a registry of biomedical wastes generated in their facility and updating them daily.
Biomedical waste management practice in India
- The management of Biomedical wastes begins at the bedside of the patient. The hospitals categorize, segregate, pre-treat, and dispose of the medical waste in different containers.
- As per the 2016 rules, these wastes have to be treated and disposed of by Common Bio-medical Waste Treatment and Disposal Facility (CBWTF).
- In case, there is no CBWTF within the reach of a healthcare facility, then such healthcare facility should install a captive treatment and disposal facility.
According to the government data, India had 200 authorized CBWTFs in 28 States in 2020 for the environmentally safe disposal of biomedical waste. The remaining states do not have such facilities.
As per official government data for 2018, India generated 608 tonnes per day of Bio-medical Waste. Of that, 528 tonnes of waste was treated and disposed of properly. So, every day there are few tonnes of biomedical waste that went untreated. The impact of Covid-19 also affects the waste handling capacity of CBWTF and captive treatment centers.
Effects of biomedical waste in India
Pollution and health hazards are the two important impacts of medical wastes.
Pollution due to biomedical waste
- Land Pollution: If not treated and dumped into landfills then there is a high chance for heavy metals like cadmium, lead, mercury, etc. get released. Further, there is a chance these metals get absorbed by plants and can then enter the food chain also.
- Air Pollution: Pathogens present in the waste can enter and remain in the air for a long period in the form of spores or pathogens. As the Covid-19 spread through the air, improper treating/not treating it might lead to a new wave of Covid-19.
- Radioactive pollution: Hospitals are increasingly using radioactive isotopes for diagnostic and therapeutic applications. The main radioisotopes used in hospitals are technetium-99m (Tc-99m), Iodine-131(I-131), etc. This radioactive material can come from research laboratories, ICUs in liquid form. These have carcinogenic properties.
Health hazards due to biomedical waste
- Spread of infectious diseases: According to the WHO study, improper waste management is one of the major causes of an increase in infectious diseases globally. This is why the Covid-19 pandemic wastes require proper treatment.
- Operational health hazards: Improper handling of biomedical waste might lead to Injuries from sharps and exposure to harmful radioactive wastes. This will create issues for nurses, emergency medical personnel, sanitary workers.
- Increase antimicrobial resistance (AMR): The biomedical wastes aggravate the problem of AMR. Ever since the pandemic, the use of biocides (sanitizers, disinfectants, and antibiotics) increased manifold. If there is no proper treatment of biocides then the AMR will increase rapidly.
Suggestions to improve biomedical waste management
- Improving the sustainability of the health care sector: The government has to move beyond monitoring and enforcement. Instead, the government has to invest along with the health service providers to scale up the proper treatment of biomedical waste.
- Equipping Municipalities and Panchayats: The government has to provide training to ground-level workers to segregate biomedical wastes. Further, the government can even allot sufficient funds through central funding from National Rural Health Mission (NRHM).
- Stringent actions against defaulters: The ill-operated health care facilities and CBWTFs have to be strictly punished. The government can even initiate the Extended Producer Responsibility (EPR) for producers of biomedical equipment.
- Trigger Innovation: The government can incentivise start-ups and Small and Medium Enterprises (SMEs) that offer solutions for waste segregation and treatment.
- Awareness campaigns for waste segregation in households: Due to home quarantine and home treatment many individuals do not use yellow and red color bags for segregating their medical wastes. So, during the supply of medicine, the health officials have to create awareness about waste segregation. They should also provide garbage bags(Red and Yellow) along with their medicines.
Conclusion
With the opening-up of vaccination for all above 18 years, the volume of infectious waste generated from the vaccination clinics will increase manifold. So, the government has to ensure proper awareness regarding waste segregation, and creation of proper facilities to treat the medical waste in India.
Government Advisory on Aerosol and Droplet Transmission of Covid-19
What is the News?
The government of India has issued an updated general advisory on Covid-19. It has warned that the SARS-CoV-2 virus can be transported through Droplets as well as in the form of Aerosols. It can infect people up to 10 meters away.
Covid-19 Transmission: The different modes of transmission of the Covid-19 virus has been the subject of intense discussion since the start of the pandemic.
Droplets Transmission: Initially, the suggestion was that the virus spreads predominantly through Droplets.
- Droplets are large mucus or saliva particles heavier than air that fall toward the ground as soon as they’re expelled.
- Droplet transmission typically occurs when a droplet containing a virus comes in contact with another person’s eyes, nose, or mouth.
- These droplets, because of their large size, travel only short distances before falling on the ground. A person 6 feet (2 meters) away is considered safe from infection.
Aerosol Transmission: Recently, scientists have been finding increasing evidence of the Covid virus traveling through aerosols as well:
- An aerosol is a suspension of fine solid particles or liquid droplets in the air.
- Aerosols can be natural or anthropogenic. Examples of natural aerosols are fog or mist, dust, forest exudates, and geyser steam. Examples of anthropogenic aerosols are particulate air pollutants and smoke.
- Since aerosols are relatively light. They can carry the virus to much larger distances up to ten meters.
- Moreover, aerosols can remain suspended in the air for several minutes or even hours. Thereby it greatly increases the chance of infecting a nearby person.
Government Advisory:
- The Government advisory asks people to keep their indoor spaces well-ventilated by keeping doors and windows open and using exhaust systems.
- It stresses that the infection transmission risk was much lower in outdoor areas since there is easy dispersion of virus particles.
- Moreover, it advises introducing outdoor air in offices, homes, and larger public spaces and measures to improve ventilation in these spaces. Advisory is the same for both urban and rural areas to curtail the spread of the disease.
Source: The Hindu
India Needs an Effective Vaccine Policy
Synopsis: The surge in Covid-19 cases coupled with a limited supply of vaccines warrants the adoption of an effective vaccine policy by the country. The policy should prioritize groups, address hesitancy and formulate a more equitable distribution plan.
Background:
- The second wave of Covid-19 has shown that the virus is not going away in a short time. It may strike the country multiple times in the coming years.
- In this scenario, the best possible way is to vaccinate the population in order to build effective immunity against the virus and reduce the death tolls. However, there are multiple concerns that demand changes to make vaccination policy effective.
Concerns regarding vaccine policy:
- Limited Supply of Vaccines: The country is facing a shortage of vaccines due to production constraints and import resistances.
- Technicalities of vaccine production make it likely that indigenous manufacturers will require 3 to 6 months to increase capacity significantly.
- For instance, the novel mRNA vaccine candidate (HGCO19) can’t be developed by Gennova Biopharmaceuticals Ltd. without support from HDT Biotech corporation, U.S.
- Similarly, the enhancement of the import of vaccines can take place only after August 2021. It is when wealthy nations would have made substantial progress in the immunization of their populations.
- Technicalities of vaccine production make it likely that indigenous manufacturers will require 3 to 6 months to increase capacity significantly.
- Vaccine Hesitancy: People are showing unwillingness to vaccinate themselves as they doubt the efficacy of vaccines.
- One of the reasons is the halt in the use of the AstraZeneca vaccine (Covishield) by some countries due to concerns over blood clots, etc. It contributed to doubts about the safety of vaccines in India.
- Target Groups: The limited supply has created a challenge of choosing amongst the multiple groups for vaccination. India needs to choose between the most vulnerable (elders, comorbidities patients) and the most valuable (working population). The former will reduce the death toll and the latter would be more beneficial for economic revival.
- Distribution Concerns: The current policy has allowed vaccination for all adults however it does not tell the order of distribution.
- The state governments are now compelled to bear all the costs of vaccination. This may give an advantage to wealthier states over poor states.
- Further, it allows market forces to decide on vaccine access for a substantial part of the population and calls for using technology (Co win portal) to get vaccinated.
- This has allowed the least vulnerable to get vaccinated early as they possess more resources.
Way Forward:
- The central government should pioneer in both – enhancing the supply and formulating a policy to ensure equitable access to vaccines.
- It should avoid transferring expenses to State governments and shouldn’t allow the private sector to decide vaccine access.
- The country should take the help of behavioral scientists to combat vaccine hesitancy and ensure that the population is vaccinated.
- The target groups must be selected on the basis of vulnerability. However, if this is impractical, then some combination of the vulnerable and working population should be chosen. This should be worked out using data and the basis of the decision should be made public.
Source: The Hindu
“Black Fungus” or Mucormycosis Declared an Epidemic by Rajasthan
What is the News?
The Rajasthan government has declared Mucormycosis or black fungus as an epidemic and a notifiable disease.
What is Mucormycosis?
- Firstly, Mucormycosis or Black Fungus is a rare fungal infection. A group of molds called mucormycetes is the reason behind it, which is abundant in the environment.
- Secondly, Transmission: It occurs through inhalation, inoculation, or ingestion of fungal spores from the environment. However, it does not spread between people or between people and animals.
- Thirdly, Symptoms: Mucormycosis can affect different parts of the body, with different sets of symptoms. Some common symptoms are face numbness, nose obstructions on one side, swelling in the eyes, or pain.
- Fourthly, Vulnerable People: It mainly affects people who have health problems or take medicines that lower the body’s ability to fight germs and sickness.
- Fifthly, Treatment: The infection is often treated with antifungal medicine, usually amphotericin B. However, the patients may eventually require surgery.
What is Epidemic, Pandemic, and Endemic?
- Epidemic is a disease that affects a large number of people within a community, population, or region.
- Pandemic is an epidemic that’s spread over multiple countries or continents.
- Endemic is something that belongs to a particular people or country.
What is Notifiable Disease?
- Notifiable Disease is any disease that the law requires to report to government authorities.
- This will allow authorities to gather information to monitor the disease, and provides early warning of possible outbreaks.
- The process will also help the government to keep track and formulate a plan for elimination and control. In less infectious conditions, it improves information about the burden and distribution of disease.
- The Government of India has notified several diseases as Notifiable such as cholera, diphtheria, encephalitis, leprosy, meningitis, pertussis (whooping cough), plague, tuberculosis, AIDS, hepatitis, measles among others.
Source: The Hindu
Measures to Prevent Future Waves of Pandemic Disaster
Synopsis: India needs to enhance its surveillance system, vaccinate its population, and reprioritise healthcare services. It will prevent future waves of pandemics.
What measures should be taken to prevent future waves of pandemic disaster?
- First, we need inputs of a strong surveillance system to identify or predict future waves. Identifying upcoming waves is very important in mitigating a catastrophe. The current disaster is mainly because of our failure to predict waves due to unreliable testing and under-reporting of cases and deaths. Hence, we need to improve on the following,
- The Central and State government should use real-time data by encouraging reliable reporting and initiating standardised definitions.
- There is a needs to strengthen review mechanisms. It will detect the outbreak in the initial stages and extinguish it before the pandemic spreads to other areas.
- Simultaneously, genomic sequencing in real-time in the fixed proportion of samples needs to be prioritized. It will identify the Mutant variants causing outbreaks.
- Second, ramping up vaccination manufacturing to ensure universal vaccination for all not only in India but globally. India has a proven capacity to scale up testing facilities within a short period of time. Thus,
- The Central government should invite foreign manufacturing firms to collaborate with Indian firms under the ‘Make in India’ Programme’.
- Fast-tracking the manufacture of all vaccines that has been approved for use by various regulatory authorities through a single-window clearance.
- Third, since 2009, WHO had declared six public health emergencies of international concern. India cannot always rely on reactive systems for each pandemic. Hence, India needs to plan for preventing and managing pandemics in the future. Future plan should focus on,
- Nearly 60% of known infectious diseases and up to 75% of new or emerging infectious diseases are zoonotic in origin. Adopting the ‘One Health’ agenda can prevent future pandemics. Because it ensures that environmental health and animal health are given similar priority as human health.
- Greater financial allocations, increasing vaccination capacity, applied research, enhancing effective communication, and monitoring effectiveness will strengthen India’s role in the future for preventing and managing pandemics.
- Finally, need to build a robust public health workforce to provide efficient public health responses.
- Front-line workers play an indispensable part in surveillance, contract-tracing, and mobilising people for primary healthcare services, including vaccination. Hence, we need to ensure that one Accredited Social Health Activist (ASHA) worker is hired for every 1,000 people. Further, an Auxiliary Nurse Midwife (ANM) and nurse practitioner are hired for every 5,000 people.
- To provide access to critical care capacity for all, we need to ensure at least one hospital with 100 beds. It should include beds with emergency and critical care services that caters to a population of 30,000-50,000.
Source: The Hindu
- First, we need inputs of a strong surveillance system to identify or predict future waves. Identifying upcoming waves is very important in mitigating a catastrophe. The current disaster is mainly because of our failure to predict waves due to unreliable testing and under-reporting of cases and deaths. Hence, we need to improve on the following,
Role of ICMR in Facilitating Evidence-based Treatment
Synopsis: ICMR must assess evidence and provide specific recommendation on treatment. An Evidence-based Treatment will build public trust in the health care system.
Background
- Drugs and therapies are being used for the Covid-19 treatment, without clear evidence. For instance, convalescent plasma therapy (CPT), Hydroxychloroquine, and the anti-parasitic drug, ivermectin.
- Evidence-based ICMR guidelines can control this issue effectively.
The case for non-evidence-based treatment: The Use of convalescent plasma therapy (CPT)
- Last year, the ICMR, based on its clinical trial results, demonstrated that CPT neither saves lives nor improves the patient’s condition. However, ICMR was ineffective in informing the public about the issue. This led to the widespread use of CPT in many states.
- In a recent statement, the ICMR recommended that the use of CPT is advisable only in early moderate disease, or within seven days of symptoms.
- Finally, in its latest guidelines, The Indian Council of Medical Research (ICMR) has finally dropped its recommendation on use of convalescent plasma therapy (CPT) as treatment for moderate COVID-19.
- This comes after the results published by The Lancet. It found no effect of the use of CPT.
- Further, evidence is emerging that CPT may be contributing to the evolution of coronavirus mutations.
What needs to be done?
- Not only CPT, but many drugs such as Hydroxychloroquine and ivermectin also, continue to find a place for the treatment of mild disease. It is also despite a specific mention of “low certainty of evidence.
- So, to avoid such situations in feature, the ICMR task force has to qualitatively assess evidence and be very specific with its recommendations.
- Further, ICMR should publicize these guidelines at regular intervals to educate the public about the evolving nature of the treatment.
- This will work better towards easing the pressure on doctors as well as in improving trust in systems
Source: The Hindu
Brain drain in the health sector – Explained, Pointwise
Contents
Introduction
India is facing a health emergency due to Covid-19 Pandemic. At present, India is registering a little less than 3 lakh cases and more than 4,000 deaths in a day. Now, India is also undertaking one of the largest vaccination programs in the world. Management of this huge task would not have been possible without the contribution of health workers. The contribution of Indian health care workers amid the pandemic is extremely commendable.
However, India is facing a shortage of health workers at this crucial point in time. The present workforce is overburdened with their work for more than a year. A part of this problem is due to a large-scale brain drain in the health sector. If India was able to retain its workforce, India’s health sector would have been in a better position now.
Status of brain drain in the health sector in India
As per government reports, India has 1.7 nurses per 1,000 population and a doctor to patient ratio of 1:1404. But both of these are well below the WHO norms. The WHO recommends three nurses per 1,000 population and a doctor to patient ratio of 1:1100. The distribution of doctors and nurses is also heavily skewed in favour of some regions. Higher concentration present in some urban pockets. Brain drain in the health sector is also the reason for this.
- For several decades, India has been a major exporter of healthcare workers to developed nations. Indian health care workers are highly prevalent in the Gulf Cooperation Council (GCC) countries, Europe, and other English-speaking countries.
- As per OECD data, around 69,000 Indian-trained doctors and 56,000 Indian-trained nurses worked in the UK, US, Canada, and Australia in 2017.
- There is also a large-scale migration of health workers from India to the GCC countries. But there is no credible data available.
- The British Association of Physicians of Indian Origin (BAPIO) estimates that the UK alone has more than 40,000 Indian doctors.
According to the FICCI, The UK and the US are the top two destinations for foreign-trained doctors. Canada and Australia are other preferred destinations. Many developed and Gulf countries provide the red carpet for the best Indian doctors and nurses. India on the other hand not only facing challenges in retaining health professionals and also facing huge demand and supply gap in Doctors, nurses in rural areas.
Reasons for brain drain in the health sector
Like any migration trends, the migration of health professionals also has both push and pull factors.
Push factors
- Low Wages: Developed countries offer better wages compare to India. For example, nurses in India receive low wages in private sector outfits. Also, they have only less opportunity in the public sector(Low employment due to lower hospitals in the public sector). So, they generally migrate to developed countries that offer better wages.
- Lack of government investment in health care: India’s health care investment to GDP ratio is just 1.2 per cent. This is the lowest figure if we compare spending by OECD and BRICS nations. This reduces better employment opportunities for health professionals.
- Lack of health care educational Institutions: India only has around 550 institutions for MBBS education. So, Many Indian students prefer to study abroad due to high course fees, limited seats in government medical colleges, etc. Once they study abroad they prefer to pursue higher studies or practice abroad alone. China is attracting a lot of Indian students in this regard.
- Other factors: This includes unethical practices of some Indian private hospitals, lack of government policy to protect the vulnerable is also a reason for a health care worker to move abroad.
Pull factors
- Access to advanced technology: Developed countries offer better opportunities to pursue research in health care. Health care professionals also get access to advance technology, research facilities and even get higher scholarship amounts for their research.
- Better standard of living and life quality: Many developed and GCCs offer a higher salary, tax benefits, higher standard of living, etc. These act as a pull factor for Indian health care professionals.
- Policies of developed countries: Developed countries adopted migrant-friendly policies towards health care professionals. For example, with the onset of the pandemic, there is a greater demand for healthcare workers across the world. The developed countries implemented various policies to retain health care employees. Such as,
- OECD countries exempted travel bans for the health professionals with job offers.
- Some countries processed visa applications of healthcare workers even during the lockdown period.
- The UK has granted free one-year visa extensions to healthcare workers and their dependents
- France has offered citizenship to frontline immigrant healthcare workers during the pandemic.
Government measures to tackle the brain drain in the health sector
The government introduced many schemes to retain the brain drain in the health sector. For example,
- Stopped issuing NORI certificates: In 2014, India stopped issuing No Objection to Return to India (NORI) certificates to doctors migrating to the US. The US government requires a NORI certificate for doctors who seek to extend their stay beyond three years. As India stopped issuing these certificates, the Indian doctors will have to return to India after three years.
- Inclusion of nurses in the Emigration Check Required (ECR) category: This policy requires nurses recruitment from other countries to be done only through the six state-related employment agencies. Further, this also makes it mandatory for the nurses to accept international contracts that are approved by the government. This increases the transparency in nursing recruitment and reduces the exploitation of nurses in the destination countries.
But these policies fail to stop the brain drain from India and not focus on the long-term prevention of brain drain.
Suggestions to reduce brain drain in the health sector
National level practices:
- Adequate investment in the health sector: Indian Budget 2021 aims to increase the Health sector spending from 1.2 percent to 2.5 percent in three years. This will increase adequate health infrastructure, adequate employment opportunities, etc.
- Creating adequate health care institutions: The government has to allow private medical educational institutes to open up medical colleges along with capping the maximum fee per seat. Further, the government can ease land requirement norms for medical and nursing colleges and ease the teachers per students ratio for post-graduate medical courses.
- Bringing in cutting-edge technology labs: The government has to create more cutting-edge research facilities to bring back health care professionals to India. For example, About 20 NRI doctors from the US and Europe relocated to Kolkata to set up the West bank Hospital as it has high-tech equipment and facilities.
- The government also has to regulate any unethical practices, exploitation of nurses in private hospitals in India. The government can even incentives the whistleblowers of such malpractices by amending the whistleblowers’ Act.
- Engage in bilateral agreements: The government can sign bilateral agreements with countries like the US, the UK, Canada, Australia towards working on a policy of “brain-share”. For example, destination countries would be obliged to supply healthcare workers to India in times of need, crisis situations like a pandemic, etc.
Global level changes
- Creating a code of conduct for ethical recruitment: The global countries have to come together and create a consensus code for ethically recruiting health care professionals. This will reduce the exploitation of health care worker abroad.
- Facilitating circular migration: Almost 37 percent of health care workers concentrated in North and South American countries. But they share only 10% of the global disease burden. On the other hand, countries in Africa and Asia share more disease burden and less health care worker presence. So, the world nations have to come together and facilitate circular migration of health care professionals in terms of crisis situations.
Conclusion
India needs systematic changes such as increased investment in health infrastructure, ensuring decent pay to workers and building an overall environment to retain health care professionals. With the advent of the pandemic, India can import medical oxygen, import vaccine, but India cannot import health professionals. So, It is high time for Indian government to not only increase public spending but also increase the Doctor and nurses ratio and prevent brain drain in the health sector
“SAMVEDNA Helpline”- Tele Counselling of Children Impacted by Covid-19
Contents
What is the News?
Children impacted by the Covid-19 pandemic are being provided telecounseling through SAMVEDNA.
About SAMVEDNA:
- Firstly, SAMVEDNA stands for Sensitizing Action on Mental Health Vulnerability through Emotional Development and Necessary Acceptance.
- Secondly, it is a toll-free helpline number that aims to provide psychological first-aid and emotional support to the COVID-19 affected children
- Thirdly, the National Commission of Child Rights(NCPCR) provides the tele-counseling.
- Fourthly, this tele-counselling service is available on a toll-free number 1800-121-2830. It is exclusive for children who are willing to talk and are in need of counselling.
- Categories: Tele-counselling is provided to children under three categories:
- children who are in quarantine/isolation/COVID care centres,
- children who have COVID positive parents or family members and
- Lastly, children who have lost their parents due to the pandemic.
About National Commission for Protection of Child Rights(NCPCR)
- NCPCR is a statutory body. It was established in 2007 under the Protection of Child Rights Act (CPCR), 2005.
- Ministry: It is under the administrative control of the Ministry of Women & Child Development.
- Mandate: It aims to ensure that all laws, policies, programmes and administrative mechanisms are in accordance with the child rights perspective as put forward in the Constitution of India and also the UN Convention on the Rights of the Child.
Source: PIB
Method to Estimate COVID-19 Deaths in India
Synopsis: Instead, of calculating the ‘excess’ death at the national level, Excess death calculated at the District level will provide a more accurate estimation of COVID-19 deaths in India.
Background
- To understand the magnitude of the pandemic there is a need for estimating COVID-19 deaths globally and in India.
- The most commonly used approach is the “excess” death approach. It is the difference between death in Normal years and deaths during the Covid-19 period.
- Further, it includes deaths directly caused by COVID-19. It also includes deaths indirectly caused due to the lack of access to care for other diseases during the pandemic and the lockdown.
- Based on the excess” death approach estimates have been released globally. However, India’s reported deaths contradict Global estimates.
- At present India needs to rely on global estimates rather than India-specific data.
- This is because of poor data availability for COVID-19 excess deaths, India has been classified in category 3 countries by WHO.
- Category 3 constitutes countries where the data on deaths are not available or usable. Hence, they are forced to adopt an indirect approach of using data from other countries.
- So, to have a reliable estimate for India on Covid deaths, India needs to calculate Excess death at the District level by analyzing the data from the Civil Registration System (CRS).
What do the global estimates reveal about the Covid deaths?
As far as now two estimates have been released globally.
- One, the World Mortality Dataset. It is the largest international dataset of all-cause mortality in 89 countries. According to this dataset, researchers conclude that excess mortality exceeds the number of reported COVID-19 deaths in these countries by over 1.6 times.
- Two, The Institute for Health Metrics and Evaluation (IHME). According to their findings, global COVID-19 deaths by May 3, 2021 is at 6.93 million. This is two times higher than the reported number of deaths of 3.24 million.
- India accounted for about 10% of them at 6,54,395. This is about three times higher than the reported official figure.
What needs to be done?
India currently has only crude estimates based on the number of extra deaths reported as compared to previous years. To improve the accuracy of Covid death estimation, we need to do the following.
- First, before estimating excess deaths a probable baseline should be defined. One can do it by estimating the mean and standard error based on data for the last five years to provide a probable range for a baseline.
- Second, Civil Registration System (CRS) data of districts with an acceptable quality of registration should be analyzed to estimate the excess deaths in a given period.
- There are enormous differences in the severity and timing of the epidemic. Therefore, the health system’s capacity within India combining data at higher levels is likely to lead to errors in estimation
- Third, for districts that lack an acceptable quality of registration, we could use alternative approaches.
- Finally, the long-term way out for India is to address the data limitations while academics work on refining their statistical approaches.
Source: The Hindu
No learning from the Spanish flu
Synopsis: The governments of several countries have failed to understand and foresee human behaviour. This is even after they have witnessed a pandemic like the Spanish Flu in the past.
Introduction
- The Spanish Flu of 1918 was the most severe pandemic in history. It lasted for 2 years, in 3 waves, with 500 million people infected and 50 million deaths. Most of the mortalities occurred in the 2nd wave.
- The people were fed up with the quarantine and social distancing measures. The people rejoiced in the streets as soon as the measures were lifted. After which the second wave occurred and claimed tens of millions of lives.
- According to James Harris, a historian at Ohio State University, the reason behind the spread of a second wave was that officials were reluctant to enforce restrictions during the war despite the presence of a new mutated strain.
Why did the people not take lessons from the past?
We haven’t learned from history to prevent millions of infections and deaths worldwide.
- Firstly, Knowledge doesn’t change behavior. Having information about the Spanish flu is very different from having to live through a similar pandemic. For instance, being informed about the protectiveness of the masks doesn’t make people wear them. Similarly, knowing about social distancing doesn’t make people perform it.
- Secondly, in many countries, people were fed up with lockdowns, wearing masks, staying at home, and not socializing last year. Human beings are social animals. Social banishment has been proved to cause pain in the brain similar to putting up with physical pain.
- Thirdly, as soon as the number of cases began to decrease by the end of the first COVID-19 wave, governments and people across the globe started to let their guard down. Many businesses were allowed to restart.
- For example, restaurants that were doubted to be one of the major centers for the spread of COVID-19 were given consent to open. Signs outside their doors read ‘No entry without a mask’, but visitors could remove their masks even while not eating once they were inside.
- People could talk, laugh, sneeze, and cough in indoor non-ventilated spaces. These people knew about the threats of this behavior. Some of them must have read about the Spanish flu. However, awareness and action often lie at opposing ends.
Where did the governments go wrong?
Everyone needs to contribute to breaking the chain of COVID-19 infections. However, the final duty of managing the pandemic cannot be on the people. It is the job of governments.
- Governments of most nations failed to learn from the Spanish flu because they failed to realize and foresee human behavior. For instance, the government in India allowed election rallies and religious gatherings.
- The government hesitated in imposing a lockdown despite the rise of new strains of the virus. Leaders were seen making speeches in crowds and conducting meetings without masks.
- Every politician wants to win over people and give them what they want. They declared victory prematurely and gave rise to policies that caused the second wave.
The conclusion
- India had the opportunity to learn from the mistakes of other countries which opened up too soon after the first wave. But it didn’t. This has led to a huge rise in COVID-19 cases and deaths.
- Overconfidence in the government’s ability to manage the pandemic and underestimation of the ability of COVID-19 to cause infections and deaths in the second wave led to the surge in infections. We have the benefit of curbing COVID-19 by vaccinating people now at least.
Source: Click here
Kerala Model to tackle the Covid-19 Pandemic in India
Synopsis: The Kerala model provides a lot of lessons to the Center and the State governments to tackle the pandemic.
Contents
Introduction:
India at present is not only battling with Covid-19 cases but also battling with many associated issues. Such as floating dead bodies in the Ganges, the demand for medical oxygen and the challenges with the vaccination drive, etc. All these impact the health infrastructure of India a lot.
Lockdown and prerequisites:
With these challenging issues, there is a debate going to implement a national lockdown. Even if a national lockdown is not feasible, regional lockdowns/micro-containment zones are necessary. But before imposing them, there are a few things to consider.
- The lockdown has to protect the interests of migrants and other worst affected sectors.
- Adequate preparation and planning are required to ensure the proper continuation of lockdown.
- The government has to provide an adequate time for the people to get themselves to prepare for the lockdown.
Lessons from Kerala model to tackle the pandemic:
The Kerala model provides lessons to not only implement the lockdown but also to tackle the pandemic effectively. The important initiatives are,
- Transparency in governance: The government of Kerala provided daily press briefings. During that, the government reveals detailed information on the rate of infections and fatalities. Apart from that, the regular information includes the availability of beds, ICUs, oxygen, vaccines, and measures taken to deal with the pandemic.
- All these increased public participation in controlling the pandemic. Further, the public also knows the gravity of the situation and built people’s trust and confidence in government measures.
- So, the Central government and other state governments have to see transparency as an important part of the COVID-19 response toolkit.
- Tackling Hunger: To tackle poverty and hunger, the Kerala government provided food kits to homes. Apart from that, Community kitchens and Janakeeya hotels(people’s hotels) have also opened to control hunger.
- Providing adequate medical attention: The government of Delhi faced a lot of challenges in providing adequate medical facilities. As a result, people used personal networks to hunt for oxygen and beds in hospitals.
- In contrast, the Kerala model created First-level treatment centers and second-level treatment centres. These models screened and treated people appropriate to their symptoms.
- Only the most serious cases reach the district and specialty COVID-19 hospitals.
- Further, Domiciliary care centres have also been created in Kerala to provide shelter, food, and treatment to those who do not have space at home to be quarantined. This prevented the migrant worker not to flee to their hometowns in panic.
- In private hospitals, 50% of the beds have been declared as COVID-19 beds. Also, the government fixed the cost of RT-PCR testing and treatment charges in private hospitals at a reasonable level.
- The private hospitals filed a PIL against fixing of price. But the Kerala High Court dismissed the petition.
- Similar to the ‘Mumbai model’, beds are allotted through centralised control rooms in each district. These rooms also monitor the requirements of oxygen and ambulances.
- Empowering the Local bodies: The Kerala model identified the Local Bodies as a first line of defence in the fight against COVID-19. They perform various functions in controlling the pandemic. Such as,
- They look out for fresh infections amongst their constituencies and ensure the supply of medicines and provisions.
- Panchayat members motivate people to get vaccinated
- The Local body members also supervise the implementation of the lockdown in their locality.
- Apart from that, they also set up help desks, providing ambulances facilities, and organising food packets.
Suggestions:
- The government has to understand that the battle against the Covid-19 is a long one. So, the Center and the States have to prepare for not only the second wave but for the third and fourth wave. To control them lockdowns will be inevitable until the progress of vaccination drives. The Kerala model has lessons for both lockdown and vaccination drives.
- Twelve Opposition parties issued a joint letter to the Center. In that they demanded,
- The government should initiate a free universal mass vaccination campaign.
- Ensuring an uninterrupted supply of medical oxygen and vaccines.
- Invoking compulsory licensing to expand domestic vaccine production.
If the Centre provided these things and the other States adhere to the Kerala model then India can tackle the pandemic effectively.
Source: The Hindu
Centre releases “Covid-19 guidelines for rural areas”
Contents
What is the News?
The Central Government has released new guidelines in the wake of the spread of coronavirus disease (Covid-19) in rural areas.
About the Covid-19 guidelines for rural areas:
Three Tier Structure: The guidelines recommend a three-tier structure to manage Covid-19 pandemic in rural areas:
- Firstly, to establish 30-bed Covid Care Centres(CCCs) in villages to treat mild cases.
- Transforming community halls and panchayat buildings into CCCs. These centres should also be equipped with at least two oxygen cylinders.
- Secondly, Primary Health Centres (PHCs), Community Health Centres (CHCs) and Sub-district Hospitals shall handle moderate cases of the Covid-19 cases. Persons having an oxygen saturation level below 94 will be treated here.
- Thirdly, district hospitals or private hospitals should manage severe cases with ambulances available for the rapid transport of patients.
Other Key Covid-19 guidelines for rural areas:
- Testing: Community Health Officers(CHOs) should be trained in performing Rapid Antigen Testing(RAT). These RAT kits should be provided at all public health facilities including Sub-centres (SCs) and PHCs.
- Symptomatic Cases: The symptomatic cases can be treated at the village level after teleconsultation with the CHO. Further, the cases with comorbidity or low oxygen saturation will be sent to higher centres.
- Surveillance: In every village, active surveillance should be done for influenza-like illness. This will periodically be held by ASHA workers. The Village Health Sanitation and Nutrition Committee(VHSNC) will help ASHA workers in this regard.
- Ayush Doctors: Qualified AYUSH doctors, final year AYUSH students or final year B.Sc nurses may be considered to run the Covid Care Centres(CCCs).
- Contract Tracing: The guidelines also focused on the need for contact tracing at every level.
- Covid kit: Each Covid-19 household would get a “home isolation kit” with paracetamol, ivermectin, multivitamin tablets. The kit will also have provisions for periodic measurements of patients’ oxygen level and fever.
Source: Indian Express
- Firstly, to establish 30-bed Covid Care Centres(CCCs) in villages to treat mild cases.
US “CDC guidelines” for fully vaccinated people
Contents
What is the News?
The US Centers for Disease Control and Prevention(CDC) said that fully vaccinated persons will no longer need their masks indoors and outdoors.
About the CDC Guidelines:
- US’s CDC guidelines said that a fully vaccinated person can take off his/her masks.
- The new guidelines are only for people who are fully vaccinated. This includes condition like,
- Two weeks have passed since the second shot of the two-dose vaccines.
- Or if a person received a single dose of the Janssen vaccine.
- The guidelines from the Centers for Disease Control(CDC) are just guidelines. State and local rules still apply.
Places where the persons need to wear masks:
- The guidelines say fully vaccinated people must still wear a mask. Especially in health care settings, transportation hubs such as airports and stations, and public transportation.
Are these CDC guidelines based on science? The decision was taken based on the following reasons:
- Current State of Pandemic in the US: The number of cases, hospitalizations and deaths in the United States have declined significantly in recent weeks.
- Effective Vaccination: The US’s followed an effective vaccination policy. Further, some people are immune because of the previous coronavirus infection. So, the pandemic is gradually coming under control.
- Study on vaccinated people: A study conducted at a major medical center in Israel found that out of 5,500 fully vaccinated workers, just eight people developed any COVID-19 symptoms.
Source: Indian Express
Issues With Technocratic Approach to Vaccination Drive
.Synopsis – The current technocratic-based vaccination drive in India excludes the digitally illiterate population of the country. It is leading to substantial biases and inequality.
Introduction-
- The GOI launched CoWin portal to digitize the vaccination drive and made online registration mandatory for vaccination booking [18-44 age groups].
- The approach has resulted in a digital divide among the rural population. Moreover, it also brought several other issues, such as vaccine exclusion and lack of privacy, with it.
Key issues with the current technocratic based vaccination drive
- Firstly, Lack of technical literacy –With no internet access and understanding of CoWin portal functions, the majority of India’s rural population is left out of COVID vaccination efforts.
- Concerns-
- Digital divide- Only 34.60 percent of the rural population has access to the internet.
- Lesser registration through CoWin portal- According to CoWin data, only 2,52,96,511 of the 14,42,10,652 vaccine registrations [for 45-plus age group] were done through CoWin.
- Concerns-
- Secondly, the COWIN portal ignores data protection and cybersecurity- The CoWin website lacks a privacy policy, putting medical healthcare data at risk of disclosure through third-party providers.
- The CoWin website is contrary to-
- The Supreme Court’s right to privacy judgment
- Also, the GOI’s departmental guidelines for official websites states that while collecting data, government websites “must incorporate a prominently displayed privacy statement…”.
- The CoWin website is contrary to-
- Thirdly, Use of Facial recognition technologies FRT also poses a threat to privacy – The CEO of the National Health Authority said that Aadhaar-based FRT will soon replace biometric fingerprint or iris scan machines at Covid-19 vaccination centres. It will avoid infections.
- The FRT will increase the risk of exclusion and discriminatory outcomes. Moreover, FRT is not an accurate mode of identification, thus affecting the proper dispensation of the shots.
The technocratic approach is prioritizing data collection and efficiency over vaccine equity. It disregards the experience of public healthcare and digital rights experts. The present deployment of CoWin, is undermining the right to health, instead of augmenting it.
Source-The Indian Express
Bad Policy Making Aggravated the Pandemic Disaster in India
Synopsis: Bad Policy-Making by the government during and before pandemic aggravated the Pandemic Disaster in India. Adherence to Key Principles of Healthcare, Economy, Data integrity, and Science would have limited the impact of the Pandemic in India.
What are the key principles forgone by the government?
- First, prioritizing universal health coverage instead of strengthening Public health facilities
- India prioritized insurance coverage after 2014, for example, Ayushman Bharat. Whereas, international experience showed strengthening public health care is the right way.
- For instance,
- UK’s National Health Service Act revolutionized health care in the United Kingdom by delinking it from a person’s income.
- Kerala’s heavy investment in public health care in the 1950s increased the capability of Human resources.
- Even, the high-level expert group appointed by the Planning Commission concluded that progressive strengthening of public facilities is the only way to achieve universal health care.
- Second, discarding the principles of Science worsened the Pandemic situation. There are instances when Science was least prioritized by the government,
- Government representatives supporting Patanjali’s Ayurvedic cure for COVID-19.
- Ignoring the Suggestions of public health expert or Scientists in Public policymaking related to Lockdown, organizing Kumbh mela, Election rallies
- Third, Government’s apathy towards prioritising Data integrity. For instance,
- One, evasion of Economic data: For example, Maximizing GDP numbers, employment statistics changing baselines, withholding periodic labor force surveys.
- Two, under-reporting of Covid-19 infection and Deaths.
- Fourth, negligence of Good economics principles. For instance, relying on Freebies rather than prioritizing sound Welfare economics like Institutionalising social security net.
- According to the latest report by the Azim Premji University, 230 million Indians slipped below the poverty line during the pandemic.
- Providing Social security net to the BPL population would have limited the Pandemic disaster in India.
- Even the global experience from US, UK, Germany, and China proved the same. Yet, India discarded the global experience.
Adherence to basic scientific and rational principles, helped India to effectively fight against smallpox and polio. This needs to be replicated now.
Source: The Hindu
- First, prioritizing universal health coverage instead of strengthening Public health facilities
State should form a joint committee to negotiate COVID vaccine price
Synopsis- Vaccine Price, availability and affordability [for 18-44 age group] would require a coordinated effort from state governments.
Introduction-
- The central government has pulled out from the third phase of the vaccination drive. The center has provided state governments’ the full responsibility for vaccinating [a group that constitutes about 40 per cent of the population].
- Now state governments have to procure vaccines directly. Further, they also need to compete with private players at the same time for a better price. As there is only a limited number of capacity and vaccine suppliers.
How can the state bring down vaccine prices?
In contrast to a market with multiple buyers, a single buyer can always negotiate a lower price for a product with one or more sellers. Thus, to bring down vaccine price, the State governments should form a consortium. There are some factors related to this. Such as,
- Involvement of Pre-purchase agreements- This would tackle any uncertainties from the point of view of vaccine manufacturers. It will also allow for faster expansion of production capacity.
- Delay in the formation of the consortium will impact the procurement – Any delays will strengthen the potential private buyers’ position. It will automatically weaken the position of the consortium to negotiate a lower price. This will result in,
- Further, widening of vaccination gap between the rich and the poor – The price difference between the consortium’s agreed prices and private sellers is likely to encourage inequity and black marketing
Thus, the formation of a consortium provides a mechanism to achieve affordable prices in India. Further, there is also a survey conducted on willingness to pay (WTP) for Covid-19 vaccines.
Key highlights of a survey on willingness to pay (WTP) for Covid-19 vaccines
- The survey is conducted for WTP for two possible vaccine choice [one is 100 percent effective and the other is 70 percent effective]
- The maximum WTP on average stood at Rs 140 for a 100 % effective vaccine, and at about Rs 109 for one with 70 % effectiveness.
- Only 2 % were willing to pay Rs 600 or more to 100 % effective vaccine and 1.5 % were willing to pay the same amount for the other vaccine.
- Nearly 66 % of the respondents experienced an income reduction of more than 50 percent as compared to the last year’s income levels. WTP also declined uniformly with the level of economic shock experienced.
- So, the economic ability of these households to afford vaccination is severely restricted.
- Apart from that, leaving sections of the eligible population out of vaccine coverage poses further risks of mutations in the virus.
Suggestions to reduce Vaccine price and provide universal vaccination
Shortage of the vaccine, poor administration and vaccine hesitancy is the reason for low rate of vaccination, therefore-
- State governments must take immediate action to form a consortium and make provisions for further subsidization of the vaccine.
- Implementing budgetary solutions like public health bonds will help to improve public finances.
- Further, the government must focus on Universal vaccination. To achieve this, the center can allow State governments to exceed budget deficit targets.
Source- The Indian Express
Measures to control the impact of Pandemic in rural India
Synopsis: To limit the impact of Pandemic in rural India, states must produce reliable data on Covid-19 infection. State governments need to build capacities and involve panchayats in Covid-19 response.
Background of Pandemic in rural India
- To tackle the second wave, active coordination between all three tiers of Government (The union, the State and Panchayat) is necessary.
- The second Covid-19 wave has impacted Rural India equally. This necessitates the need to implement the delivery of vaccines and healthcare services on a war footing in rural areas.
- However, ensuring access to health services for all in rural India is a big challenge due to various reasons.
Challenges in tackling Pandemic in rural India:
- Disparities in access to health care between urban and rural India is high: For instance, 75 per cent of hospitals are in urban areas.
- Denial attitude: People in rural India are hesitant to test themselves. Further, they are not willing to admit that they have the disease. This denial attitude is leading to the loss of lives.
- Lack of Medical Kits for testing: Many in Rural India lack access to medicine, thermometers and oximeters.
- All the above problems have complicated the availability of reliable data on the number of infected persons as well as the death caused by Covid-19. This resulted in ineffective planning. For instance, hurdles in Oxygen availability and allocation.
Suggestions to tackle Pandemic in rural India
- Firstly, State officials and district commissioners should actively report both positive numbers and deaths. As it is important to have the right data. For this, mobile testing vans need to be introduced immediately.
- Secondly, families with Covid-positive members should be given kits consisting of medicine, thermometers and oximeters. The delivery of the kits can be supplied through the panchayats.
- Thirdly, a task force, consisting of all ward officers, district and municipal commissioners, should map out the demand for health care equipment. This will help Epidemiologists, experts and doctors to predict better the requirement of oxygen, medical devices, etc.
- Fourthly, learning from the best practices of Mumbai administration.
- Mobilisation of human resource: Mumbai used the food and drug administration department for planning the demand and ensuring the supply in the city.
- Foresighted Planning: Every ward in the city of Mumbai also created an emergency stock of oxygen. This reduced the time to send supplies to hospitals running out of oxygen.
- Building additional capacity rationally: One of the important lessons to be learnt from Mumbai is that hospitals should only increase beds if they can provide oxygen.
- The state should also increase hospital capacity by creating additional oxygen plants with adequate ICU beds.
- Fifthly, Decentralised decision-making and planning. The Union government should decentralise crucial decisions to the state governments.
These steps can ensure a better reduction rate of Covid-19 Pandemic in rural India.
Source: Indian Express
“Community Transmission”(CT) and “Categorisation of diseases”
Contents
What is the News?
India is registering the highest number of cases globally every day. But the World Health Organization(WHO) Report mentions, India is yet to label itself in the category of community transmission(CT).
Note: Currently, India has labelled itself in the category of ‘cluster of cases’ category.
About Categorisation of diseases:
In general, the World Health Organization (WHO) uses the following categories to describe transmission patterns:
- Sporadic cases,
- Clusters of cases
- Community transmission.
What is the category of the Sporadic case?
- These are a small number of cases (one or more) either imported or detected locally
What is the Cluster of Cases category?
- Cluster transmission has been used by Indian authorities to identify infections that are largely concentrated in a limited locality. The disease concentration is often within a family and its extended circle.
- Under this, cases detected in the past 14 days are predominantly limited to well-defined clusters. Further, the disease detected will not directly be linked to imported cases.
What is Community Transmission(CT)?
- It means that the epidemic has become so widespread in a community. Further, it gets difficult (if not impossible) to determine who is passing on the infection to whom.
- In simple terms, Community Transmission is classified when the source of the infection is not known.
- CT will happen when new cases in the last 14 days cannot be traced to those who have an international travel history or to any specific cluster.
Stages of Community Transmission: WHO guidelines suggest four subcategories within the broader definition of CT:
- CT1: Low incidence of locally acquired cases detected in the past 14 days
- CT2: Moderate incidence of locally acquired cases detected in the past 14 days
- CT3: High incidence of locally acquired cases in the past 14 days
- CT4: Very high incidence of locally acquired cases in the past 14 days.
Countries classified under Community Transmission:
- Countries such as the United States, Brazil, United Kingdom, France have labelled themselves as being in ‘community transmission’.
- However, among the countries with the most number of confirmed cases, Italy and Russia do not label themselves as being in community transmission.
Government policy based on Categorisation:
- India’s refusal to describe itself as being in community transmission had an effect on how the authorities addressed the pandemic.
- Under Cluster Transmission, the government gives priority to testing, contact tracing and isolating to prevent further infection.
- On the other hand, under community transmission, the government prioritises treatment and observing advisories to stay protected.
Source: The Hindu
Centre Should Relook its Vaccine Policy
Synopsis: The vaccine policy of the government would enhance the difficulties of states and the vulnerable population. It would give greater benefit to the affluent class and the urban regions. Therefore, the center must relook it in order to make it more equitable.
Contents
Background:
- The Centre government has filed an affidavit in Supreme Court with reference to the COVID-19 management case. It has insisted on the continuation of its revamped vaccine policy that was introduced for vaccinating the 18+ population.
- The policy was revamped after the demand to universalize the vaccination program among all adults came from various states.
About the Vaccine Policy:
- The center has put forward a more liberalized policy under which it will procure 50% of the total vaccine production. While the states and private sector will be allowed procurement of 25% each in every state.
- Each state will get vaccines based on a quota decided by the Centre government and there would be a uniform price of vaccines across all the states.
- The policy would increase the vaccine maker’s revenue as Covaxin will fetch a weighted price of Rs. 477 per dose. Similarly, Covishield would be priced at Rs. 302 per dose.
- The weighted average is calculated based on a share of 50% for the Centre, 25% for States, and 25% for the private sector for both vaccines.
Procurement Price Covaxin Covishield Centre 154 154 States 400 300 Private 1200 600 However, many experts are demanding a relook of this policy as it may not deliver the desired results.
Issues with vaccine policy that demands a relook:
- Firstly, Bias against the Vulnerable population: The private players will sell vaccines at higher prices that may not be affordable for the vulnerable population. Further, the addition of 600 million (18-44 age category) people, has created extreme vaccine shortages thereby leading to more exclusion under the current program.
- Secondly, Against International Practice: The national government is solely buying the vaccines in every other country. Although there are some exceptions like Indonesia and the Philippines. Here the corporates are allowed to buy internationally, to vaccinate their workers for free.
- Thirdly, Inconsistent Nature: The policy is based on the principle of liberalization. However, the center is controlling both price and quantity for every State. This is against liberalization.
- It is also ironic that on one hand, the center is deciding which manufacturer of Remdesivir will sell how much to which State and at what price.
- While on the other hand, it is deregulating the Covid vaccine market which currently has just two suppliers.
- Fourthly, Burden on States: Instead of the full production at zero cost, the States now got one-quarter of the production at twice or more the price paid by the Centre.
- Fifthly, Problems with Private Participation: It is not clear how to define the private sector in a specific state. Procurement contracts by private participants are done at a corporate level and not by State units. This may benefit large urban areas, where there is a greater presence of the private sector.
Way Forward:
- Firstly, the centre should procure 100% doses and equitably distribute them among the states. Its ability to give bulk orders allows it to buy vaccines cheaper than States or the private sector.
- It can increase its procurement price from 154 in order to raise the revenue of vaccine producers.
- Further, the companies must be given large long-term orders for 100% of India’s needs. This would enable them to invest more and sell globally.
- Secondly, the government should also widely licence Covaxin in order to boost production and tackle vaccine shortages. Most of the core work in developing the vaccine was done at the ICMR-NIV in Pune, indicating the use of public funds for development.
- Thirdly, it should arrange more supplies by negotiating with global suppliers through the diplomatic route. This would also help in converting the idea of the door to door campaign into a reality.
- Lastly, it should give special interest-free 50-year loans to States in order to bear the additional burden of the vaccine program.
Social Issues Current Affairs Updates For UPSC IAS Mains 2024 Examination
WHO warns against use of “Ivermectin” to treat Covid-19
What is the News?
The World Health Organization(WHO) has recommended against the use of ‘ivermectin‘ drug for the treatment of COVID-19 patients.
Despite this, Ivermectin is still listed in India as a possible treatment option for mild COVID-19 patients under home isolation.
About Ivermectin Drug:
- Ivermectin is an orally administered drug used to treat parasitic infections. These include parasitic infections of the intestinal tract, skin, and eyes.
- How does it work? Ivermectin works by binding to parts inside the parasite. It eventually paralyses and kills off the parasite. Or it stops adult parasites from making larvae for a while. This provides relief to the parasitic infection.
- Why is it used for Covid-19 patients? Ivermectin was found to be effective in reducing the multiplication of certain RNA viruses. Such as SARS and Covid-19 RNA. Hence, it is used for the treatment of COVID-19 in mild to moderate cases.
What has WHO said? WHO has recommended against the use of Ivermectin drug for Covid-19 patients on following grounds:
- No scientific basis for a potential healing effect against Covid-19 especially from pre-clinical studies;
- No meaningful evidence for clinical activity or clinical efficacy in patients with Covid-19 disease,
- A concerning lack of safety data in the majority of studies.
Source: The Hindu
Impacts of Digital inequality on Health and Education
Synopsis: Digital inequality or Unequal access to digital platform is worsening inequalities in accessing public goods such as Education and Health.
Contents
Facts on Digital inequality in India
- Inequality in access to digital devices: According to National Sample Survey (2017), only 6% of rural households and 25% of urban households have a computer.
- Inequality in access to Internet Services: Only 17% in rural areas and 42% in urban areas have access to internet.
- Due to the prevailing inequality in digital access, the digital solutions offered for providing basic services such as health and education have failed.
Reasons behind Digital inequality in education
- Lack of access to online classes: According to the Azim Premji Foundation, ASER and Oxfam report, between 27% and 60% could not access online classes, due to lack of devices, shared devices, inability to buy “data packs”, etc.
- Loss of Lives: a college student studying in Delhi and a 16-year-old in Goa died by suicide as their family could not afford to repair the phone they used.
- Lack of learning environment at home: a quiet space to study is a luxury for many. For instance, 25% of Indians lived in single-room dwellings in 2017-19. Further, girls at home are burdened with domestic chores.
- Advantages in Peer learning is forgiven: For instance, even students with issues in English language found easy to pick up the language with the help of peers. Now, online education has deprived them this advantage.
Reasons behind Digital inequality in health
India’s Poor population is at a disadvantage in accessing good health care due to the following reasons,
- One, very low public spending on health (nearly 1% of GDP). This has contributed to the high share of ‘out of pocket’ (OOP) health expenditure in India was over 60% in 2018.
- Even in the United States, where health system is highly privatised, OOP was merely 10%.
- Two, the private health sector in India is poorly regulated. As a result, they charge exorbitant prices and has contributed towards the development of black market for scarce services
- Three, shortage of essentials such as drugs, hospital beds, oxygen, vaccines etc.,
To overcome the above challenges, the government chose to promote Digital health services as a solution. However, digital health services have resulted in unequal access to health care due to the following reason.
- Exclusion: Platform- and app-based solutions can exclude the poor entirely thereby denying their right to access health care. For instance,
- People with knowledge of technology are at advantage to access digital health services, compared to the vulnerable populations without digital knowledge. For example, in the case of CoWIN, it is much harder for people without phones, computers, and the Internet to book slots.
- Language barrier: The website is only available in English, restricting the use for the mass non-English population.
- Privacy violation: For example, the push towards digital health ID databases may result in health records being used by private entities without our consent.
Way forward
- Need to increase spending on health to 3% of GDP to reduce 50% of out-of-pocket expenditure as per Economic survey 2021.
- Need to enforce laws against medical malpractices strictly.
- The Centre needs to ensure Patient privacy. Decentralized digital storage followed in countries like France and Taiwan should be created rather than creating a centralized database for digital health records.
Source: The Hindu
Time to Revive the Plan for Indian National Health Services
Synopsis: The pandemic has broadly highlighted the inadequacy in our health care system and has brought serious consideration for the formation of the Indian national health services.
Background
- There has been a coordinated effort from medical staff, the Centre, the state, and other state institutions to control the Pandemic. For instance,
- The railways are running special trains carrying oxygen supplies.
- There is an involvement of military in medical supply chains.
- The Karnataka government has ordered private hospitals above a certain size to reserve 75% of their beds for COVID-19 patients, who will be paid for under a public scheme
- Despite these measures, the Indian healthcare system is struggling to control the Pandemic.
Issues in the Indian health care system
- Inadequate public health expenditure: India spends nearly 1% of GDP.
- Inadequate public health providers: for instance, in certain rural areas the doctor-population ratio is over 1:40,000
- High out-of-pocket expenditure: Medical expenses constitute the major reason for personal debt in India.
- Systemic issues: Highly fragmented, corruption, urban-centered, elite-focused.
To address the issues ailing our health care system, India needs to form Indian National Health services, in line with British National Health Service.
How the British National Health Service function?
- Firstly, the service is funded entirely from Public money (Taxation). The budget includes a payment to general practitioners, most of whom remain private providers but are paid by the state for treating NHS patients
- Secondly, all hospital treatment and medicines are free, as are outpatient and follow-up appointments.
- Thirdly, the NHS is the largest employer in the U.K. and Its current budget is about 7.6% of GDP. Despite being large in scale, it provides highly localized access to care.
- Fourthly, the formation of the British National Health Service has resulted in providing top-class universal healthcare, including training and research. However, some issues like subjective preference to patients of different social classes still exist.
- Fifthly, in India, during 1946, the civil servant Sir Joseph Bhore proposed Indian national health services broadly modeled on the lines of the British National Health Service or NHS.
- Lastly, he further recommended the integration of preventive and curative medicines at all levels.
Source: The Hindu
- There has been a coordinated effort from medical staff, the Centre, the state, and other state institutions to control the Pandemic. For instance,
Ex-Defence doctors to provide online consultation on “e-Sanjeevani OPD”
What is the News?
Ex-Defence doctors will also now provide online consultation on e-Sanjeevani OPD to the needy patients in Rajasthan. This facility will be extended to other states shortly.
E-Sanjeevani: It is a telemedicine platform of the Ministry of Health and Family Welfare(MoHFW). The platform has enabled two types of telemedicine services:
- eSanjeevani: It is a doctor to doctor telemedicine system being implemented under the Ayushman Bharat Health and Wellness Centre(AB-HWCs) programme. It seeks to connect all 1,50,000 HWCs using the hub-and-spoke model by December 2022.
- eSanjeevaniOPD: It was launched amid the Covid-19 pandemic to enable patient-to-doctor teleconsultation.
e-ICU Platform:
- e-ICU has been launched on the e-Sanjeevani platform. It has been developed by the Medical Branch of Integrated Defence Staff in coordination with C-DAC Mohali.
- Purpose: The portal will help the Medical Officers to get real-time consultations from specialists doctors in managing their patients.
- The portal is based on the Hub & Spoke model. Under this, Medical Specialists are at the Hub and the Medical Officers are at the Spokes. This will help to leverage technology for overcoming the specialist shortages as part of the Digital India mission.
Source: PIB
Central Vista judgment: Issue of public participation in public projects
Solving Present Health Care Crisis With Lessons from Green Revolution
Synopsis: India is facing a severe shortage of healthcare infrastructure. But, this is not the first time. India has already tackled a food shortage which was worse than this during the 1960s by the green revolution.
Contents
Introduction:
India is witnessing shortages of almost everything that is needed to treat COVID-19 patients. Such as hospital beds, drugs, ventilators, Vaccines, and, above all, medical oxygen. Many countries such as the US, the U.K., the European Union, and even China offered help to India to tackle the second Covid-19 wave. This situation resembles India from the Mid-1960s.
The Situation of India during the 1960s:
- India faced a severe food shortage after facing two consecutive years of drought. After that, India forced to accept US aid. It is a point to note that, India at that time neither supported USSR nor the USA.
- President Lyndon, send food to India by the shipload. So that India can keep the ship on a short lease”
- Though it was the worst situation, the response of Indian leadership was exemplary.
- Prime Ministers Lal Bahadur Shastri, Indira Gandhi, and others brought the scientific and bureaucratic communities to debates. Especially to bring a quantum leap in food production.
- The debate turned into action very soon. Within a few years, India achieved Food security.
- No one imagined that India from such a dreadful situation will achieve food security this fast.
- The Green Revolution stands out in Indian history even today. It is the display of extraordinary accountability of political leadership, combined ability to resolve an issue from bureaucrat and Scientific community.
Advantages for present India vis-à-vis 1960s:
- In March 2020, India faced a similar 1960s problem on health infrastructure. To improve the medical capability and delay the Covid-19 spread India imposed lockdown at very short notice.
- But India has certain advantages at present when compared to the situation in 1960. Such as,
- At present, India has a better industrial base, compared to the 1960s. So, India needs some time to ramp up hospital beds, ventilators, and oxygen supply.
- Similarly, certain parts of India actually have a surplus of oxygen. They can help to fulfill urgent demands.
- India has an enormous foreign exchange reserve at present. This is not the case in the 1960s. So, India was in a better position to import some crucial medical inputs such as vaccines.
Suggestions:
- Inter-State variation in death rate is directly related to the amount of health spending with respect to the state domestic product. Similarly, the health infrastructure of the country is also important. So, to avert any future crisis States have to increase the level of spending on health.
- India also witnesses a hike in Food prices during the pandemic. This denotes that there is a disruption of supply in between in the supply chain. This will be further impacted due to various State-level lockdowns. To avoid this, PM has to interact with the farming community. This is an important lesson for India from the mid-sixties.
Source: The Hindu
Nation wide lockdown is an Opportunity to Improve Health Infrastructure
Synopsis – At last, states are implementing strict lockdowns. It is to handle the out-of-control spread of Coronavirus infection. Now, states should use this opportunity to improve health infrastructure in the country.
Introduction
- Life threat from a mutating virus has aggravated manifold. An increase in Covid cases from 9,000 new daily in early February to over 4,00,000 in May, is mostly caused by incorrect messaging, political rallies, and religious gatherings.
- To curb the transmission of the virus, there is a need to impose national wide lockdown. However, lockdown should be used to improve the health infrastructure.
Benefits of a lockdown
- Break the chain of transmission of COVID-19 – The lockdown will help to break the chain of transmission of the virus so that number of cases falls.
- Lockdown will provide breathing time-
- The chance of respite for the overburdened medical community – The lockdown will help healthcare professionals to manage existing cases.
- In the meantime, the government should increase essential health supplies such as oxygen concentrators, ICU beds, and ventilators. It is necessary to treat Covid-19 patients.
- The lockdown provided a breathing space for the government to ramp up COVID-19 testing facilities to assess the true scale of the pandemic.
- The lockdown would provide the Centre government time and capacity to boost vaccine’s domestic production.
Way forward
- Firstly, government should avoid shut out employment and services completely. Home delivery services and some vending should be permitted.
- Secondly, the state government should ensure proper social distancing during ration distribution. Online payment for ration and consumer goods and doorstep delivery can be used.
- Thirdly, facilitation of Travel for emergencies must happen without harassment.
- Fourthly, people should focus on wearing quality good masks, keeping a safe distance, and avoiding big gathering
Source – The Hindu
Failure of Governance in India- Reason Behind the Pandemic Crisis
DCGI approves “2-deoxy-D-glucose (2-DG)” – an anti-COVID drug developed by DRDO
What is the News?
Defence Research and Development Organization(DRDO) has developed an anti-COVID drug named 2-deoxy-D-glucose(2-DG). Recently, the Drugs Controller General of India(DCGI) has approved this drug for emergency use.
About 2-deoxy-D-glucose (2-DG):
- 2-deoxy-D-glucose (2-DG) is an anti-Covid oral drug. It has been developed by the Institute of Nuclear Medicine and Allied Sciences (INMAS), a lab of DRDO in collaboration with Dr Reddy’s Laboratories(DRL).
How does a 2-DG drug work?
- The 2-DG comes in powder form in the sachet. One has to take it orally by dissolving the powder in water.
- The drug accumulates in the virus-infected cells. It, thereby, prevents virus growth by stopping viral synthesis and energy production.
- The selective accumulation of the drug in virally infected cells makes this drug unique.
Significance of this drug:
- The drug helps in the faster recovery of hospitalised patients. Further, it also reduces supplemental oxygen dependence.
- A higher proportion of patients treated with 2-DG also showed RT-PCR negative conversion in Covid-19 patients.
Source: Indian Express
Project MediCAB: Augmentation of Hospital Infrastructure
What is the News?
IIT Madras supported start-up Modulus Housing has developed a portable hospital unit called ‘MediCAB’.
About Project MediCAB:
- Project MediCAB is an initiative of the Office of principal scientific advisor and IIT Madras.
- Purpose: It is a portable hospital unit that has been developed to boost healthcare infrastructure by assisting states to set up COVID-19 extension hospitals.
- The project is a decentralized approach to detect, screen, identify, isolate and treat COVID-19 patients in their local communities through these portable microstructures.
- Features:
- The portable hospital is foldable. It is composed of four zones- an isolation room, a doctor’s room, a twin bed ICU, maintained at negative pressure, and a medical room/ward.
- The hospital can be easily assembled in eight hours by four people. Further, when folded the unit can be reduced five-fold which makes it very cost-effective for transportation.
- Significance: Innovations such as MediCAB will help in boosting the healthcare infrastructure in India as it can be rapidly transported. The hospital can be deployed at any place and at any time.
Source: DDNews
Ayush Ministry launches nationwide campaign for “AYUSH 64” & “Kabasura Kudineer”
What is the News?
The Ministry of Ayush has launched a massive nationwide campaign to distribute two key products. One is the Ayurvedic drug AYUSH 64. The other is the Sidha drug Kabasura Kudineer. Both will provide benefit to the vast majority of out of hospital Covid-19 patients.
About Ayush 64:
- Firstly, Ayush-64 is a polyherbal Ayurvedic Drug (i.e. use of more than one herb).
- Secondly, the drug was developed by the Central Council for Research in Ayurvedic Sciences(CCRAS). CCRAS is the apex body for research in Ayurveda under the Ministry of Ayush.
- Thirdly, the drug was originally developed in 1980 for the management of Malaria.
- Fourthly, However, this drug has now been repurposed for Covid-19.
- Fifthly, the ingredients of this drug showed notable antiviral, immune-modulator, and antipyretic(reducing fever) properties.
- Sixthly, the drug can be useful for the treatment of asymptomatic, mild, and moderate COVID-19 infection cases.
About Kabasura Kudineer:
- Kabasura Kudineer is a Siddha formulated drug. It has been found to be useful in the treatment of asymptomatic, mild, and moderate COVID-19 infection cases.
- Siddha is a traditional medicine originating in South India. It is one of the oldest systems of medicine in India.
Source: PIB
“Black Fungus Infection” Cases in Covid Patients
What is the News? Doctors in Delhi are witnessing a rise in cases of Covid-19 induced Black Fungus Infection.
About Black Fungus Infection:
- Firstly, Black Fungus infection is also known as Mucormycosis (previously called zygomycosis).
- Secondly, it is a serious but rare fungal infection caused by a group of molds called mucormycetes. These molds are present naturally in the environment.
- Thirdly, mucormycosis mainly affects people who have health problems or take medicines that lower the body’s ability to fight germs and sickness.
- Fourthly, ymptoms of the disease are face numbness, nose obstructions on one side, swelling in the eyes, or pain.
- Fifthly, the infection can occur in almost any part of the body. However, the infection is not contagious. This means that it cannot transmit between people or between people and animals.
- Sixthly, treatment of this infection is possible with prescription antifungal medicine. If not detected early, the infection can be fatal. It can also lead to loss of vision or jaw in others.
Note: Use of steroids in the treatment of Covid-19 infection plus diabetes as co-morbidity could be the reason for a rise in the number of black fungus infections again.
Source: Indian Express
Reason behind Covid Vaccine Shortage Crisis
Synopsis: Lack of firefight and planning are the main reasons responsible for the current Covid vaccine shortage crisis. The center needs to put in some extra efforts to address the challenges.
What are the reasons for the current Covid crisis?
- First, the delayed decision to make the vaccine available in the open market. Though now the government has allowed recently, the withdrawal of the price cap on vaccines can lead to a disparity among states to ensure universal vaccination for its citizens.
- The Indian-made Covaxin, whose distribution earlier was free, will now cost Rs 400 to the states and Rs 1,200 to private hospitals.
- The financial position of many states is so weak that they can hardly buy two doses for every person at the rate of Rs 400 per vaccine.
- Further, removal of price cap may lead to Exorbitant profiteering at the cost of people’s lives.
- Second, inadequate availability of vaccines across the country due to lack of planning. This has delayed our fight against Covid pandemic. For example, Maharashtra has announced a stop to vaccinations for three days.
- Further, there were no steps taken to increase their availability. While other countries such as the US and EU advanced funding to companies researching the vaccine, India did nothing.
- The US and the EU also booked 40 crore doses and 80 crore doses respectively in advance. While India placed its first order of vaccine in January 2021 and that too only for 1.60 crore doses. (less than 1 percent of its population).
- Third, lack of vision from our authorities to ensure ample availability of oxygen by anticipating the possibility of the second wave.
- Fourth, Lack of access to live-saving drugs due to profiteering by companies and middlemen.
Further steps to take?
- One, to provide universal vaccination, the Centre should bear the cost of vaccination. Also, a one-time tax can also be levied to mobilize funds.
- Two, the state must adopt a zero-tolerance policy towards the black marketing of medicine. Further, Remdesivir should be procured and disbursed directly based on the assessment of the Disaster Management Group.
- Three, micro-planning at the local level should be carried out and a website for every district to dispense complete information from beds to oxygen, medicines, and ventilators should be enabled.
Source: Indian Express
- First, the delayed decision to make the vaccine available in the open market. Though now the government has allowed recently, the withdrawal of the price cap on vaccines can lead to a disparity among states to ensure universal vaccination for its citizens.
Use of CT scan for testing Covid is not Correct
Synopsis: The available data and the risk factors suggest that the widespread use of CT scans in diagnosing infectious diseases needs to be sidelined.
Background
- There are mainly three reasons why tests in clinical medicine are performed.
- Diagnosis: To identify the disease
- Etiognosis: To identify the causative factor of the disease.
- Prognosis: To find out the future development of a particular disease.
- In this context, the use of computerised tomography (CT) scans for COVID does not satisfy all the above criteria, for an accurate diagnostic test.
Validation on the effectiveness of CT scan test for Covid
- First, CT scans are not accurate enough to diagnose COVID-19. For instance, according to a study by The Cochrane, CT scan can accurately diagnose COVID-19 in about 88% of individuals with a positive RT-PCR.
- Since an RT-PCR itself misses 30% of people who have COVID-19, a chest CT is likely to diagnose only 62% of all individuals having COVID-19. It makes it a relatively inaccurate test for diagnosis.
- Second, CT scans are also not accurate enough to identify the causing factor of the disease (Etiognosis). For instance, according to a study by The Cochrane, radiologists have mislabelled 20% of those who did not have the disease as having COVID-19.
- This has serious consequences on an individual’s health.
- One, the real causative factor for the disease is left undetected.
- Two, individuals are subjected to unwanted psychological stress.
- This has serious consequences on an individual’s health.
- Third, using a CT scan to identify the future course of the Covid disease is also unlikely. For instance,
- A CT scan can only show the infection in the lungs at that particular point in time.
- This suggests that a CT is unlikely to give a physician more information than a simple tool such as an oximeter.
- Finally, the risks involved in getting a CT of the chest done are high.
- According to a study published by The New England Journal of Medicine, in 2007, 4% of all cancers in the United States may be attributed to the radiation from CT studies.
- Also, apart from the risk caused to individuals, there are risks to radiology technicians, staff, and doctors.
- Further, there is a high risk of transmission of the virus at such centers. This is because CT scans are needed to be kept in closed air-conditioned spaces.
Way forward
- For diagnosis of Covid, RT-PCR tests, which have higher accuracy compared to CT scans, can be done.
- Individuals should make an informed decision by evaluating the potential risks involved in getting the CT done.
- Further, patients with two negative RT-PCR swabs tests need to be evaluated for the possibility of other lung diseases
Source: The Hindu
- There are mainly three reasons why tests in clinical medicine are performed.
“AYUSH 64” Ayurvedic Drug Govt is Recommending for Mild Covid-19
What is the News?
The Ministry of Ayush has announced that it has taken steps to increase the production of AYUSH 64 across the country to treat mild to moderate cases of coronavirus infections.
About Ayush-64:
- Ayush-64 is an Ayurvedic drug developed by the Central Council for Research in Ayurvedic Sciences(CCRAS), the apex body for research in Ayurveda under the Ministry of Ayush.
- The drug was originally developed in 1980 for the management of Malaria.
- However, this drug has now been repurposed for Covid-19 as its ingredients showed notable antiviral, immune-modulator, and antipyretic properties.
- The drug can be useful for the treatment of asymptomatic, mild, and moderate COVID-19 infection cases.
- The drug was found to significantly enhance the recovery in terms of disease symptoms and severity. It also has significant beneficial effects on general health, fatigue, anxiety, stress, appetite, general wellbeing, and sleep.
- Ayush-64 is a polyherbal formulation i.e. use of more than one herb. The development of the drug was in compliance with all regulatory requirements of pharmacopeial standards by the Central Council for Research in Ayurvedic Sciences (CCRAS)
Source: PIB
“SUTRA model” has flaws in predicting the pandemic – Scientists
What is the News?
The Indian government backed the SUTRA model to chart the Covid-19 trajectory in the country. But few scientists have raised concerns over the SUTRA model.
SUTRA Model:
- SUTRA stands for Susceptible, Undetected, Tested (positive) and Removed Approach.
- Purpose: SUTRA is a mathematical model. It is used for charting the trajectory of COVID-19 in the country.
Parameters: The model uses three main parameters to predict the course of the pandemic:
- Beta or contact rate: This measures how many people an infected person infects per day. It is related to the R0 value. R0 is the number of people an infected person spreads the virus over the course of his/her infection.
- For example, if a disease has an R0 of 18. Then a person who has the disease will transmit it to an average of 18 other people
- Reach: It is a measure of the exposure level of the population to the pandemic.
- Epsilon: It is the ratio of detected and undetected cases.
Why Scientists are calling the SUTRA model flawed?
- The SUTRA model predicted that the peak Covid-19 burden in India will be 0.6 million symptomatic infections by early 2021. Further, the model predicts fewer than 50,000 active cases from December. Thus, it creates a perception that the second wave of the pandemic was highly unlikely in India. But this is not true.
- The model relied on too many parameters. Also, these parameters got recalibrated whenever its predictions broke down.
- Further, the model was ‘calibrated’ incorrectly. It relied on a Sero Survey conducted by the ICMR in May 2020. The survey said 0.73% of India’s population may have been infected at that time.
What did the scientists working on the SUTRA model said?
- Scientists said that a mathematical model can only predict the future. That too will work as long as the virus dynamics and its transmissibility don’t change substantially over time.
- So the scientists said that is not the case with the Covid-19. The virus has been changing very rapidly. Hence, any prediction for Covid-19 must be continually readjusted.
Source: The Hindu
New Malaria Vaccine Can be a Game Changer in Curtailing Malaria
Synopsis:
Phase 2b clinical trials of R21/Matrix M (a new malaria vaccine) have shown the efficacy of 77%. It is a new version of RTS, S — another candidate against malaria. Experts believe that this new version could be a game-changer in curtailing the spread of malaria across the globe, especially during pandemic times.
Contents
Background:
- The results of phase 2b clinical trials of R21/Matrix M were published recently in the Lancet Journal.
- The new malaria vaccine showed an efficacy of 77%, much higher than its previous version named RTS,S.
About Malaria:
- Firstly, it is caused by the bite of the female Anopheles mosquito if the mosquito itself is infected with a malarial parasite.
- Secondly, there are five kinds of malarial parasites — Plasmodium falciparum, Plasmodium vivax (the commonest ones), Plasmodium malariae, Plasmodium ovale, and Plasmodium knowlesi.
- Thirdly, according to the World Malaria Report 2020, cases of Malaria in India dropped from about 20 million in 2000 to about 5.6 million in 2019.
- Fourthly, globally 39 countries have declared themselves Malaria free.
- As per WHO, a country can be declared malaria-free when it reports zero indigenous cases of malaria for 3 or more years.
About the Previous Version:
- RTS, S has been in development for more than 30 years. It is a joint work of Walter Reed Institute of Research, GlaxoSmithKline, and Bill and Melinda Gates Foundation with the PATH Malaria Vaccine Initiative.
- It targets the liver stage protein of the Plasmodium falciparum life cycle.
- Thus, it stops the Plasmodium falciparum malaria parasite from entering the liver thereby preventing the subsequent deadly blood stages.
- To date, it is the only vaccine to reduce malaria in children. However, it doesn’t have high efficacy.
About the new version:
- R21/Matrix M is a modified version of RTS, S.
- Scientists at the University of Oxford have been developing it for the last 6-7years. Serum Institute of India is manufacturing it.
- The vaccine trial began in 2014-15 on 450 children in Burkina Faso.
- The result of the phase 2b trial showed a 77% efficacy. This made it the first vaccine to reach WHO’s goal of at least 75% efficacy.
Need of New Malaria Vaccine:
- High Incidence of Malaria: In 2019, there were an estimated 229 million cases of malaria and 409 000 malaria-related deaths in 87 countries. In the same year, India witnessed 5.6 million cases.
- Under 5 children in sub-saharan Africa accounted for approximately two-thirds of global deaths.
- Greater Hardships posed by Pandemic: As per a WHO survey, approximately one-third of countries around the world reported disruptions in malaria prevention, diagnosis and treatment services during the first quarter of 2021.
- Disruptions occurred as people were unable or unwilling to seek care in health facilities.
- Further lockdowns and restrictions on the movement led to delays in the delivery of insecticide-treated mosquito nets.
What’s next?
- Serum Institute of India and US vaccine maker Novavax have begun the process of phase 3 trials in 4 African countries.
- This would assess large-scale safety and efficacy in 4,800 children aged five to 36 months.
- The success of the trial would enable bulk production of the vaccine that would help curtail malaria across the globe.
Source: Indian Express
One Health Approach – Significance and Steps Taken by India
Synopsis:Covid-19 has once again shown the degree of chaos that can be spread by zoonotic diseases. This gives India an opportunity to work on the One Health approach.
Contents
Background
- In 1856, the father of modern pathology (Rudolf Virchow) observed that there are no dividing lines between animal and human medicine.
- The Covid-19 pandemic once again highlighted the interconnectedness of the systems.
- The havoc caused by the pandemic induced the experts to sensitize countries towards the ‘One Health’ approach on the occasion of World Veterinary Day (April 24th).
What is the One Health Approach?
- Firstly, it is a collaborative, multisectoral, coordinated, and transdisciplinary approach. It recognizes the interconnection between people, animals, and the environment.
- Secondly, it calls for working at the local, regional, national, and global levels with the goal of achieving optimal health outcomes.
Need for focusing on ‘One Health’:
- High Prevalence of Zoonotic Diseases: More than two-thirds of existing and emerging infectious diseases are zoonotic. Experts believe that there are more than 1.7 million viruses circulating in wildlife, and many of them are likely to be zoonotic.
- It is an infectious disease that jumps from animal to humans.
- Anthropozoonotic infections get transferred from humans to animals.
- Transboundary impact: The transboundary impact of viral outbreaks such as the Nipah virus, Ebola, Severe Acute Respiratory Syndrome (SARS), etc. were alarming for the world. It has made it imperative for the world to focus on one health.
- Huge Economic Cost: Zoonotic diseases place a heavy burden on the economy of countries.
- For instance, the WHO estimates that rabies (also a zoonotic disease) costs the global economy approximately $6 billion annually.
India and one health approach:
- India’s ‘One Health’ vision derives its blueprint from the agreement between the tripartite-plus alliance towards ‘One World, One Health’.
- The alliance includes:
- the Food and Agriculture Organization of the United Nations (FAO),
- the World Organization for Animal Health (OIE),
- the World Health Organization (WHO) and the United Nations Environment Program (UNEP).
Steps taken by India towards ‘One Health’:
- The country established a National Standing Committee on Zoonoses in the 1980s.
- The Department of Animal Husbandry and Dairying (DAHD) has launched several schemes to mitigate the prevalence of animal diseases since 2015.
- For instance, under the National Animal Disease Control Program, 13,343 crore rupees have been sanctioned for Foot and Mouth disease and Brucellosis control.
- DAHD has partnered with the Ministry of Health and Family Welfare in the National Action Plan for Eliminating Dog-Mediated Rabies.
- Further DAHD will soon establish a ‘One Health’ unit within the Ministry.
- A Center for One Health will soon be established at Nagpur.
- Efforts are being made to revamp programs that focus on capacity building for veterinarians.
- The government is also upgrading the animal health diagnostic system such as Assistance to States for Control of Animal Diseases (ASCAD).
Challenges hindering the success of one health approach:
- Veterinary manpower shortages make the early detection of zoonotic diseases difficult.
- Lack of information sharing between human and animal health institutions
- Inadequate coordination on food safety at slaughter, distribution, and retail facilities
Way Forward:
- The focus should be on increasing investments and augmenting awareness generation towards the’One Health’ approach.
- There must be the integration of existing animal health and disease surveillance systems.
- For instance, the Information Network for Animal Productivity and Health, and the National Animal Disease Reporting System can be integrated.
- The government needs to formulate best-practice guidelines for informal market and slaughterhouse operations. This would improve inspections, disease prevalence assessments, etc.
- Further, it must create mechanisms to operationalize ‘One Health’ at every stage from top to grassroots level.
Source: The Hindu
Managing Vaccine Shortage by Proper Gap Between Vaccinations
Synopsis: To achieve universal vaccination, India needs to work on a few out-of-the-box solutions for vaccine shortage. For example, increasing the gap between vaccination effectively.
Contents
Introduction:
The New Vaccine Policy aims to vaccinate people above 18 years. The Policy came into force on May 1. But a few states have postponed the vaccination program citing a shortage of the vaccine.
Vaccine shortage:
- According to the Co-WIN portal, India is producing roughly 2 million vaccines a day. However, the number of vaccines administered daily is roughly 2.3 million to 2.5 million. So, technically the production capacity falls below even the daily requirement.
- As of April 29, India’s 9.1 % of the population received one dose of vaccine. Similarly, only 1.9 % of the population received both doses.
- Since India announced the new vaccination policy, the demand for vaccines has increased three times, but the supply of vaccines remains the same.
How India expected to tackle the vaccine shortage?
- At present, India is expecting a few million doses of Russian vaccine Sputnik.
- Similarly, Covishield vaccine maker Serum Institute of India also going to improve their scale-up production to 100 million doses per month soon.
- Also, the Covaxin manufacturer Bharat Biotech is expecting to scale up the production to 50-60 million doses a month.
Despite these developments, the next few month’s production is unlikely to go beyond 150 million doses a month.
Interval between two doses:
- Covishield: Phase 3 trials of the Covishield vaccine found out that the second dose offered after 12 weeks of the first dose will provide the best result and protection. So the best option to take the second dose of vaccine is 12 weeks for Covishield.
- However, due to urgency, second doses administered after six to eight weeks also improved efficacy over time.
- Covaxin: The second dose of Covaxin can be taken four to six weeks after the first.
Present condition of vaccination in India:
At present India’s routine immunisation programmes for children are administered at a four-week gap in India. But globally they follow an eight-week gap. The reason for the lower gap between vaccination in India is due to,
- Operational reasons: India’s distribution of vaccines in two phases with a long gap might create a delay in vaccination.
- Low coverage: If the gap between vaccination is increased then people might not vaccinate at the correct time.
Suggestions to avoid vaccine shortage:
- India should increase the gap for Covishield to 12 weeks. This is because India needs to control the progress of the pandemic. The Covishield trials have shown that the higher the gap, the greater the proven efficacy. Furthermore, it has other advantages as well. Such as,
- Increasing the gap between vaccination will give some time to manufacturers to produce the vaccine.
- It allows more people to take at least one shot of the vaccine. Immunologically, it is understood that even one dose can activate the immune system. Here, the vaccine will make the natural infection a sort of booster infection and protect people for a longer time than the non-vaccinated individual.
- Like the US, India also needs to ensure evolving guidelines on vaccination. This will ensure more vaccination of single dose.
- The United States’s Centers for Disease Control and Prevention(CDC) initially came up with a vaccination gap of three-month. Later the CDC reduced this gap to one month.
Source: The Hindu
Supreme Court observations on “seeking medical help for COVID-19”.
What is the News?
The Supreme Court has said that there should not be any coercive action against any citizen. This is especially for citizens who are putting out emergency calls on social media for seeking medical help for COVID-19.
Background:
- Uttar Pradesh government had recently ordered strict civil and criminal action against citizens. This is for making false appeals on social media for seeking help for COVID-19
- But against the UP government order, the Supreme Court recently issued the following observations.
Key observations on seeking medical help for COVID-19:
- The Supreme Court has warned the State governments and the police against taking any action on the spread of information from the citizens affected by Covid-19.
- Further, the court also warned the government and police for taking actions on the request of help through social media from citizens affected by COVID-19.
- The court has said that any move to punish citizens actions on social media to seek help for oxygen cylinders, COVID-19 drugs, beds and hospitals would attract contempt of court action.
- Further, the court has also referred that the free flow of information during the 1970 famine enabled the government to tackle problems effectively. But the restriction of information during the 1918 pandemic created troubles for the government.
- Lastly, the court has also told the States that this was a time of great crisis. Hence, empathy and action should be the rule of the day.
Source: The Hindu
“Immunisation Agenda 2030 or IA2030” launched on World Immunisation Week.
What is the News?
Global agencies like the World Health Organization (WHO), UNICEF, GAVI and others have launched the Immunisation Agenda 2030 or IA2030 during World Immunisation Week.
Contents
World Immunisation Week:
- It is celebrated every year in the last week of April. It aims to promote the use of vaccines to protect people of all ages against disease.
- The theme for 2021: Vaccines bring us closer.
About Immunisation Agenda 2030(IA2030):
- The Immunisation Agenda 2030(IA2030) sets an ambitious, overarching global vision and strategy for vaccines and immunisation for the decade 2021–2030.
- Vision: IA2030 envisions “A world where everyone, everywhere, at every age, fully benefits from vaccines for good health and well-being.”
- Based on: The IA2030 is based on the learnings from Global Vaccine Action Plan(GVAP). IA2030 has a target to address the unmet targets of the GVAP.
- The GVAP was developed to help realize the vision of the “Decade of Vaccines(2011–2020)”.
- GVAP was launched in 2012 with the aim to prevent millions of deaths by 2020. The GVAP aims to achieve this through more equitable access to vaccines for people in all communities.
- Core Principles: The IA 2030 strategy is guided by four core principles: it puts people in the centre. The strategy is led by countries. They will implement the strategy through broad partnerships and data.
Key Features of Immunisation Agenda 2030:
- The IA2030 will ensure the benefits of immunisation are shared equitably among and within countries.
- It will focus on a bottom-up approach. This is in contrast to the GVAP’s ‘top-down’ approach.
- It will give priority to people particularly, the most marginalised communities living in fragile and conflict-affected settings. It also gives priority to mobile populations such as people moving across borders.
Targets:
- Firstly, to avoid 50 million vaccine-preventable infections in this decade as part of this immunization program.
- Secondly, to reduce the number of zero-dose children by 50%. The programme hopes to do this by extending immunisation services to 13 million such children.
- Zero-dose children are those who have received no vaccines through immunisation programs.
- Thirdly, to achieve 90% coverage for essential vaccines given in childhood and adolescence
- Fourthly, completing 500 national or subnational introduction of new or under-utilized vaccines. This includes vaccines such as COVID-19, rotavirus, or human papillomavirus(HPV), etc.
Significance:
- The agenda will help by contributing to the achievement of the UN-mandated sustainable development goals or SDGs, specifically SDG3. SDG 3 aims to“Ensure healthy lives and promote well-being for all at all ages”.
Source: Down To Earth
“Emergency Financial Powers” to Armed Forces to tackle pandemic
Contents
What is the News?
The Union defence ministry has granted emergency financial powers to the country’s armed forces. This is to empower their efforts against the Covid-19 pandemic.
About Emergency Financial Powers to Armed Forces:
- The Emergency Financial Powers will allow armed forces to establish and operate quarantine facilities and hospitals.
- Besides, it will also help them to operate and procure equipment and resources to perform any required urgent tasks.
- The armed forces will be able to perform all these operations without the usual clearances.
Who has these powers?
- Vice Chiefs of the armed forces including the Chief Of Integrated Defence Staff, Chairman Chiefs of Staff Committee(CISC) and General Officer Commanding-in-Chiefs(GOC-in-Cs) have these powers. Further, similar equivalents of all three Services have been given full powers.
- Further, Corps Commanders and Area Commanders have been delegated powers up to ₹50 lakh per case
- Also, Division Commanders, Sub Area Commanders and equivalents have been delegated powers up to ₹20 lakh per case.
Duration:
- These powers have been devolved initially for three months from May 1 to July 31, 2021.
- These are in addition to the emergency powers delegated to the medical officers of the armed forces.
Other Organizations contribution during the pandemic:
- Defence Research and Development Organisation (DRDO) is arranging big size oxygen cylinders for fulfilling requirements of different hospitals.
- The Navy has sent a 76-member medical contingent from five Naval hospitals to the 900-bed COVID hospital in Ahmedabad. This is to bolster the availability of trained manpower.
- The Cantonment Boards have extended support to civil administration in various parts of the country to fight over the increase in Covid-19 cases.
Source: The Hindu
How Government Regulate the Prices of Vaccines and drugs?
Synopsis: The Supreme Court recently reminded the government of its powers to regulate the pricing of vaccines and drugs.
Contents
Introduction:
The Supreme Court has raised the issue of differential pricing for Covid-19 vaccines for the center and states. It directed the central government to clarify in its affidavit the basis and rationale for pricing.
How does the government regulate the pricing of drugs?
- Firstly, the Government of India regulates the pricing of essential drugs through its Essential Commodities Act, 1955.
- Secondly, under Section 3 of the Act, the government has enacted the Drugs (Prices Control) Order. The DPCO lists over 800 drugs as “essential” in its schedule. Government caps the prices of medicines in this list.
- Thirdly, the capping of prices is done based on a formula. This formula is worked out in each case by the National Pharmaceutical Pricing Authority (NPPA). (The NPPA was set up in 1997).
What prices the government cannot regulate?
- Regulation through DPCO is not applicable for patented drugs or fixed-dose combination (FDC) drugs.
- For example, the price of the antiviral drug remdesivir. The government is not regulating the prices of this drug even though it is in great demand to treat serious cases of Covid-19.
Various ways to regulate the pricing of vaccines:
Experts suggest the government can use few methods to control the pricing of vaccines. These are,
- The Patents Act,1970: The act has two key specific provisions that could be potentially invoked to regulate the pricing of the vaccine. The two provisions are:
- Section 100: It gives the central government the power to authorise anyone (a pharma company) to use the invention for the purposes of the government. Basically, this provision enables the government to license patents of the vaccine to specific companies. This is done to speed up manufacturing and ensuring equitable pricing.
- Section 92: It deals with compulsory licensing. It says that the government without the permission of the patent holder can provide license under the following situations:
- The circumstance of national emergency; or
- The circumstance of extreme urgency; or
- Case of public non-commercial use.
- After the government issues a notification under Section 92 the pharma companies can approach the government for a license. They can start manufacturing the patented drug by reverse-engineering the product.
- Epidemic Diseases Act,1897: It is another legal route suggested by experts to regulate the pricing of vaccines.
- Firstly, Section 2 of the Act: It empowers State Governments to take special measures and prescribe regulations during the outbreak of an epidemic disease.
- Secondly, if the State Government thinks that other Acts are insufficient, then the state may issue a public notice to prescribe temporary regulations for the public/class of persons to follow.
- Thirdly, the undefined powers under section 2 can be used to take measures to regulate pricing. However, the law is not sufficient for its implementation. Punishment for violation of orders under section 2 is nominal, which restricts its implementation.
- Fourthly, violation of the Act is penalised under Section 188 of the Indian Penal Code. It says that any person who disobeys an order given by a public servant will be punished with imprisonment up to 1 month. If such disobedience causes danger to human life, the term may extend to six months or a fine that could extend up to Rs 1,000.
Way forward:
The government has various ways to control the pricing of the vaccine. So the government has to resolve the challenges with the new vaccination policy. Further, to achieve universal vaccination for Covid-19 the government has to take these necessary steps.
Source: The Indian Express
How to Prevent 3rd Wave of Covid-19?
Synopsis: Mass vaccination will be the best solution to contain Covid19. However, to prevent the 3rd Wave of Covid-19 we need to adhere to measures such as mask-wearing, physical distancing, hand hygiene.
Contents
Background
- International experience from other countries such as the UK, South Africa, United States indicated to us about the possibility of recurrence of Second-wave in India.
- However, preparedness to tackle the second wave was largely ignored.
- There is a high possibility of a third wave once the second wave recedes. This is, if, we don’t take active measures to control the spread.
- Hence, India needs to plan effectively to contain the possibility of a 3rd wave.
How the possibility of a third wave can be Prevented?
- Mass vaccination is the right option. It will help achieve herd immunity and will bring the Pandemic under control.
- However, vaccinating the entire population will take a considerable amount of time due to the following challenges:
- Slow pace of vaccination,
- Inelastic vaccine supplies
- limited finances with State governments
- So, along with mass vaccination drive, India needs to follow other methods such as mask-wearing, physical distancing, hand hygiene, ban on mass gatherings to reduce community transmission. For instance,
- According to a study on Beijing households, face masks were 79% effective in preventing transmission when they were used by all household members.
- Similarly, according to the National Academy of Sciences, near-universal adoption of nonmedical masks in combination with complementary public health measures could reduce community spread.
How to persuade people to wear masks?
- An experimental study in Bangladesh provides an understanding of how to persuade people to wear masks voluntarily.
- According to the study by Mushfiq Mobarak of Yale University, the following interventions helped to increase the percentage of people using masks three-fold.
- Providing Free masks along with well-designed instructional material.
- Improvements in mask Quality. Masks should be comfortable to wear in hot and humid conditions, along with effective filters.
- Reminders from religious and community leaders and volunteers.
How India can replicate this model to Nudge Mask wearing?
- First, need to allocate budgetary resource for the cost of supplying free reusable masks.
- Second, we need imaginative and creative communication campaigns to explain the reasons for mask wearing as well as the right way to wear a mask.
- Third, community-level leaders, networks of health workers at the village and community levels should be involved in health campaigns.
If the country is to reduce the impact of future waves, it is essential that the above measures are put in place.
Source: The Hindu
Issues in COVID-19 Management Guidelines
Synopsis: The Health Ministry’s COVID-19 management guidelines show disregard for evidence, pricing, cost-effectiveness, and social relevance.
Introduction
The Health Ministry released its first COVID-19 management guidelines about a year ago. This guideline included hydroxychloroquine for the treatment of Covid-19. It led to its panic buying.
Later, in a year, multiple studies rejected this claim. However, Health Ministry’s guidelines released on April 22 still prescribes hydroxychloroquine.
What are the other issues in the COVID-19 management guidelines?
- First, disregard for evidence. For example,
- The ICMR after several trials has revealed that the use of convalescent plasma does not save the lives of those with COVID-19. At best the plasma can prevent progression to severe disease in mild cases. Yet, convalescent plasma is mentioned in the Ministry’s guidelines.
- Ivermectin, a drug used against parasites, has been recommended in the guidelines. However, World Health Organization (WHO) recommended against its routine use.
- Second, it also overlooks the importance of pricing and cost-effectiveness. For example,
- One, there is supply-demand mismatch in Remdesivir due to black-marketing. It led to an increase in the cost of hospitalization due to the steep price of the drug in the black market.
- Two, budesonide inhalers have been included as an option for mild patients based on the results of two clinical trials. Though it does not result in saving lives or reducing hospital admissions.
- This will result in a lack of access to inhalers for patients with asthma and chronic obstructive pulmonary disease (COPD) due to panic buying by Covid patients.
What changes are needed?
- First, guidance on drugs being used for COVID-19 should be included. This is because, many unsafe drugs such as Azithromycin, Doxycycline, are being prescribed.
- Second, the most efficacious antivirals in COVID-19, the monoclonal antibodies should be mentioned.
- Third, the COVID-19 treatment guidelines should focus more on oxygen delivery, steroids, and anti-coagulants.
Rewriting the guidelines based on the available evidence, and keeping cost-effectiveness and the social relevance of the Indian health system should be the way forward.
Source: The Hindu
- First, disregard for evidence. For example,
“Trachoma” eliminated from Gambia as a public health problem
What is the News?
The World Health Organization (WHO) recently validated the Gambia for its elimination of trachoma as a public health problem.
- Overall, this makes Gambia second country after Ghana to achieve this milestone in the WHO’s African Region. (Please note that, Africa & WHO’s African region are not the same)
- Ghana did it in 2018.
- This also makes Gambia second country after Côte d’Ivoire to eliminate a Neglected Tropical Disease (NTD) in 2021.
- Côte d’Ivoire successfully eliminated human African trypanosomiasis, also known as “sleeping sickness”, as a public health problem, becoming the second African country after Togo to be validated by the World Health Organization (WHO).
About Trachoma:
- Firstly, Trachoma is a neglected tropical eye disease. It is caused by the infection due to the bacterium Chlamydia trachomatis.
- Secondly, Transmission: Trachoma spreads through personal contact (via hands, clothes or bedding). It also transmits by flies that contact the discharge from an infected person’s eyes or nose.
- Thirdly, Vulnerable Group: Trachoma mainly affects children. It is becoming less common with increasing age.
- Fourthly, Impact: Repeated infections in childhood lead to scarring of the inner side of the upper eyelids. This will result in the inward turning of the eyelid margin. This painful condition is known as trachomatous trichiasis. If left untreated, this condition can result in visual impairment and blindness.
Global Elimination of Trachoma by the year 2020 (GET2020).
- The WHO in 1996 launched the Global Elimination of Trachoma by the year 2020 (GET2020).
- Purpose: It supports countries to implement the SAFE strategy in Trachoma elimination. Further, it also strengthens national capacity through epidemiological assessment, monitoring, surveillance, project evaluation and resource mobilization.
SAFE Strategy:
- WHO adopted the SAFE strategy in 1993. Its mandate is to provide leadership and coordination to international efforts in eliminating trachoma as a public health problem. The SAFE strategy also reports on the progress towards that eliminating Trachoma.
Source: WHO
- Overall, this makes Gambia second country after Ghana to achieve this milestone in the WHO’s African Region. (Please note that, Africa & WHO’s African region are not the same)
Understanding Herd Immunity and Rising Covid Cases in India
Synopsis: Herd Immunity can’t be attained solely by a rise in Covid-19 positive people. It is also dependent on the absolute number of susceptible individuals and the rate of transmission of the virus.
Contents
Background:
- The data from various serological surveys in metro cities shows high immunity levels in the metro cities. As per them, Covid-19 had touched:
- 56% of population in Delhi by January 2021.
- 75% in some slums in Mumbai in November 2020.
- About 30% in Bengaluru in November 2020.
- This indicates attainment of herd immunity but still, the Covid-19 cases are rising.
What is Herd immunity?
- It is a stage of an epidemic in which some members of a population group remain protected from infection.
- This happens as the majority of those around them have already developed immunity either through vaccination or prior infection.
What is a Serological Survey?
- It is a blood test that seeks to assess the prevalence of disease in a population by detecting the presence of specific antibodies against the virus.
- The test only indicates past infections (which triggered an immune response) and is not used to detect active infections.
Understanding the current spread: –
- The number of daily cases depends on 3 factors:
- Number of infectious people in the population (those who have developed immunity)
- Number of susceptible individuals (those who are not infected)
- Rate of transmission of the virus – It depends on the nature of the virus and the extent of contact between individuals.
- As per experts, the cases are rising due to:
- Increased interaction and contact among the population since February 2021. This increased the virus in circulation and led to increased cases in the susceptible population.
- The high absolute number of Susceptible population among which the virus is circulating. For instance, in this second wave, the affluent class and youth are getting more infected who were less targeted in the first wave.
- Therefore, solely relying on the first factor to check the virus spread will not yield rational results.
Future Trajectory:
- Firstly, a decline would be observed if it is proved that the virus (even the new strain) is infecting the susceptible population more.
- Secondly, a greater surge could occur if the new strain is again infecting the previously infected individuals. This scenario would also question the efficacy of our vaccines in fighting the virus. Source: Indian Express
- The data from various serological surveys in metro cities shows high immunity levels in the metro cities. As per them, Covid-19 had touched:
The New Vaccine Strategy May Widen Inequality
Synopsis: The new vaccine strategy fails to address the issues of affordability and accessibility. It may contribute to widening inequality in access to health care.
Background
- Recently, the Centre revised its vaccine strategy to accelerate its vaccination drive to bring the Second wave Covid 19 under control.
- The revised strategies are,
- One, Vaccine coverage is now been extended to the entire adult population i.e., Population above 18 years of age.
- Two, vaccine market has been deregulated. Vaccine manufacturers can now sell 50% of their vaccine production to State governments and private hospitals, and the prices can be higher than the price fixed by the government.
- Three, a grant of ₹45 billion to the two vaccine manufacturers, the Serum Institute of India (SII) and Bharat Biotech, to boost their capacities. Note, there has been no formal announcement of the grant till now.
- However, the newly revised vaccine strategy fails to address many critical issues, such as Universal vaccination, responsibility of a welfare state, affordable life-saving drugs etc.,
What are the issues with the new vaccine strategy?
- First, issue of demand-supply mismatch due to the expansion in the coverage of the vaccine-eligible population.
- India faces vaccine shortages mainly due to the following issues,
- One, lack of vision led to the policy of ‘Vaccine diplomacy’. India promised exports of vaccines to 95 countries, mostly in Africa and Asia instead of securing Vaccines for its own population.
- Two, the inability of Indian vaccine manufacturers to increase production capacity because of the following two reasons,
- Lack of access to essential raw materials to produce vaccines from the U.S. a few days back, the US restricted the Export of essential materials under its Defense Production Act.
- Lack of financial capacity to expand vaccine production. Vaccine manufacturers are requesting a grant of ₹30 billion from the government.
- Second, the issue of affordability and accessibility to vaccines.
- The center had shifted its responsibility to states to procure vaccines for the population aged above 18 years to 45 years.
- Whereas the centre will support vaccination only for people above 45 years, and healthcare workers, and frontline workers.
- Further, the government has not fixed the prices of vaccines that are to be sold to the state government and private agencies. This has given rise to the following issues,
- One, increase in vaccine pricing due to fragmentation of the market into three layers namely, central, State, and private hospitals. Earlier, the role of center as a single central procurement agency helped in limiting the price of vaccines.
- Two, it may result in inequitable access to vaccines across States owing to disparities among states’ financial capacity. Further, many State governments may find it difficult to procure the required number of vaccine doses to meet the demands of the targeted population.
- Third, the issue of public money involved in Vaccine production without considerable benefits to the society at large.
- The government provides ₹45 billion to the two vaccine producers in India for expanding their production capacities. It is questionable.
Way forward
We can tackle the issue of affordability of vaccines by ensuring a competitive market for vaccines. More open licensing for vaccine manufacturers to scale up production would enhance competition in the market. It would enable the vaccines to reach every citizen in the country.
Source: The Hindu
Universal vaccination in India : Challenges and way forward – Explained, Pointwise
Contents
- 1 Introduction
- 2 India’s vaccination policy so far
- 3 Salient features of India’s new vaccination policy
- 4 Other steps taken towards universal vaccination in India
- 5 Need for achieving universal vaccination in India
- 6 Challenges to universal vaccination in the Covid-19
- 7 Suggestions to improve universal vaccination in India
- 8 Conclusion
Introduction
The daily cases of Covid-19 infections are breaking new records. India is almost touching 4 lakh cases per day. Moreover, India’s health care infrastructure is also falling short of taking care of that many cases at once. Thus, the majority of experts are of the opinion that the only way out of this crisis is universal vaccination in India. It means the majority of the population should be administered vaccines to achieve a herd immunity.
India started its coronavirus vaccination drive almost three months ago. According to the data from the Ministry of Health and Family welfare, so far, India has vaccinated only 146 million people (less than 2% of the population has received both the doses). With the universal vaccination in mind, India recently released a new vaccination policy. But to vaccinate the remaining population, India has to face various challenges and need innovative solutions.
India’s vaccination policy so far
- India so far released three phases of vaccination policy
- The first three phases vaccinated healthcare workers, frontline workers, and those above the age of 45.
- The Centre procured the entire quantity of vaccines from manufacturers Serum Institute of India and Bharat Biotech(Covishield and Covaxin respectively). The centre then distributed them to states for vaccination.
- The states distributed the stock to government vaccination centres. These government centers administered the vaccine free of cost. Private hospitals charged recipients Rs 250 per dose.
Salient features of India’s new vaccination policy
The new vaccination policy is the fourth phase of India’s Covid-19 vaccination policy. Under this phase, there are few changes,
- Changes for Citizens:
- All adults over the age of 18 will be eligible for vaccination starting from May 1.
- Those eligible in the earlier phases can continue to get the free doses provided by the Government of India.
- Changes for distribution:
- Under the new rules, the Centre will automatically receive only 50% of vaccines produced by manufacturers. It will allocate these to states based on the extent of infection (active cases) and performance (speed of administration).
- The remaining 50% can be acquired by the states directly or by private hospitals and industrial establishments.
- The Centre will allow the imported, fully ready-to-use vaccines to be entirely utilised in the other-than-Government of India channel.
Other steps taken towards universal vaccination in India
- Electronic Vaccine Intelligence Network(EVIN): It is an innovative technological solution aimed at strengthening immunisation supply chain systems across the country. The EVIN shows real-time information on vaccine stocks and flows and storage temperatures across all cold chain points in the country. During the Covid-19 vaccination, the delivery system will use this EVIN solution.
- CoWIN platform and CoWIN App: It is a digitalised platform launched by the Ministry of Health and Family Welfare (MoHFW). It aims to help agencies to keep a track of the Covid-19 vaccination programme in real-time. Further, the app also allows Indian citizens to apply for a Covid-19 vaccine shot. The app also provides a QR based Certificate once the person is vaccinated.
- Further, India’s drug regulatory authority relaxed Imports restrictions on COVID-19 vaccines. Also, it approved the restricted use of vaccines, which are already approved for restricted use by the US in emergency situations.
Need for achieving universal vaccination in India
- Reducing daily caseload and eliminating Covid-19 altogether: At present India’s daily caseload is the highest in the world. India will soon register half a million cases each day. Universal vaccination will not only reduce the Covid-19 cases but also help India to achieve Covid-19 free status.
- Reducing infection to the vulnerable sections: Covid-19 infects senior citizens and people having comorbidity such as diabetes, blood pressure, etc. By vaccinating them India can prevent the life of countless individuals.
- Vaccines are the most effective health intervention against Covid-19: Universal vaccination in India will prevent various health intervention costs and economic cost of the Indian economy. Universal Vaccination will provide relief to
- Heavily burdened health infrastructure and health care professionals.
- The Covid-19 induced lockdown and associated economic losses, etc
- Can help to achieve herd immunity before universal vaccination: ‘Herd immunity is the indirect protection from an infectious disease if a population is immune either through vaccination or immunity developed through the previous infection. WHO supports achieving ‘herd immunity’ through vaccination. India needs to vaccinate around 70-75% of its population to achieve herd immunity. So, in process of Universal vaccination, India can reach herd immunity.
- Past Experience: Vaccination is the most effective way to reduce the impact of epidemics and pandemics. Universal vaccination in India has eliminated smallpox, polio. They also reduced the impacts of serious diseases including measles, mumps, rotavirus, etc. Further, India’s Universal Immunisation Programme (UIP) provides free vaccines against 12 life-threatening diseases, to 26 million children annually. But achieving a similar feat against the Covid-19 is not an easy task.
Challenges to universal vaccination in the Covid-19
The population of India is 1.3 billion. If the Covaxin and Covishield require two doses then India needs to vaccinate 2.6 billion doses across the nation. This itself is a challenge.
- Infrastructure challenges: This is one of the biggest hurdles in India’s universal vaccination programme against the Covid-19. This includes,
- Unequal distribution of cold storage facilities among states. For example, out of the 28,932 cold chain points, half are in the five southern states, Maharashtra and Gujarat. Whereas the eight states in the North and Odisha that account for over 40 per cent of the country’s population have only 28 per cent of the cold chain points.
- Other Infrastructure challenges: Both the Covaxin and Covishield requires to stored within a temperature of 2-8 degree Celsius. But the temperature-controlled boxes face challenges like frequent power supply interruption, lack of storage facilities at the remote location, etc.
Challenges related to affordability:
- Under the new vaccination policy, vaccine producers can sell 50% of their production directly to State governments and private hospitals. Further, the price of vaccines to state and private is not fixed.
- So, the private manufacturers may make a huge profit. This creates problems in affording the vaccine. This is evident as both vaccine manufacturers hiked their prices after the launch of the policy. For example, the Serum Institute mentions Rs 400 for state government and Rs 600 for private parties.
- Creation of Interstate equality: With the new vaccination policy states are responsible to vaccinate their people. With every state individually contacting the suppliers and bargaining price and supply, the discretion will be with the supplier. So this will create interstate inequities and make poorer states suffer more. This is a clear deviation from universal vaccination in India.
- Production-related challenges: The world’s largest vaccine maker, Serum Institute of Technology initially promised to supply 100 million doses of vaccines a month. But in reality, it only provided between 50 million to 60 million doses. India so far exported 66.4 million vaccines(As of April 27). With the government commitment to export vaccines along with the production gap, India is facing a delay in universal vaccination and facing a demand-supply mismatch.
The issue of vaccine hesitancy:
- In simple terms, it refers to delay in acceptance of vaccines or refusing vaccines despite their availability. In the past three months, only 40 percent of the 30 crore high-risk population were vaccinated, partly due to the initial vaccine hesitancy.
- There is a non-transparency of data related to the two vaccines proposed for use in the program.
- Furthermore, acquiring the data for under the 50s with comorbidities will also a challenging and difficult one.
- The Issue of Vaccine wastage: According to the RTI information, India has wasted more than 44 lakh of 10 crore doses(Till April 11). Tamil Nadu wasted over 12 percent, followed by Haryana (9.74%), Punjab (8.12%). Ideally, a vaccination centre must have 10 recipients to make optimal use of a single 10-dose vial. If the person is not available then that vaccine vial becomes a waste.
Suggestions to improve universal vaccination in India
- Conducting a detailed demand-supply analysis: To conduct a calibrated expansion of the eligibility criteria India needs to conduct a detailed analysis including the vaccine manufacturers’ real-time production capability, the supply chain delays, etc.
- Reducing vaccine hesitancy: The only way to counter that is to be open and honest about adverse effects and make available relevant information in the public realm. So, both the state government and the centre need to be more transparent in the Universal vaccination process.
- India can establish an independent team of experts under the aegis of the WHO to ensure adherence to recruitment standards, consent conditions, adverse event record management, compensation standards. This will improve public confidence and provide enough data for the future policies of the government.
- Encourage stakeholder participation: The government have to rectify the issues with the new vaccination policy with better stakeholder participation.
- Stakeholders should include not only state governments but also the local bodies that are struggling to control the pandemic.
- The government can ask private companies towards cartelisation: (It means the group of industry participants coming together to fix the price of products and services.). Since the foreign players are also producing vaccines, India can work towards the cartelisation efforts. This will fix the price of Covid-19 vaccines. In case of any failure in the process, India can invoke compulsory licensing and reduce the vaccine prices towards universal vaccination in India.
- The move towards zero-wastage: The state governments have to use each and every vaccine in an effective way. States wasting the vaccine can follow zero-wastage states like Kerala, West Bengal, Himachal Pradesh, etc. For example, the Kerala model includes the following steps. such as,
- Training health care staffs including ASHA workers towards the importance of vaccine usage
- Creating efficient inventory management for managing vaccines.
- Mobilise beneficiaries after they register for the vaccine.
Conclusion
“None of us will be safe until everyone is safe”, so the government has to take necessary steps towards universal vaccination. The need of the hour is a winning strategy against an epidemic that has drained us economically, socially and psychologically. The winning strategy is feasible when all the stakeholders come together to address the grievances.
Need to Accelerate Vaccination drive
Synopsis: Need to address the issues that issues that are hampering India’s Accelerate Vaccination drive on a priority basis.
Background
- Currently, India is vaccinating more than three million people per day and has administered more than 140 million doses of the vaccine as of April 25, 2021.
- However, only about 22.3 million (1.63% of India’s population), have been fully vaccinated, against a requirement of 70%-75% for achieving herd immunity. Whereas the Israel has vaccinated 55% of its population.
- India needs to address the issues that is hampering its efforts to push for accelerated vaccination drive.
Steps Taken to Accelerate India’s Vaccination drive?
- First, the eligible population for getting vaccinated has been expanded. Earlier Population above 45 years were prioritised, but now People above the age of 18 years were also allowed.
- Second, decision has been taken to make available vaccines in the open market and vaccines approved in other countries.
What are the issues that are hampering India’s accelerated vaccination drive?
Though many policy decisions were taken to augment vaccination drive, there are certain challenges that need to be addressed on priority basis,
- First, issue of delay over availability of imported vaccines due to policy restrictions.
- India’s drug regulatory authority relaxed Imports restrictions on COVID-19 vaccines. Also, it approved the restricted use of vaccines, which are already approved for restricted use by US in emergency situations.
- Consequently, newer generation mRNA vaccines and other vaccines effective against the variants and mutant strains are made available in India.
- However, full-fledged roll-out of these vaccines will be delayed. There is a mandatory requirement for trials and safety assessments of the first 100 recipients of these vaccines.
- Second, issue of ethics in making vaccines available for priority populations is a hurdle in universal vaccination. For instance,
- One, Priority was assigned to health care and other front-line health workers. Because it satisfied the doctrine of utilitarianism (Maximum benefit for maximum number of people).
- Two, Prioritising population above 60 plus and with co-morbidities was done to protect the most vulnerable.
- Three, prioritising population above 18 years was done based on health economics point of view. Because the Disability-Adjusted Life Years (DALYs) saved through vaccination of the 18-plus age-group would be the highest.
- However, students in the 16-plus age-group were deprived of vaccination.
- Third, the issue of vaccine pricing. Lack of access to vaccines for the population under 18 to 44-year age-bracket under the ‘Government of India channel’ may discourage the socially and economically disadvantaged people. For example, labourers and daily wage workers.
What needs to be done?
- One, utilising the data of vaccine efficacy of foreign vaccines that has been tested on Indian origin population can cut short the mandatory trial necessities in India.
- Two, allowing the population above 16 plus age group for getting vaccinated as approved by the United States Centers for Disease Control and Prevention.
- Third, State governments can provide the vaccine to Socially disadvantaged age-group free of cost. For example, Kerala have already committed to providing vaccines free of charge to all eligible people
- Fourth, the differential pricing regime announced by the Serum Institute of India and Bharat Biotech for supply of their vaccines to the central government and State governments needs to be reconsidered.
Source: The Hindu
What is “Breakthrough Infection”?
What is the News? The union health ministry has said that the breakthrough infection rate is low for both Covaxin and Covishield vaccines.
Contents
What is it?
- Breakthrough infection is a case of illness in which a vaccinated individual becomes sick from the same disease for which the vaccine was administered.
- Simply, it occurs when vaccines fail to provide immunity against the pathogen they are designed to target.
Possible Reasons for Breakthrough Infections:
- India’s healthcare and frontline workers were on the priority list for vaccination during the first phase. They were always prone to more occupational exposure to the coronavirus disease.
- The second wave of Covid-19 is highly transmissible, it might also have contributed to the breakthrough infection rates.
India’s Breakthrough Infections Data:
- Covishield: After the first dose two per 10,000 people get reinfected and after the second dose, three per 10,000 people get reinfected.
- Covaxin: After the first dose four per 10,000 people get reinfected after the number remains the same for the second dose too.
- This type of Infections are mostly mild or asymptomatic because the individuals still have partial protection.
Concerns:
- According to a US study, people with no symptoms transmit more than half of all cases. This means that controlling this silent transmission from persons without symptoms is very important for controlling the pandemic.
- Hence, it is very possible that an asymptomatic breakthrough infection can result in the further spread of the disease in the community.
- This happens especially because people may become careless following vaccination and many such infections are asymptomatic.
Source: The Hindu
Issues in Pricing Mechanism of Covid-19 vaccines
Synopsis: A single price for Covid-19 vaccines will fuel production and ensure efficient vaccination.
Introduction
Economists suggest market-based solutions for covid-19 vaccines due to their claimed efficiency. The market depends on the price mechanism and the forces of supply and demand.
- Increased competition pushes up supply and pushes down prices. This combination leads to an efficient allocation of scarce resources.
- However, the Market mechanism works well, when there is no externality is associated with the good.
- An externality occurs when the production or consumption of a good results in the cost or benefit to an unrelated third party.
- Vaccines have a positive externality because their use benefits the vaccinated person and also reduces transmission t0 others.
- Almost everyone ignores the full set of benefits from goods with positive/negative externalities. Thus, the market isn’t the most suitable tool for the distribution of such goods.
How the new Vaccine policy could result in vaccine failure?
The government is not considering the large positive externality attached to vaccination. This may result in inefficiency in vaccine delivery.
- Firstly, manufacturers have to declare their prices in advance for their 50 percent supply to the open market. However, there is no limit on the retail price they would charge. This might result in vaccine inequality.
- Secondly, low-income people are naturally prone to infect others because of their nature of work. Low income has a higher negative externality and thus vaccinating them first is more beneficial to society. However, these people cannot ordinarily afford the vaccine.
- Lastly, when the market is allowed to deliver vaccines, richer people will be prepared to pay more and will have better access.
- The market will ignore those with lower purchasing power, in spite of them having a higher chance of spreading the disease. The bigger the income difference between the two sections, the larger will be the degree of market failure.
What is the solution?
The new policy could lead to possible efficiency loss. The effective solution for addressing market failure is that a single price can be paid to vaccine makers for all the doses that they supply. The price should be high enough to fuel them to rapidly increase production.
- The government will have to pay the vaccine maker or the hospital managing the dose. The suggested solution is similar to the fertiliser subsidy, which is now paid to companies only after actual sales to farmers.
- A subsidy is not paid on any bag unless the purchase, along with the farmer’s biometric authentication and other details, is captured on a point-of-sale machine at the retail outlet linked to a central server.
- The vaccine producer gets the full market price after a person gets vaccinated. It will also ensure no deviation or grey market. It is in our own interest to get not just ourselves, but also others vaccinated.Source: click here
Measures to Control the Covid-19 Second Wave
Synopsis: The current rapid spread of the Covid-19 is a result of poor political choices, poor communications, and neglect of public health principles
Contents
Background
- India is witnessing a more intensive spread of Covid 19 in the second wave. For example, more than 3 lakh daily cases are reported, fatality rate has increased (2,000 deaths daily).
- This poses a threat to the economic and social well-being of the Indian people.
What are the reasons for the spurt in Covid 19 infection?
It is due to combination of many factors, such as
- Demography: India hosts the second largest population in the world. As the disease is contagious it spreads faster in high density population areas. Example, Cities like Delhi, Maharashtra.
- Diversity: India is geographically a large state and it is a socially diverse country. This makes controlling the coronavirus more challenging.
- Lack of effective Political leadership: During the first wave of infection, successful efforts to enforce social distancing and other public health measures helped in containing the spread of Covid19. However, the large political rallies and religious gatherings (Kumbh Mela festival) have contributed to the sudden surge in infection.
- Natural factors: Consistent mutation of the virus resulted in the production of more deadly variants. For example, India is now faced with “double mutant” strain of SARS-CoV-2.
- Ineffective public health management: Limited efforts towards genomic surveillance has resulted in lack of data to guide policy decisions.
What needs to be done?
First, need to break the chains of transmission by imposing Short-term targeted lockdowns. However, it has to be reminded that lockdowns cause a terrible economic and social cost and should be used as a last resort.
Second, need to expand access to vaccines. However, efforts must be made to overcome the logistical challenges to administer vaccines to a large number of populations.
Steps to minimise the number of lockdown days:
- Firstly, the Health functionaries should increase the testing rate with the goal of getting the positivity rate under 5%.
- Secondly, society has to be made responsible. Universal mask-wearing should be followed mandatorily as it is largely helpful in curbing the spread of the disease.
- Thirdly, sensitive decision-making by the political agents. Restriction on all major indoor and outdoor events, including rallies, religious festivals, weddings, is essential.
- Fourthly, vaccine manufacturers should be incentivized to produce Vaccines at a large capacity and at faster rate. In all likelihood, India’s pandemic will end if enough Indians are vaccinated.
Focus on public health measures, improve vaccinations, universal masking, and effective coordination across public health efforts can get back life to normal.
Source: The Hindu
“Harlequin Ichthyosis” – Odisha’s First Case
What is the News?
Odisha reported its first-ever case of a baby born with harlequin ichthyosis. It is a rare genetic condition.
Note: India’s first recorded case of a baby born with harlequin ichthyosis was in 2016, at a private hospital in Nagpur, Maharashtra. Such cases were also reported in Delhi, Patna, and West Bengal.
About Harlequin ichthyosis:
- Harlequin ichthyosis is a severe genetic disorder that mainly affects the skin.
- Cause: The disease is caused due to mutations in the ABCA 12 gene inherited from the parents.
- The ABCA12 protein plays a major role in transporting fats in cells that make up the outermost layer of skin.
- Severe mutations in the ABCA12 gene lead to the absence or partial production of the ABCA12 protein.
- This results in a lack of lipid transport. As a result, severity of the mutation affects skin development.
- Impact on Skin: The disease creates large diamond-shaped plates across the body that are separated by deep cracks (fissures). The skin becomes dry and scaly almost like fish skin and hence the term ‘icthyosis’, derived from ‘ikthus’, Greek for fish.
- Cases: The disease affects one in three million births.
- Treatment: There is no cure for harlequin ichthyosis yet. And, the current treatment is centred around protecting the skin and preventing infection.
Source: Down To Earth
UK Variant Behind current COVID-19 surge in Delhi: NCDC chief
What is the News?
The National Centre for Disease Control(NCDC) has released data obtained from the ‘Genome Sequencing of SARS-CoV-19’ Samples in India. UK Variant is the cause of the Current COVID-19 surge in Delhi.
Who conducted the study?
- Indian SARS-CoV-2 Consortium on Genomics(INSACOG) has conducted Genome Sequencing of around 15,000 samples. It is about 1% of India’s coronavirus caseload.
Key Findings from the study:
- Firstly, Variants of Concern(VoC): The relative proportion of known Variants of Concern or VoC (the U.K., South Africa, Brazil variants) is around 11% of the sequenced samples.
- VoC is a category used during the initial assessment of a newly emerged variant of a virus. Before this, an emerging variant may have been labeled a “variant of interest”.
- Secondly, The proportion of the UK. variant (B.1.1.7) in the samples sequenced from Delhi increased to 50% from 28% in the 2nd week of March.
- The UK variant has a mutation N501Y. It increases the transmission of the virus leading to increased disease severity and mortality.
- Thirdly, there was also a rise in the Indian variant (B.1.617). The Indian Variant possesses two mutations “E484K and L245R” that are associated with increased efficacy and decreasing the potency of vaccines.
- Fourthly, Vaccines Effectiveness: According to a Preliminary report by the CSIR-Centre for Cellular and Molecular Biology, Hyderabad, Covaxin and Covishield appeared to be effective against the Indian variant.
Source: The Hindu
Zydus Cadila’s antiviral drug “Virafin” gets emergency use nod
What is the News? Drug Controller General of India(DCGI) has granted emergency use approval for pharma major Zydus Cadila’s antiviral drug ‘Virafin’ to treat moderate COVID-19 in adults.
About Virafin Drug:
- Virafin is an antiviral drug. It is administered subcutaneously, i.e., it is injected under the skin. “Zydus Cadila”, a pharma major, manufactured. The drug was originally approved for the treatment of liver disease caused by the hepatitis B and C virus.
- The drug has now been repurposed for treating the moderate COVID-19 disease.
- It has been found that when the drug was given to Covid patients in the early stage, it showed significant improvement in moderate Covid cases.
- The drug was also found to reduce hours of supplemental oxygen required by patients.
- Moreover, patients who were treated with the drug ‘Virafin’ were tested Covid negative within 7 days.
- Hence, after the emergency approval, the drug will now be available on the prescription of a medical specialist for use in hospital/institutional setup.
Source: The Hindu
China Model to Contain Pandemic
Synopsis: The Centre should step in to coordinate policy measures across states to contain the pandemic, rather than putting the onus on the states. China’s model to contain pandemic should be studied and replicated in India
Contents
Background
- The central government recently adopted a decentralised decision-making approach, to contain the spread of Covid-19 second wave.
- The government has given free hand to the states to decide on lockdowns and other measures.
- Further, the Prime Minister in his recent speech appealed to the youth to form small committees to ensure adherence to COVID-19 restrictions.
- However, in the China model, centralised planning along with local mobilization shows a different story. It was immensely successful in containing the spread of COVID-19.
How the China Model functioned?
China Model included the Residential Committees (RC) at the grass-root level and the Central leadership to assist the RCs with resources.
About Residential Committees
- RCs were officially not part of the state and defined as institutions of self-governance. It had a large number of voluntary youths and college students.
- They had to perform administrative tasks, implement policy, mediate local disputes. Also, they had a task to assist government agencies with maintaining public surveillance, health, and sanitation, etc.,
- After the outbreak of the Pandemic, the RCs were the main authorities that enforced rules and assisted people with their necessities. For example,
- They strictly enforced rules of entry and exit. No residents were allowed to leave, and no non-residents were allowed to access the community area other than for essential medical needs.
- Also, they assisted people by providing home delivery of daily food necessities, tracing contacts, registering and visiting each individual, etc.,
Role of Central Leadership
- Further, the central leadership quickly acknowledged the efforts of the “first line of defence” the Residential Committees.
- The government also supported the RC workers with subsidies, provision of health equipment, insurance, publicity, and other institutional support.
The China Model though had certain challenges the epidemic has been successfully contained.
How the China Model can be replicated in India?
- In urban India, many have residential associations and local governments that can undertake similar mobilization like RCs in China.
- Through the support from Central leadership and a centralised plan of action, it can support them through resources and authority from central to local organisations.
- This will help in the effective mobilization of volunteers for better information dissemination, service delivery, and promoting social distancing.
Allowing states to their own means will only increase policy inconsistency and unequal access between states with different fiscal capacities and healthcare infrastructure. The need of the hour is for the central leadership to step up and coordinate policy measures across the country.
Source: Indian Express
India’s “New Covid-19 vaccine policy”
What is the News?The Government of India has announced the fourth phase of its New Covid-19 vaccine policy. This phase expands its vaccination coverage to everyone aged 18 and older from May 1.
Contents
Earlier Three Phases:
- The first three phases vaccinated healthcare workers, frontline workers, and those above the age of 45.
- The Centre procured the entire quantity of vaccines from manufacturers Serum Institute of India and Bharat Biotech(Covishield and Covaxin respectively). The centre then distributed them to states for vaccination.
- The states distributed the stock to government vaccination centres. These government centres administered the vaccine free of cost. Private hospitals charged recipients Rs 250 per dose.
Fourth Phase of Covid-19 Vaccine Policy:
Under this phase there are few changes,
Changes for Citizens:
- All adults over the age of 18 will be eligible for vaccination starting from May 1.
- Those eligible in the earlier phases can continue to get the free doses provided by the Government of India.
Changes in Distribution:
- Earlier, 100% of vaccines were being procured by the Centre and allocated to the states based on demand.
- Under the new rules, the Centre will automatically receive only 50% of vaccines produced by manufacturers. It will allocate these to states based on the extent of infection (active cases) and performance (speed of administration).
- The remaining 50% can be acquired by the states directly or by private hospitals and industrial establishments at a price.
Note: The government will monitor the prices charged by private hospitals. A mechanism will be put in place to monitor vaccine stocks and capturing prices on the Co-win platform.
READ ALSO :-Skill Development : news and updates
Imported Vaccines:
- The Centre will allow the imported, fully ready-to-use vaccines to be entirely utilised in the other-than-Government of India channel.
- Thus, if a foreign pharma giant brings its vaccine to India, it will be free to directly sell the entire stock in the open market at a competitive price.
Source: Indian Express
Roadblocks to achieve universal vaccination
Synopsis: India needs to develop a practical plan, as it is facing many roadblocks to achieve universal vaccination for all.
Background
- Initially, India decided to prioritize vaccination for the most vulnerable citizens (nearly 300 million).
- The main reason for that were the limitations of India’s manufacturing capacity to provide vaccination to its whole population.
- Thus, only about 5% of the intended beneficiaries have been vaccinated till now.
- However, a combination of panic, public pressure, and the magnitude of the second wave has forced the government to authorize vaccines to anyone above 18.
- Further, the state government’s control over procurement has been liberalized.
- But achieving the goal of universal vaccination for all is still a distant dream due to a lack of planning and preparedness.
Read Also- :-Appointment of Parliamentary Secretaries
What are the roadblocks to achieve universal vaccination for all?
- First, lack of foresight has led to shortages in the supply chain. India unlike other countries did not foresee a devastating second wave. Hence, India did not make purchase agreements with other vaccine manufacturers. India also applied different standards, while waiving critical trials for Covaxin, it applied stringent requirements for foreign companies.
- Second, liberalizing states to procure vaccines will not help. This is because of two reasons,
- One, already international vaccinators such as Pfizer and Moderna have supply commitments to other countries.
- Two, States in India are weak in finances and negotiating power.
- Third, with the resurfacing of lockdown due to second-wave, the administration of logistics will be challenging.
India could have avoided this situation with effective foresight and planning. Now, India should work with pragmatism and preparedness to achieve the goal of universal vaccination for all as soon as possible.
Source: The Hindu
Importance of Secondary Level Health Services
Synopsis: The load on tertiary health services can be reduced by strengthening the secondary level care health services. For rural areas, the focus should be on community health centres and for urban regions, peripheral hospitals at the secondary level.
Contents
Background:
- The Indian health system is generally divided into the primary, secondary and tertiary level.
- The second wave of Covid-19 has exposed the deficiencies in the current reactive approach of the government.
- People are dying due to a lack of access to treatment facilities rather than inadequate solutions to treat the virus.
Reactive approach:
- Under this, the government transforms well-performing facilities at the tertiary level into state-of-the-art COVID-19 hospitals.
- Similarly, many temporary COVID-19 facilities are created by hiring buildings and open spaces providing only beds.
- The government has also created many first-line treatment centres under this approach.
- This approach is being adopted in the majority of states.
Concerns associated with Reactive approach:
- People are unable to access their routine hospital services from these facilities. Because routine hospitals are turned into COVID facilities.
- The temporary structures without adequate infrastructure were unable to cater to the needs of patients in real-time situations.
- First-line treatment centres are failing to generate trust among people and were shut down when the cases went down.
Therefore, many experts are now advising the government to leverage the potential of the secondary level.
Read also- Ayushman Bharat
New Approach of using Secondary Level Health Services:
- Under this, the functional facilities at the secondary level can be converted into exclusive COVID-19 care centres. It will be useful to treat those patients who don’t need ICU support.
- In rural areas, the Community Health Centre (CHCs) can cumulatively add up to 50000-75000 beds.
- A CHC covers a population of 80,000-1,00,000 in rural areas.
- It functions as the first referral unit for curative care services referred from primary health centres (PHCs).
- The PHC (Primary Health Centres) must be strengthened to cater to the needs of people for other curative care services.
- In urban areas, states must develop peripheral hospitals at the secondary level within the government sector. Ideally, 100-150 bedded hospitals for every 3 lakh population.
Benefits of the Secondary Level Health Services:
- Firstly, it will reduce the workload on tertiary care especially in states like Bihar, Uttar Pradesh and Chhattisgarh, which possess poor health infrastructure.
- Secondly, Specialists for these secondary centres can be easily directed from district hospitals or medical colleges. Thereby providing better feasibility.
- Thirdly, these new centres can be used for sample collection and vaccine delivery as well. As the centres are already functional and command a certain level of trust.
- Fourthly, post-pandemic, these facilities can return to their normal work and won’t be closed like temporary structures.
Way Forward:
- The states must leverage the potential of this new secondary level approach.
- They should provide the secondary level units with sufficient funds and personnel so that they can duly function as COVID-19 care centres.
In a nutshell, we can say that adoption of this new approach will improve delivery potential, augment people’s trust and contribute to strengthening health services in the long run.
Source: The Hindu
“Global Diabetes Compact” – To Increase Access to Treatment
What is the News? The World Health Organization (WHO) launches a Global Diabetes Compact Initiative.
About Global Diabetes Compact Initiative:
- Global Diabetes Compact aims to reduce the risk of diabetes. It will ensure that all people diagnosed with diabetes have access to equitable, comprehensive, affordable, quality treatment and care.
- This initiative launched at the Global Diabetes Summit. WHO and the government of Canada Co-hosted the summit with the support of the University of Toronto.
- Global Targets: The initiative will set standards for tackling the disease in the form of ‘global coverage targets’. It will ensure a wider reach of diabetes care. A “global price tag” will also quantify the costs and benefits of meeting these new targets.
Need of Global Diabetes Compact
- Diabetes is one of the major comorbid conditions. It is linked to severe COVID-19 infections.
- The number of people with diabetes quadrupled in the last 40 years. It is also the only major non-communicable disease for which the risk of dying early is going up rather than down.
- About half of all adults with type 2 diabetes remain undiagnosed. And 50% of people with type 2 diabetes don’t get the insulin they need.
Also read – Increasing cases of getational Diabetes
About Diabetes:
- Diabetes is a Non-Communicable Disease (NCD) that occurs either when the pancreas does not produce enough insulin (a hormone that regulates blood sugar, or glucose) or when the body cannot effectively use the insulin it produces.
Read Also–Increasing Cases of Gestational Diabetes … –
Types of Diabetes:
- Type I diabetes: It is also known as juvenile diabetes (as it mostly affects children of age 14-16 years). It occurs when the body fails to produce sufficient insulin. People with type I diabetes are insulin-dependent which means they must take artificial insulin daily to stay alive.
- Type 2 diabetes: It affects the way the body uses insulin. While the body still makes insulin, unlike in type I, the cells in the body do not respond to it as effectively as they once did. This is also the most common type of diabetes, and it has strong links with obesity.
- Gestational diabetes: This type occurs in women during pregnancy when the body sometimes becomes less sensitive to insulin.
Source: Down To Earth
The Questions Surrounding COVID Vaccine Exports by India
Synopsis: The government should make sure to citizens that the COVID vaccine exports by India are not at the cost of their health.
Introduction:
Recently Minister of State in the Ministry of External Affairs stated that India is Exporting vaccines after considering the domestic and international Factors. Further, he also mentions that India will continue to export vaccines based on the production and needs of the national vaccination programme.
Contents
Potential of India’s vaccine exports:
- According to Ministry of External Affairs statistics, upto April 13, India alone supplied over 65 million vaccines to 90 countries globally. This accounts for one month of India’s current COVID-19 vaccines production. Of these
- More than 10 million doses are sent as grants.
- Almost 36 million on a commercial basis.
- About 19 million under the COVAX programme.
- India also exports vaccines to GAVI. India is a member of Gavi’s COVAX facility. Further, India also receives other vaccines from GAVI. So, exporting vaccine to GAVI is an obligation to India.
Why India need to export vaccine?
India explained the need to export vaccine during the recent Raisina Dialogue.
- Our PM mentioned that Humanity as a whole must be at the centre of our thinking and action. Further, he explains India must think of the entire humanity, not merely of people with Indian boundary.
- Also, the Minister of External Affairs mentions “equitable access to vaccines is critically important“. Further, he also mentions that “no one will be safe till everyone is safe”.
- Indian PM also mentioned the concept of ‘Vasudhaiva Kutumbakam’. (the world is one family). India desires to be a good global citizen. A similar concept is also there in the Objective Resolution. (moved by Jawaharlal Nehru in the Constituent Assembly by 1946.)
So being a responsible global power, India needs to think beyond itself. So, exporting vaccine is essential as much as vaccinating Indians.
How India calculates the number of Vaccines that it exports?
Being a global citizen India needs to export vaccines but not at the cost of non-vaccinating Indians. The recent Minister of State in the Ministry of External Affairs speech mentions that it is decided based on three factors.
- Quantum of domestic production.
- The demands of the national vaccine programme
- Requests for vaccines manufactured in India.
Questions surrounding quantum of exporting vaccine:
- Despite the above factors, the export value is not clearly defined. There is an ambiguity on how these factors collectively help in the decision-making process of calculating vaccine exports. For example, If an independent judgment is based on domestic production and national vaccine programme, then only the leftover(remaining) vaccine has to be exported.
- Even if it is obligatory to send vaccines to the COVAX program, sovereign states can always invoke national interest to override obligations.
- Similarly, the commercial contracts of the company can also get disregarded under existing laws to fulfill national interests.
So exporting vaccine is for the general foreign policy of India. But the government have to clarify to its people, that exports are not at the cost of their health.
Source: The Hindu
- According to Ministry of External Affairs statistics, upto April 13, India alone supplied over 65 million vaccines to 90 countries globally. This accounts for one month of India’s current COVID-19 vaccines production. Of these
Significance of Lessons from the First COVID Wave
Synopsis: Partial lockdowns again are going to widen economic and social inequalities. Every step towards prevention must consider the Lessons learnt from the first COVID-19 wave in India.
Introduction
- India’s second COVID-19 wave is more contagious than the first. Many States have imposed lockdowns of various scales. However, political rallies, social and religious events are still ongoing, making these restrictions meaningless.
How did the first wave lead to uneven growth?
The International Monetary Fund estimated India’s GDP to grow at 12.5% this year, but this growth cannot be inclusive.
- Firstly, the technological, pharmaceutical, and healthcare sectors saw the greatest growth. The wealth of billionaires in India increased by 35% even during the pandemic.
- Secondly, sectors including travel and tourism and wellness and hospitality recorded historic lows. The pandemic destroyed the informal and MSME sector. It pushed 75 million Indians into poverty.
- Thirdly, the unplanned lockdown highlighted the vulnerability of the migrant workers and poor as they had to walk back to their villages.
- Fourth, many economists predicted that India’s revival from the COVID-19 induced depression would be a ‘K-shaped’ curve. It means only a part of our population recovers.
- Fifthly, COVID-19 has affected the poor the most. Introducing partial lockdowns will limit the movement of goods and laborers. It will considerably reduce industrial productivity and create paths that will widen our inequalities.
Suggestions
Interconnected industries can function at the maximum possible capacity in multiple shifts. However, Strict health and safety regulations should be framed and followed. Non-essential gatherings should be banned.
- Firstly, governments will have to account for demand contraction. Thus, it should urgently ensure cash incentive packages at both individual and institutional levels. This will boost consumption and investments.
- Secondly, the need to provide additional provisions for job stamps; direct cash transfer and employment guarantee schemes.
- Thirdly, the NYAY scheme that guarantees a minimum income of ₹6,000 to every household is a solution that needs to be used at this time.
- Fourthly, reports indicate that new COVID-19 mutations are challenging even to the younger population. India will have to speed up vaccine production, procurement, and distribution.
- Fifthly, open vaccination for all age groups. This would make it easier for the majority of laborers to be present at their workplaces with lesser risks. Students will also be able to attend classes and examinations.
The conclusion
The government should take responsibility for the lapses in the health care system and vaccine shortages. The private sector and NGOs played a huge role in quickly scaling up healthcare infrastructure during the first wave. With political will and public participation, we should now be able to save lives without negotiating on our population’s livelihood.
Source: click here
“MANAS App” – A Mental-Health Digital platform
What is the News?
Principal Scientific Adviser to the Government of India has virtually launched the “MANAS” App.
About MANAS App:
- MANAS stands for Mental Health and Normalcy Augmentation System. It is a comprehensive, scalable, and a national digital wellbeing platform. It has been developed to promote the mental well-being of Indian citizens.
- Nodal Agency: Office of the Principal Scientific Adviser to the Government of India.
- Developed by: National Institute of Mental Health and Neuro Sciences (NIMHANS) Bengaluru, Armed Forces Medical College(AFMC), Pune, and Centre for Development of Advanced Computing(C-DAC) Bengaluru.
- Key Features:
- Firstly, the platform integrates the health and wellness efforts of various government ministries.
- Secondly, the application can be used for a person’s overall wellbeing and is supported by teleconsultation, especially for mental health-related problems.
- Thirdly, there will also be health tracking and all data records will be maintained. It will help users during future consultations.
- Significance: The platform was endorsed as a national program by the Prime Minister’s Science, Technology, and Innovation Advisory Council (PM-STIAC).
About Office of the Principal Scientific Adviser(PSA):
- Setup in: Office of the Principal Scientific Advisor (PSA) was set up in 1999 by the Cabinet Secretariat. It is currently a Secretary level position.
- Mandate: It is the chief advisor to the government on matters related to scientific policy. The policies focus on critical infrastructure, economic and social sectors.
About PM-STIAC:
- PM-STIAC is an overarching council. The Principal Scientific Advisor (PSA) is the chairman of the council.
- Functions: The council perform functions such as,
- Assess the status of specific S&T domains
- Comprehend challenges in S&T domains
- Formulates immediate, mid, and long term interventions and
- presents a roadmap to the Prime Minister.
Source: PIB
Importance of Clinical Trials in COVID-19 Treatment
Synopsis: Clinical Trials have been instrumental in the development of treatment for Covid-19 so far.
Introduction
The World Health Organization (WHO) declared the SARS-CoV-2 pandemic on March 11, 2020. Doctors did not know how to treat patients with COVID-19 in the beginning. Clinical care was dominated by opinion, narratives, and code of belief in the first few months.
- For example, it was believed that hydroxychloroquine could cure COVID-19. The truth is hydroxychloroquine does not benefit COVID-19 patients.
- After one year, many medicines which do not cure Covid-19 are still in use, such as steam inhalation, multivitamins, mineral supplements, ivermectin, and chloroquine, etc.
How the clinical trials helped in finding the best treatment?
Clinical trials are important for finding the best treatment. Doctors treated symptoms and provided life support until these trials produced results.
- Firstly, many COVID-19 patients developed blood clots and treated with blood-thinning medications. Other treatments included oxygen, breathing support ventilators for severely ill patients, kidney dialysis, and supporting heart with blood pressure medications.
- Secondly, COVID-19 demanded for producing high-quality evidence quickly. There was a requirement for designing trials to test many treatments at once with innovative designs such as platform trials and adaptive trials.
- For example, The RECOVERY trial network in the U.K., the REMAP-CAP trial globally focusing on critically ill patients, and the WHO-led SOLIDARITY trial.
- RECOVERY verified that there was no benefit of using hydroxychloroquine, azithromycin, lopinavir-ritonavir, colchicine, and convalescent plasma.
- REMAP-CAP found that hydroxychloroquine and lopinavir-ritonavir were harmful to use. It proved that there is no benefit with convalescent plasma.
- SOLIDARITY highlighted the lack of benefit of Remdesivir. It is an antiviral drug that possibly shortens the illness duration.
- Thirdly, it is important that the results of these clinical trials should be interpreted into clinical practice by healthcare professionals managing COVID-19 patients.
What are the drugs that have been proven to benefit COVID-19 patients?
- Firstly, Corticosteroid (dexamethasone) is effective in COVID-19 patients who require oxygen and in severely ill patients (hydrocortisone).
- Secondly, two interleukin-6 receptor blocking drugs (tocilizumab and sarilumab) benefit COVID-19 patients. They show enhanced results used in combination with corticosteroids, specifically in patients with moderate and severe COVID-19.
What should be done?
- Thus, clinical trials show that apart from supportive care (oxygen, ventilatory support), the only drugs that reduce mortality are steroids and interleukin-6 receptor blocking drugs. Thus, random drugs without proper clinical trial, need to be avoided
Source: click here
The National Commission for Allied and Healthcare Professions (NCAHP) Bill, 2020
Introduced: Rajya Sabha (15th Sep 2020)
Passed: Rajya Sabha (16th Mar 2021)
Passed: Lok Sabha (24th Mar 2021)
Present Status: Assent granted. Converted to an Act.
About National Commission for Allied and Healthcare Professions [NCAHP] Bill, 2020
Objective:
- The Bill seeks to regulate and standardize the education and practice of allied and healthcare professionals.
- Ministry: Health and Family Welfare
Allied health professionals and their role in the delivery of healthcare services-
Allied health professionals are individuals engaged in the delivery of health or related care. Their area of expertise includes therapeutic, diagnostic, curative, preventive, and rehabilitative interventions.
Role- They are the first to recognize the problems of the patients and serve as safety nets. Their awareness of patient care accountability adds tremendous value to the healthcare team in both the public and private sectors.
Key provisions of the NCAHP bill 2020
- Definition of Allied health professional: The Bill defines an allied health professional as an associate, technician, or technologist. The professional, who is trained to support the diagnosis and treatment of any illness, disease, injury, or impairment. For example- The bill recognizes over 50 professions such as physiotherapists, optometrists, nutritionists, medical laboratory professionals, radiotherapy technology professionals.
- Healthcare professional: A ‘healthcare professional’ includes a scientist, therapist, or any other professional who studies, advises, researches, supervises, or provides preventive, curative, rehabilitative, therapeutic, or promotional health services. Such a professional should have obtained a degree under this Bill. The duration of the degree should be at least 3,600 hours (over a period of three to six years).
- The bill uses the International System of Classification of Occupations (ISCO code) to classify allied professionals.
- This allows for greater global mobility and better prospects for such professionals.
- It will benefit up to 8-9 lakh current allied and healthcare professionals.
- The establishment of a central statutory body as a National Commission for Allied and Healthcare Professions. It shall perform the following functions:
- To frame policies and standards.
- To govern professional conduct.
- Also, to recommend credentials.
- Further, to establish and maintain a central registry.
- Professional Councils: The Commission will constitute a Professional Council for every recognised category of allied and healthcare professions. The Professional Council will consist of a president and four to 24 members, representing each profession in the recognised category. The Commission may delegate any of its functions to this Council.
- The Bill has the provision for state allied and healthcare councils to execute major functions through autonomous boards.
- The state councils are in charge of implementation, while the National Commission is in charge of policy formulation.
- Offences and penalties: No person is allowed to practice as a qualified allied and healthcare practitioner other than those enrolled in a State Register or the National Register. Any person who contravenes this provision will be punished with a fine of Rs 50,000.
Why government’s recognition of allied healthcare professionals is a paradigm shift?
- Stressful life due to modern lifestyle, rapid urbanization
- Rising chronic non-communicable disease burden.
- An increasing proportion of elderly people.
The above issues require a change in healthcare delivery methods. Therefore, trained, allied health professionals are needed to care for patients with mental illnesses, the elderly, those in need of palliative treatment. Also, it will enable professional services for lifestyle change related to physical activity and diets.
Way forward-
- Allied healthcare professionals are an important part of the medical profession. Their contribution is equal to, if not greater than, that of doctors.
- The law would increase job opportunities for allied and healthcare professionals and also provide dignity to their valuable works.
Source- The Indian Express
India’s vaccination strategy needs a course correction
Synopsis: India’s vaccination strategy lacks a few important steps and needs immediate action.
Introduction: Recently the Drug Controller General of India formally approved another vaccine candidate(Sputnik V). This vaccine is approved under emergency use authorisation.
India’s vaccination strategy:
- So far, India’s vaccination strategy relied almost entirely on Covishield. The other vaccine Covaxin so far has only limited extent in India’s vaccine strategy.
- India also allowed using foreign-made vaccines in India. But, these vaccines have to be approved by their respective regulatory agencies. Such as the U.S., the U.K., Europe, Japan.
- Similarly, there is World Health Organization’s (WHO) list of approved emergency use vaccines. Indians can also use those vaccines.
Concerns with India’s vaccination strategy:
- Vaccine approved in a different country may have adverse effects on the Indian population.
- The WHO vaccines can avoid local clinical trials. But, they are subject to parallel bridging trials. For example, Pfizer approached Indian regulators for such bridging trails.
- India due to emergency use authorization rushed through its regulatory process. This is evident as India had enough time and opportunity to conduct clinical trials in the right way for Vaccines such as Covishield and Covaxin. But India approved these vaccines under Emergency use.
- Not clear planning on vaccine stocks. Countries like the U.K. and the U.S. planned enough vaccine dosage for their country in attaining self-sufficiency. For example, in the US at least 30% of its adults have got one dose of vaccination. But India did not have any such plan. So, without that, ‘atmanirbhar’ in the vaccine is not feasible.
Suggestions to improve India’s Vaccine strategy:
India’s pharmacovigilance programme has to step up to solve the challenges in India’s vaccine strategy.
- India must not repeat the same mistake. India has to understand that the available choice of vaccine does not translate into immediate availability.
- All the Indian vaccine companies had a tie-up with their foreign counterparts. So, even though they make millions of vaccines in India, they will sell them to the highest global bidders(Profit-motive). So India has to ensure vaccine availability to at least for its adult population.
- India has to study the past. Last year, the Indian health system faced a shortage of hospital beds, ventilators, and black marketing of drugs. With the cases increasing once again, India has to improve the situation prior to the worrying state.
Source: The Hindu
WHO guidelines to control Transmission of “Zoonotic Diseases”
What is the News?
The World Health Organization(WHO), World Organization for Animal Health and United Nations Environment Programme jointly released guidelines to control “Zoonotic Diseases” for governments. Guidelines ask to reduce the risk of transmission of zoonotic pathogens to humans in food production and marketing chains.
What are Zoonotic Diseases?
- Zoonosis is an infectious disease that jumps from a non-human animal to humans.
- Zoonotic pathogens may be bacterial, viral, or parasitic. They can spread to humans through direct contact or through food, water, and the environment.
Key Guidelines issued by WHO:
- Firstly, Countries should suspend the sale of live animals captured from the wild in food markets. This is an emergency measure as they are the leading source of emerging infectious diseases like the coronavirus.
- Secondly, strengthening the regulatory base for improving standards of hygiene and sanitation in traditional food markets. This will reduce the risk of transmission of zoonotic diseases.
- Thirdly, Adequately training food inspectors to ensure businesses comply with regulations to protect consumers’ health.
- Fourthly, Strengthening animal health surveillance systems for zoonotic pathogens. This includes both domestic and wild animals. This will provide an early warning for pathogen emergence. Further, it will also help in developing the control measures.
- Fifthly, Developing and implementing food safety information campaigns. The campaign should create awareness to market traders, stallholders, consumers, and the wide public. These campaigns should communicate the principles of food safety and the risks of transmission of zoonotic pathogens.
Source: The Hindu
ICMR’s International Symposium on “One Health” in India
What is the News? Union Minister for Health and Family Welfare chairs ICMR’s International Symposium for one health in India.Contents
About ICMR’s International Symposium
- ICMR’s Indian Journal of Medical Research: The journal discusses the One Health approach.
- The title of this symposium is ‘One Health in India: Research informing biosafety, preparedness, and response’.
- Committee on Eco-Health Initiatives: A high-level steering committee for Eco-Health Initiatives in India was announced. This committee will have its secretariat hosted at the ICMR. It will be supported by the upcoming National Institute of One Health which is planned to be set up in Nagpur.
About One Health:
- It is an approach that recognizes that the health of humans, animals, and ecosystems are interconnected.
- Hence, it involves applying a coordinated and multidisciplinary approach at the local, regional, national and global levels. It will address potential or existing risks that originate at the animal-human ecosystems interface.
Importance of Approach:
- The approach is important because many times the same microbes infect animals and humans as they share the ecosystems they live in. Hence, efforts by just one sector cannot prevent or eliminate the infection.
- Examples:
- Rabies in humans can be effectively prevented only by targeting the animal source of the virus (for example, by vaccinating dogs).
- Information on influenza viruses circulating in animals is crucial to the selection of viruses for human vaccines for potential influenza pandemics.
Application areas of One Health
This approach is particularly relevant for:
- Food safety
- Control of zoonoses (diseases that can spread between animals and humans, such as flu, rabies, and Rift Valley Fever)
- Combating antibiotic resistance (when bacteria change after exposure to antibiotics and become more difficult to treat).
Examples of Approach:
- It helped discover the source of Kyasanur Forest Disease (KFD), a highly dangerous hemorrhagic fever more threatening than COVID-19.
Source: PIB
ICMR’s 3rd serological survey: Need to rethink on vaccination strategy
National Policy for Rare Diseases 2021
Synopsis – National Policy for Rare Diseases 2021 is a good start; it provides financial assistance for one-time treatments of up to Rs. 20 lakh, implements a crowdfunding mechanism, establishes a rare disease registry, and allows for early detection.
Introduction-
- Recently, the Ministry of Health and Family Welfare has approved the National Rare Disease Policy 2021.
- The policy provides financial assistance for one-time treatments of up to Rs. 20 lakh, implements a crowd-funding mechanism, establishes a rare disease registry, and allows for early detection.
What is a Rare Disease?
Any disease that affects a small percentage of the population is considered rare. World Health Organization defines rare disease as having a frequency of less than 6.5-10 per 10,000 people.
- Around 7000 rare disease have been identifies. In which 80 percent are of genetic origin.
- India has around 70 million people affected by rare diseases.
- Example of rare disease– Inherited cancers, Autoimmune disorders, Congenital malformations, Hirschsprung’s disease, Gaucher disease, Cystic fibrosis, Muscular dystrophies and Lysosomal Storage Disorders (LSDs).
What are the key highlights of the policy?
- First, Categorization – The policy has categorised rare diseases in three groups:
- Group 1- Disorders amenable to one-time curative treatment.
- Group 2- Those requiring long term or lifelong treatment.
- Group 3- Diseases for which definitive treatment is available but challenges are to make optimal patient selection for benefit, very high cost and lifelong therapy.
- Second, Financial support– Those suffering from rare diseases (diseases specified in Group 1 of the rare disease policy) would be eligible for financial assistance of up to Rs20 lakh under the Rashtriya Arogya Nidhi umbrella scheme.
- Voluntary crowd-funding for treatment- The policy will make use of a crowd-funding mechanism to cover the cost of treatment of rare diseases.
Concern with the Policy-
- Group 3 patients are completely ignored – Group 3 patients are now at risk and at the mercy of crowd-funding due to a lack of long-term funding support.
Way forward-
State needs to adopt a load sharing model– The Centre’s contribution of the annual costs will be halved [Rs. 40- 50 crore], if it can persuade the States to adopt a load-sharing model, as a few states such as Kerala, Tamil Nadu, and Karnataka have already suggested
Source- The Hindu
Health Ministry Releases “National Policy for Rare Diseases 2021”
What is the News?
The caretakers of patients with ‘rare diseases’ are not satisfied with the National Policy for Rare Diseases 2021. The Union Health Ministry recently released the policy.
Rare Diseases: WHO defines a rare disease as a lifelong disease or disorder that often highly weakens an individual. It has a prevalence of 1 or less per 1000 population. Example: Haemophilia, Thalassemia, Sickle cell anaemia, auto-immune diseases among others.
- However, every country has its own definition for rare diseases.
- The US defines rare diseases as a disease or condition that affects fewer than 200,000 patients in the country.
- Likewise, the EU defines rare diseases as life-threatening or chronically debilitating (weakening) condition. It should affect no more than 5 in 10,000 people.
About National Policy For Rare Diseases,2021:
- Aim: The policy aims to lower the incidence and prevalence of rare diseases based on an integrated and comprehensive preventive strategy. The strategy includes awareness generation, counselling programmes, providing affordable Health Care among others.
Key Features of the National Policy For Rare Diseases,2021:
- Categorisation: The policy categorizes rare diseases into three groups:
- Group 1: Disorders amenable to one-time curative treatment;
- Group 2: Diseases requiring long term or lifelong treatment; and
- Group 3: Diseases for which definitive treatment is available, but challenges are to make an optimal patient selection for benefit.
- Government Support:
- The government will provide Financial support of up to Rs. 20 lakh under the Umbrella Scheme of Rashtriya Arogya Nidhi for treatment of those rare diseases listed under Group 1.
- Moreover, Beneficiaries for such financial assistance would not be limited to BPL families. About 40% of the population, eligible under Pradhan Mantri Jan Arogya Yojana, will also be eligible for assistance.
- Further, for group 2, the State Governments can consider supporting specific patients. It includes a rare disease that can be managed with special diets or hormonal supplements or other relatively low-cost interventions (Diseases listed under Group 2).
- Voluntary Crowdfunding: The government has said that it will assist in voluntary crowd-funding for the treatment of Group 3. It is because it will be difficult to fully finance the treatment of high-cost rare diseases of Group 3.
Objections to the Policy:
- The policy offers no support to patients awaiting treatment since the earlier National Policy for Treatment of Rare Diseases 2017 was kept on hold.
- The policy has left patients with Group 3 rare diseases to fend for themselves. It has absolutely no consideration for Group 3 patients who require lifelong treatment support.
Rashtriya Arogya Nidhi scheme:
It provides financial assistance to patients living below the poverty line and who are suffering from major life-threatening diseases, to receive medical treatment.
Source: The Hindu
Ministry of Health and Family Welfare launches “Tribal TB Initiative”
What is the News?
Union Health Minister launches the Tribal TB Initiative to achieve the goal of TB Mukt Bharat.
About Tribal TB Initiative:
- Aim: Firstly, Tribal TB Initiative aims to address the problem of Tuberculosis in Tribal Population.
- Secondly, the initiative will initially focus on 161 districts across 18 identified States. It will focus on vulnerability mapping, active case finding, and promote behavioral change at the ground level.
- Thirdly, TB Mukt Bharat initiative aims at the elimination of TB by 2025.
Why was this initiative launched?
- Over 104 million tribal populations live in India. It spreads across 705 tribes and accounts for 8.6 % of India’s population.
- This tribal population is highly vulnerable to TB due to physical remoteness, malnutrition, poor living conditions, and lack of awareness. Hence, the initiative is launched to focus on these areas.
Note:
- Lakshadweep and the district of Badgam in Jammu and Kashmir have been declared TB Free on World TB Day 2021.
- The Government of India has increased the Budget allocation for TB in India four-fold in the last 5 years.
Other Tribal Health-Related Initiatives:
- ALEKH: It is an e-newsletter that is to be released on a quarterly basis. It will showcase the works of different stakeholders involved in improving the health and nutrition of tribals.
- Swasthya Portal: It aims to provide health and nutrition-related information to the tribal population of India.
Source: AIR
Health Minister Appointed as Chairman of “Stop TB Partnership Board”
“Double Mutant” COVID Virus Variant Found
Contents
What is the News?
Indian SARS-CoV-2 Consortium on Genomics (INSACOG) has been doing genome sequencing of Covid-19 Variants. It has found a unique “double mutant” virus variant in India. This variant has a unique combination of mutations, not seen anywhere else in the world.
What is Double Mutation?
- Double Mutation is when two mutated strains of a virus come together and form a third strain.
- The one reported in India is the result of the combination of E484Q, and L452R strains. The L452R strain is found in California in the United States, while, the E484Q strain is indigenous.
Is this double Mutant COVID Variant Harmful?
- Mutation in the virus is a normal process. But some mutations help the virus in defending itself from vaccines or antibodies or linking to a spike in cases.
- However, the capability of double mutant coronavirus variant in increased infectivity or in making COVID-19 more severe is still uncertain.
- Hence, INSACOG will submit details of this variant to a global repository called GISAID. If it qualifies, it will be classified as a “variant of concern”(VOC).
- Variant of concerns requires appropriate public health actions, such as
- Notification to WHO under the International Health Regulations,
- reporting to CDC,
- local or regional efforts to control spread,
- increased testing, or research to determine the effectiveness of vaccines and treatments against the variant
Note: So far, only three global Variants of Concern (VOCs) have been identified: the U.K. variant (B.1.1.7), the South African (B.1.351) and the Brazilian (P.1) lineage.
About INSACOG:
- Indian SARS-CoV-2 Consortium on Genomics(INSACOG) is a grouping of 10 National Laboratories. It was established by the Ministry of Health and Family Welfare(MoH&FW).
- Aim:
- Firstly, to monitor the genomic variations in the SARS-CoV-2 on a regular basis through a multi-laboratory network.
- Secondly, to ascertain the status of a new variant of SARS-CoV-2 in the country.
- Furthermore, to establish a surveillance system for early detection of genomic variants and determine the genomic variants in the unusual events/trends.
- Coordinated by: The Department of Biotechnology (DBT) along with MoH&FW, ICMR, and CSIR coordinate it.
- Significance: The knowledge generated through this vital research consortium assists in developing diagnostics and potential therapeutics and vaccines in the future.
Global Initiative on Sharing All Influenza Data(GISAID) Initiative
- The GISAID Initiative was launched on the occasion of the 61st World Health Assembly in 2008.
- In 2010, Germany became the official host of the GISAID Initiative through a public-private partnership.
- Aim: It aims to promote rapid sharing of data of all influenza and COVID virus sequences globally. Moreover, it helps to understand, how the viruses evolve, spread, and potentially become pandemics.
- Headquarters: Munich, Germany.
Source: The Hindu
What is “Parosmia”?
What is the News?
The most common symptoms of Covid-19 are anosmia and ageusia. However, several people are also experiencing parosmia. It is characterized by a change in perception of odours.
Anosmia: It is the partial or complete loss of the sense of smell. This loss may be temporary or permanent.
Ageusia: It is a condition, characterized by a complete loss of taste function of the tongue.
About Parosmia:
- Firstly, Parosmia is a medical term. It describes a condition in which affected individuals experience distortions in the sense of smell.
- Secondly, a person with parosmia is able to detect certain odours. But they might experience the smell of certain things as different and often unpleasant. For example, coffee may smell like burnt toast.
- Thirdly, Causes: People who are recovering their sense of smell following a loss from a virus or an injury typically experience parosmia.
- And lastly, Parosmia is a temporary condition and is not harmful in itself.
Source: Indian Express
Deadly drug-resistant superbug “Candida Auris or C.Auris” found in Andamans
Contents
What is the News?
Candida Auris (deadly hospital pathogen) identified for the first time in the Andaman and Nicobar Islands.
About Candida Auris:
- Candida Auris or C.auris is a multidrug-resistant fungus. It presents a serious global threat to human health.
Origin of Candida Auris:
- Candida Auris was first identified in 2009 in a patient in Japan. The fungus emerged in more than 40 countries across five continents in the last decade.
- The fungus is mostly found in tropical marshes and marine environments, outside hospital environments.
- However, it is an emerging pathogen, thus very little is known about the Candida Auris so far.
Symptoms of C.Auris:
- C.Auris infections can show no symptoms before turning into a fever and chills. These symptoms don’t go away despite the use of medicines and can lead to death.
- C.auris survives on the skin before entering the body through wounds. Once in the bloodstream, it causes severe illness and can lead to death.
Why C.Auris is harmful? C.Auris is considered dangerous because of three reasons:
- Fisrtly, C.Auris is often multidrug-resistant. It means that it is resistant to multiple antifungal drugs commonly used to treat Candida infections.
- Secondly, it can survive and persist within the hospital environment for prolonged periods. It is capable to survive on dry environmental surfaces for prolonged periods. It means that it adapts well to survival outside human host settings as well.
- Lastly, C.Auris is difficult to identify with standard laboratory methods, and it can be misidentified in labs without specific technology. Misidentification may lead to inappropriate management.
Vulnerable Population:
- C.Auris can get deadly for immunocompromised patients. The incidence of deaths from this fungal infection is high in countries such as the US and the UK, but its prevalence is less in Indian hospitals.
Treatment:
- Echinocandins, a class of antifungal drugs, can treat most of the C.auris infections. However, some C. auris infections have been resistant to antifungal medications making them more difficult to treat.
Source: Indian Express
Public trust is key to successful vaccination programmes
Synopsis- Need transparency and timely data sharing to build public trust in the COVID-19 vaccination programme.
Introduction-
- Major European countries, including Germany, France, Italy, and Spain have halted the use of AstraZeneca’s COVID-19 vaccine. This is followed by the warnings of harmful blood clots in some recipients.
- However, the World Health Organization (WHO) and the European Medicines Agency have ruled out any correlation between AstraZeneca’s vaccine and blood clots.
Data on Blood Clot:
According to a study based on the U.S. population, about 1,000 to 2,000 blood clots occurs every single day in the human body.
In the recent AstraZeneca’s COVID-19 vaccine case, there are only 40 blood clot cases reported due to that.
But people are reluctant to get the vaccine due to these types of events. Further, it would lead to a negative effect on the vaccination push.
What are the reasons behind the impediments to vaccination programmes?
- No proper vaccine efficacy data available – There is uncertainty and suspicion regarding the side effects of the Covid-19 vaccine.
- The risks associated with COVID-19 vaccines have not been fully investigated as these vaccines were issued under the Emergency Use Authorizations.
- The National Committee on Adverse Events Following Immunization has no proper details about the serious adverse events following immunization.
- Transparency and prompt data sharing: There is lack of transparency and data sharing in vaccination programmes. It could lead to a lack of trust in the vaccine.
Suggestions to improve vaccination programmes
- Firstly, transparency and timely data sharing about the vaccine, and open public health communication will win public trust and faith in vaccines.
- Secondly, like the U.S. Centers for Disease Control and Prevention, India should also create data on adverse vaccine effects.
- Lastly, vaccine hesitancy is the main obstruction in the smooth vaccination drive. And so, it must resolve immediately.
Source- The Hindu
Health Minister Appointed as Chairman of “Stop TB Partnership Board”
What is the News?
Union Minister for Health and Family Welfare appointed as the Chairman of the Stop TB Partnership Board. The Minister will serve a 3-year term commencing July 2021.
About Stop TB Partnership:
- Stop TB Partnership was established in the Year 2000.
- Aim: The aim is to eliminate tuberculosis as a public health problem.
- Significance: It is a unique international body as it aligns all countries in the world to fight against TB.
- Amsterdam Declaration: In 2000, Stop TB Partnership gave a call for collaborative action from ministerial delegations of 20 countries with the highest burden of TB.
- Partner organizations: It has 1500 partner organizations. It includes international, non-governmental, and governmental organizations and patient groups.
- Secretariat: Geneva, Switzerland.
India’s Initiatives against Tuberculosis:
- Firstly, India has committed to eliminating TB in the country by 2025, five years ahead of the global deadline of 2030.
- Secondly, National Strategic Plan (NSP) for TB Elimination (2017-2025): It is a framework to provide guidance for the activities of various stakeholders to reduce the burden of TB mortality and morbidity. It aims to work towards the elimination of TB in India by 2025.
- Thirdly, Nikshay Poshan Yojana: It is a direct benefit transfer (DBT) scheme to provide nutritional support to TB patients.
- Lastly, TB Harega Desh Jeetega’ Campaign: This campaign aims to improve and expand the reach of Tuberculosis care services across the country by 2022.
Source: PIB
WHO Announced “Global Breast Cancer Initiative”
What is the News?
The World Health Organization (WHO) announced an initiative called the “Global Breast Cancer Initiative”.
About Global Breast Cancer Initiative:
- Aim: The initiative aims to reduce global breast mortality by 2.5% by 2040.
- The initiative will particularly focus on reducing deaths in low-income countries. There the progress to tackle the disease is relatively slow.
- Key Features of the Initiative:
- Guidance to Governments: Under the initiative, WHO will work with other UN agencies. They will provide guidance to governments on how to strengthen systems for diagnosing and treating breast cancer. It is expected to improve capacities to manage other types of cancer.
- Evidence-based Technical Package: An evidence-based technical package will also be provided to countries as part of the initiative. It will incorporate existing WHO cancer tools and products.
About Breast Cancer:
- Breast cancer is the most common form of cancer in women. It is responsible for one in six cancer deaths among women and has overtaken lung cancer as the world’s most commonly diagnosed cancer.
- Survival Rates: Breast cancer survives for five years after diagnosis exceeds 80% in most high-income countries. However, it is 66% in India and 40% in South Africa.
Source: Down To Earth
Increasing Cases of Gestational Diabetes in India
Synopsis: India registers a high number of gestational diabetes cases, which are bound to increase in the future. This coupled with low awareness and poor testing potential calls for immediate action.Contents
Background:
- Diabetes is a metabolic disease that causes high blood sugar. The hormone insulin moves sugar from the blood into your cells to be stored or used for energy.
- If a person is having diabetes, the body either doesn’t make enough insulin or can’t effectively use the insulin it makes.
- India has 7 crore cases of diabetes and almost 3.5 crore prediabetes cases.
- Further, Type 2 diabetes is most common, it is preventable with some lifestyle changes. However, very less focus is placed on Gestational diabetes.
About Gestational Diabetes:
- It is a transitory form of diabetes occurring in pregnant women.
- South Asian women are at higher risk of development as shown by data from the International Diabetes Federation. It estimates that 25% of south Asian women would develop it.
- In India, it is assumed to be more prevalent in urban areas (30%) than rural areas (10%). Further, assuming a 10% rate of development, the figure for gestational diabetes comes around 27-30 lakh women every year.
Impact of Gestational Diabetes:
- First, it enhances complications during pregnancy. This includes preeclampsia (fits during pregnancy), prolonged and obstructed labor, need for assisted delivery, postpartum hemorrhage, etc.
- Second, the above complications can cause a spike in maternal and neonatal mortality rates.
- Third, if not death, then the probability of developing other problems is quite high.
- Type 2 diabetes gets developed in almost 50% of women.
- Children also are at high risk of obesity, type 2 diabetes, and cardiovascular diseases.
Challenges in Managing Gestational Diabetes:
- First, there is a lack of awareness regarding gestational diabetes due to which, it gets noticed after the complication has occurred.
- Second, our health system also lacks the capacity for providing robust and timely testing.
Way Forward:
- There should be a prompt and adequate implementation of national guidelines on the diagnosis and management of gestational diabetes.
- The single test procedure suggested by Dr. V. Seshiah (a pioneer in the field of diabetes and pregnancy) and subsequently approved by the World Health Organisation should be adopted for better diagnosis.
- In order to spread awareness, the 10th march can be celebrated as National Gestational Diabetes Awareness Day.
- The Diabetes Study Group of India recommended this step as it would be an act to recognize Dr V. Seshiah’s contribution to the field of diabetes and pregnancy for more than 40 years.
Source: The Hindu
Cabinet approves “Pradhan Mantri Swasthya Suraksha Nidhi | PMSSN”
What is the News?
The Union Cabinet approves the Pradhan Mantri Swasthya Suraksha Nidhi (PMSSN).
About Pradhan Mantri Swasthya Suraksha Nidhi(PMSSN):
This program will ensure access to universal & affordable health care through a fund that does not lapse at the end of the financial year.
Features:
- It has been set up as a single non-lapsable reserve fund for a share of Health.
- It will be made from the share of health in the proceeds of Health and Education Cess.
- The fund will be administered and maintained by the Ministry of Health & Family Welfare
Note: Finance Minister announced the 4% Health and Education Cess during the Budget 2018-19. It replaced the existing 3% Education Cess.
How will the fund be utilised? The fund will be utilized for the following flagship schemes of the Ministry of Health & Family Welfare:
- Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana (AB-PMJAY)
- Ayushman Bharat – Health and Wellness Centres (AB-HWCs)
- National Health Mission
- Pradhan Mantri Swasthya Suraksha Yojana (PMSSY)
- Emergency & disaster preparedness and responses during health emergencies
- Any future programme/scheme that targets to achieve progress towards SDGs and the targets set out in the National Health Policy (NHP) 2017.
Source: PIB
Prerequisites for Developing Digital Health Data
Synopsis: National Digital Health Mission aims to build digital health infrastructure in India. But there are many hurdles in developing comprehensive digital health data.Introduction:
Recently on Independence Day, our Prime Minister announced National Digital Health Mission. The Mission aims to develop the backbone for integrated digital health infrastructure in India. Developing countries with significant health challenges like India critically need such an infrastructure.
The NDHM will help in developing the diagnostics and management of health services. Apart from that, the NDHM will also help in achieving broader public health monitoring, research, socio-economic studies, prioritizing resource allocation and policy interventions, etc.
Digitization can make healthcare more organized, effective, and efficient. But we must know that Digitization can’t substitute the fundamentals like an investment in nutrition and welfare, primary healthcare services and healthcare professionals, etc.
What is the prerequisite to digital health infrastructure?
Before going completely digital, certain things are essential to achieve the desired social objectives. They are,
- India needs to carefully develop various ways to fulfil the “health needs of the public”. India needs to carefully examine the following things and their improvement with digitization. Such as,
- Ways of facilitating better diagnosis and management,
- Understanding of the data structures for effective health services
- Alleviate health problems with digitization such as malnutrition and child stunting, etc.
- Challenges with Privacy: It may also create tensions between a collection of digital health data and individual rights to privacy. For example, many countries like UK, Sweden, the US, etc. attempted to build digital health infrastructures they were not successful due to serious privacy-related controversies.
- Linking the digital health data to other sectors: This data may be linked to other sectors such as banking and services with adequate access to data. This creates two types of challenges.
- Not linking the digital health data with other sectors will make the potential uses of digital health data very limited.
- Complete interlinking of digital health data will create various problems such as privacy violation, the vulnerability of data to profit-motivated pharma companies, etc.
- Design of Digital health data operations: Access to digital data requires identifying and understanding the complexity in various data sources such as immunisation records, data in government and private hospitals, diagnostic centres, etc. The design should also include an understanding of data generation frequency, error models, sharing and other operational requirements, etc.
- Building an effective system that can generate people’s trust requires building a transparent process. That process should have openness and public consultations in all spheres of development. This includes avoiding “crony expertise”, rejecting poorly-conceived designs and ideas, etc.
So, developing a comprehensive digital health infrastructure not only depends on the health sector alone. Instead, it also depends on e-governance and the administration of digitisation in India.
- India needs to carefully develop various ways to fulfil the “health needs of the public”. India needs to carefully examine the following things and their improvement with digitization. Such as,
Issues associated with the launch of Coronil
Synopsis: Coronil Launch event is in controversy again. Ministers and public figures must not be seen as endorsing drugs whose efficacy is in doubt
Background
At a recent event, Haridwar-based Patanjali announced that its Coronil Ayurveda medicine recognized as a “supporting measure in COVID-19” by Ayush Ministry. Ministry awarded the Certificate of Pharmaceutical Product (CoPP) as per the WHO certification scheme.
After receiving certification, the export of medicine has become possible. This event was presided by Union Health Minister Harsh Vardhan and Transport Minister Nitin Gadkari.
The company claimed that it is the first evidence-based medicine to fight COVID-19.
This event attracted several criticisms. Indian Medical Association (IMA) criticized this promotion as unethical and a “blatant deceiving of the people of the country”.
What are the issues associated with the launch of Coronil?
- Firstly, Patanjali is a private company and coronil is the product of it. As per code of act, Doctors are barred from promoting any drugs and Dr Harsh Vardhan (health minister) is an ENT surgeon.
- Secondly, Baba Ramdev claimed at the event that WHO endorsed Coronil. Whereas, WHO South-East Asia in a tweet refused any such endorsement.
- Third, the publication of a randomized clinical trial of Coronil in a research journal was also put forward as an endorsement by that magazine. These publications are nothing but an initial requirement that put forward the report in front of subject experts.
- Fourth, the published report reveals that medicine was tested only on 95 patients. All of them were asymptomatic and mildly symptomatic but confirmed as RT-PCR positive. This number is very small. Moreover, a large population with mild or no symptoms recovers without any external intervention.
However, it is not the only case, where a drug approved without any solid research. DGCA previously approved itolizumab by Biocon, which was tested only on the sample of 30. Approval of Covaxin also was in a haste and lacked solid scientific evidences.
Integration of “Non-Alcoholic Fatty Liver Disease” with NPCDCS
What is the news?
The Ministry of Health & Family Welfare has launched operational guidelines for integration of NAFLD(Non-Alcoholic Fatty Liver Disease) under NPCDCS (National Programme for Prevention & Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke).
About NPCDCS (National Programme for Prevention & Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke):
- Launched in: It was launched in 2010. It aims to prevent and control Non-Communicable Diseases(NCDs).
- Implemented under: National Health Mission(NHM).
- Objectives: The objectives of the programme include awareness generation for the prevention of NCDs. Some important constituents of this program are screening, early detection, management and referral to an appropriate level health facility.
About Non-Alcoholic Fatty Liver Disease(NAFLD):
- It is a term for abnormal accumulation of fat in the liver despite the absence of harmful alcohol use, viral hepatitis or medications.
- Prevalence of NAFLD in India: As per studies, the prevalence of NAFLD is around 9% to 32% of the general population in India. There is a higher prevalence among overweight or obesity and those with diabetes or prediabetes.
Stages of NAFLD: The main stages of NAFLD are:
- Simple Fatty Liver Disease – It is a largely harmless build-up of fat in the liver cells. It may only be diagnosed during tests carried out for another reason.
- Non-Alcoholic steatohepatitis(NASH) – Mere deposition of fat in the liver is termed steatosis. It is characterized by inflammation of the liver.
- Fibrosis – It is where persistent inflammation causes scar tissue around the liver and nearby blood vessels. But the liver still able to function normally.
- Cirrhosis – It is the most severe stage after years of inflammation. At this stage, the liver shrinks and becomes scarred and lumpy. This damage is permanent and can lead to liver failure (where your liver stops working properly) and liver cancer.
Is NAFLD Curable?
- Once the disease develops, there is no specific cure available, and health promotion and prevention aspects targeting weight reduction, healthy lifestyle can prevent the mortality and morbidity due to NAFLD.
Source: PIB
“Intensified Mission Indradhanush (IMI) 3.0”
What is the News?
Recently Union Health Minister launched Intensified Mission Indradhanush (IMI) 3.0 in India. After the launch, States and UTs have started the implementation of the IMI 3.0.
Development of Immunisation Programme in India:
- Ministry of Health and Family Welfare introduced the Immunization Programme in India in 1978. It was released in the name of ‘Expanded Programme of Immunization’ (EPI).
- In 1985, the EPI programme was modified as ‘Universal Immunization Programme’ (UIP). This was to be implemented in a phased manner to cover all districts in the country. Despite being operational for many years, UIP able to fully immunize only 65% of children in their first year of life.
- Mission Indradhanush:
- It was launched in 2014. The aim of the mission was to ensure full immunization with all available vaccines for children up to two years of age. Further, the mission aims to vaccinate pregnant women who were either unvaccinated or partially vaccinated under UIP.
- Diseases covered for Vaccines: Under the mission, vaccination is provided free of cost against 12 vaccine-preventable diseases. Such as Diphtheria, Pertussis, Tetanus, Polio, Measles, Rubella, severe form of Childhood Tuberculosis, Rotavirus diarrhoea, Hepatitis B, Meningitis & Pneumonia caused by Haemophilus Influenzae type B, Pneumococcal Pneumonia and Japanese Encephalitis.
- However, under Mission Indradhanush, Vaccination against Japanese Encephalitis and Haemophilus influenza type B is provided only in selected districts of the country.
- Intensified Mission Indradhanush(IMI)
- It was launched in 2017. The aim was to vaccinate each and every child up to two years of age. Apart from that, IMI also vaccinates all those pregnant women who have been left uncovered under the routine immunisation programme/UIP.
- Special attention was given to unserved/low coverage pockets and urban slums with a migratory population.
- Special vaccination drives were conducted under IMI. These drives aimed to ensure full immunisation coverage in 90% of select districts and cities by 2018.
- Intensified Mission Indradhanush (IMI) 2.0
- It was launched in December 2019. It aimed to achieve targets of full immunization coverage in 272 districts of 27 States. Full immunization of 652 blocks in Uttar Pradesh and Bihar also targetted. Hard-to-reach and huge tribal populated region were chosen as blocks
- The mission has a focus on urban, underserved population and tribal areas.
- IMI 2.0 also had Inter-ministerial and inter-departmental coordination.
- Intensified Mission Indradhanush (IMI) 3.0
- It aims to cover children and pregnant women who missed the routine immunisation during the COVID-19 pandemic.
- Beneficiaries from migration areas and hard to reach areas will be targeted.
- The mission will follow the COVID-Appropriate Behaviour(CAB) approach during the immunisation activities.
- States have been asked to follow a “staggered approach” (Staged approach) to avoid crowding at the vaccination sites.
- The vaccination sessions will be planned in such a way that not more than 10 beneficiaries will present at the session site at one given point in time.
- Source: The Hindu
Challenges in controlling Zoonotic diseases in India
Synopsis: India can turn into a hotspot for zoonotic diseases (diseases that spread from animal to human), if not controlled now. Research must be proactive as this could be a larger crisis than the COVID pandemic.
Introduction
During the covid-19 pandemic, Scientists developed tools to study the virus more effectively. Further, they also set up channels to test the efficacy of the Food and Drug Administration (FDA) approved drugs. But the challenges of Zoonotic diseases still exist.
Vulnerability of India to Zoonotic diseases:
Global meta-analyses mention that Zoonotic diseases are likely to emerge in areas with many mammal species. As per the analysis, high land use and land cover change, and high human population density are the reasons for zoonotic diseases.
- According to Global meta-analyses, India can be a hotspot for the possible emergence of zoonotic diseases in the world.
- India’s approach to addressing zoonotic diseases has mainly been reactive. This is evident as the research and public health intervention usually begin when there is an outbreak.
Challenges in controlling Zoonotic diseases?
There are several scientific challenges that exist in zoonotic diseases. They are,
- One cannot predict the zoonotic disease pandemic. This is evident from the recent Covid pandemic.
- It is hard to collect viral and bacterial samples from biodiversity. Collecting samples is nearly impossible from wild reservoirs like bats and rodents.
- It is impossible to monitor and control biodiversity hotspots. Further, the government cannot detect the transmission of the pathogen from one hot spot to another.
- Moreover, it is difficult to predict the evolutions of pathogens and their relation with the hosts (animals). It is also evident in the COVID pandemic.
Suggestions:
Scientists have to conduct interdisciplinary research and sustained efforts to reduce challenges. So, Scientists from various domains have to come forward and work for a common cause just like they did for covid testing and vaccinations.
Read Also:-
Clean drinking water to all: Initiatives and challenges – Explained Pointwise
Introduction
Recently Telangana government has achieved 100% tap water connections to all schools and Angan Wadi Centres (AWCs) under 100 day Special Campaign. The other states like Andhra Pradesh, Himachal Pradesh, Goa, Haryana and Tamil Nadu also achieved this target.
Under the Jal Jeevan Mission (JJM) the central government also aims to provide Functional Household Tap Connection (FHTC) to every rural household in India by 2024. Further, the recent budget expanded the Jal Jeevan Mission to urban areas as well. But to provide clean drinking water, the government has to do much more than just providing the water connections.
Important aspects of Jal Jeevan Mission
The JJM aims to envisage a supply of 55 litres of water per person per day. Important aspects of the Jal Jeevan mission are,
- The JJM will focus on integrated demand and supply-side management of water at the local level.
- It will implement source sustainability measures to recharge and reuse through greywater management, water conservation, rainwater harvesting.
- The Mission will converge with other Central and State Government Schemes to achieve its objectives of sustainable water supply management across India.
- The JJM will generate maximum community participation in the form of ‘Jan Andolan to achieve the target.
Other schemes aimed towards providing Drinking water
- Swajal Yojana: It is a community-owned drinking water program for sustained piped drinking water supply powered by solar energy. It was launched in 115 aspirational districts of India.
- Jal Mani Programme: It aims to provide value and quality addition to the ongoing Rural Drinking Water Supply Programme to mainly address the water quality. The aim is achieved by installing Stand-Alone Purification System in rural Schools
- Atal Bhujal Yojana: It is a Central Sector Scheme aims to improve groundwater management through community participation in identified priority areas in seven States
What are the advantages of providing clean drinking water?
- India will face fewer water-borne diseases. According to a study, more than 21% of the country’s diseases are water-related. In 2015 alone, India lost over 1 lakh children under the age of five due to diarrheal diseases. It is preventable if India provides clean water to its population.
- Fulfilling SDG: By providing clean water and sanitation to all, India can achieve Sustainable Development Goal 6 (clean water and sanitation for all). Along with that, India can also achieve other SDGs as well such as good health and well-being, etc.
- Recharge of groundwater level: According to NASA (National Aeronautics and Space Administration), India’s water tables are declining at the rate of 0.3 meters per year. Clean water through wastewater management may reduce the demand for groundwater. This will improve the groundwater table.
- JJM and other schemes provide employment opportunities. Successful implementation of the National Skill Development Mission has created a pool of skilled manpower in plumbing, masonry, fitting, electricity, etc. The JJM implementation will utilize their skills and also provide employment opportunities to the migrant labours returning home.
- For example, Recently Ministry of Jal Shakti deployed labourers returning to their homes due to the COVID-19 pandemic in the Jal Jeevan Missions.
- Better local infrastructure – Apart from solving the drinking water problem, the schemes will also improve better infrastructure facilities especially in rural India. Infrastructure facilities will be in the form of water management structures, supporting infrastructures in-home, streets, etc.
What are the challenges associated with providing clean drinking water?
- Water is a state subject. So, Centre intervention in this domain is limited. The States also look into the issue of drinking water problem as their individual problem (not the problem of other states). This leads to interstate disputes for water and prevents them from enacting a holistic solution.
- India doesn’t have enough water for its population. India has 16% of the global population, but only 4% of freshwater resources. One billion people in India are living in water-scarce areas. So, providing enough drinking water to all is a great challenge with limited resources.
- Providing quality piped water will be a great challenge. In the majority of the Metro cities and Urban areas, demand for water is higher than the supply. To compensate for the deficit, local authorities mix the surface & groundwater.
- Moreover, NITI Aayog report mentions nearly 70 percent of the country’s freshwater sources are contaminated. So it is impossible to ensure that quality water alone is supplied to homes.
- The “slippage” problem in India: Wide temporal and spatial variation of monsoon result in the slippage problem. For example, India receives 75% of its total rainfall during the four months-long monsoon season alone. So, there is a higher chance that drying up of the water source or collapse of the created facilities will create the problem of drinking water again in the earlier cover areas of schemes such as Jal Jeevan Mission.
- Reducing per capita availability of water in India is also a challenge. The Per capita availability was at 1816 cubic meters in 2001. But it reduced to 1545 cubic meters in 2011. Further, It is expected to reduce to 1367 cubic meters in 2031. In such a scenario Providing 19.02 crore, pipe connections will increase the demand for drinking water and reduce the per capita availability of water.
Suggestions to improve access to drinking water
- Providing clean drinking water needs a few corrections at the ground level. Such as,
- Artificial Recharge Techniques such as Rainwater Harvesting Systems in houses and localities should be mandatory. This will increase the Groundwater level in Indian villages.
- Government has to encourage local participation in water conservation by steps such as an awareness campaign.
- The government has to enact a specific plan for water-stressed states and water-stressed areas like the Hiware Bazar model of local-level water regeneration.
- Hiware Bazar is a village in Maharashtra’s drought-prone Ahmednagar district. Within a decade it changed from the water-stressed region to one of the most prosperous villages of the country. They achieve this by regenerating their natural resources such as forests, watersheds, and soil with local Panchayat.
- The government can explore the options of Pricing water used by well-off sections and agriculture. This fund can be used in the maintenance of the pipes and drains.
- Mandatory compliance: The sources, as well as the quality of water in the country, need to be maintained on a war front basis. The government can ensure mandatory compliance of local bodies to the Bureau of Indian Standards on water quality. This will ensure quality water at the local level.
- The government has to explore technological solutions in drinking water management. Such as establishing water treatment plants in water storage facilities to remove toxic inorganic pollutants and dissolved solids.
India cannot provide clean drinking water to people at the expense of depletion of the existing resources. It will take India, a step closer to the ground-zero level. At the same time, India cannot wait till the present population depletes the water resources. So, It is high time for the government to act on water conservation along with the aim of achieving clean drinking water for all.
A study on the cost of ensuring “WASH” in healthcare facilities
What is the News?
A study was conducted to estimate the cost of ensuring WASH (water, sanitation and hygiene) in healthcare facilities for one year across India. The study was published in BMJ Global Health journal.
What is WASH?
- The term “WASH in health care facilities” refers to the provision of water, sanitation, health care waste management, hygiene and environmental cleaning infrastructure, and services across all parts of a facility.
Key Findings of the study:
- The study estimates that improving WASH across the public healthcare facilities in India and maintaining this for a year would cost $354 million in capital costs. Further, it will need $289 millions as a recurrent expense (all payments other than for capital expenses like maintenance, electricity, rent, etc).
- The most costly interventions were providing clean water, linen reprocessing, and sanitation. Similarly, the least expensive were hand hygiene, medical device reprocessing, and environmental surface cleaning.
Impact of Poor WASH Facilities:
- A 2019 joint global baseline report by WHO and UNICEF had pointed out that globally, one in four healthcare facilities lacked basic water servicing. Further, one in five health care facilities had no sanitation service and 42% had no hygiene facilities.
Significance of providing WASH facilities:
- WASH will reduce deaths: Approximately, the death of 3 lakh children under five years can be prevented each year.
- Achieving SDGs: The status of WASH in healthcare facilities is an important issue in development. Ensuring availability and sustainable management of water and sanitation is one of the 2030 sustainable development goals.
- Infection prevention and control: The WASH interventions can help reduce healthcare-associated infections. Especially among the mother and neonates across the Indian healthcare system.
- Cost-effective intervention: In 2012, the WHO report calculated ‘For every dollar invested in sanitation, there will be a $5.50 gain’. This will be in the form of lower health costs, more productivity, and fewer premature deaths, etc.
Source: The Hindu
Read also:-
Why Complete Elimination Strategy of COVID virus is not feasible?
Synopsis: The empirical evidence shows that the idea of the complete elimination of COVID viruses in a selected few countries is not feasible. Rather, it will only increase the socioeconomic disparities thereby making the goal of elimination infeasible.
Background
- A recent article published in The Lancet has advocated for “elimination strategy”, it is also known as the zero-COVID-19 strategy for eliminating the virus.
- Zero-COVID-19 strategy means that the replication of the virus will be reduced to the least so that no new cases will occur in a defined geographical area.
- The elimination strategy has the following three elements,
- Rapid reduction in the number of infections to zero.
- Creation of virus-free green zones and
- Prompt outbreak management when new cases occur occasionally.
- Rich countries are working on this strategy by vaccinating each and every citizen.
- However, this strategy of the complete elimination of the virus is not suitable for every country.
Why this strategy is not suitable for all countries?
Complete elimination of the virus by vaccination is only suitable for geographically isolated countries such as New Zealand. It can afford strict border control measures. Even here, it is difficult because of the following reasons,
- First, the virus will be in circulation in the countries from each other. So, the threat of a Virus outbreak will stay for a while.
- Second, the Virus is mutating at a very fast pace. Universal vaccination will not be helpful against new variants. It is difficult to consistently upgrade vaccines.
- Third, a zero-COVID-19 strategy will worsen global health inequities. The idea of creating green zones for free travel will benefit richer countries and alienate poorer nations.
- Fourth, the experience from the elimination of other diseases shows that the complete elimination of the COVID virus is not possible. For example,
- Measles and neonatal tetanus are present for more than 20 years. It caused nearly 25,000 newborn deaths in 2018. Despite the global efforts for vaccination it still remains a major public health challenge in the developing world.
- Polio, eradicated from Southeast Asia, is still endemic in Afghanistan and Pakistan.
- Also, according to immunologists surveyed by the science journal Nature the Covid virus will become endemic in certain countries.
What are the Solutions?
Instead of isolated strategies for a few countries, global leadership and resources to vaccinate the vulnerable population are required.
- First, disease control measures should be implemented globally. The vaccine coverage for vulnerable populations across the globe should be increased.
- Second, the current pace of vaccination needs to be increased by 4.3 times to vaccinate 6.4 million persons per day.
- Third, along with this, mapping of elderly and persons with comorbidities needs to be done on a priority basis for vaccination.
- Fourth, there is a need to strengthen epidemiological and genomic surveillance for COVID-19.
- Fifth, a plan for the goal of achieving Universal Health Coverage (UHC) is required. Because the COVID-19 pandemic has reversed the gains made in other health programmes like tuberculosis control.
Thus, the idea of eliminating virus in a selected few countries should be replaced with a pragmatic goal of controlling COVID-19, not elimination. Since the zero-COVID-19 strategy comes with zero evidence of feasibility, focusing on it will result in wastage of our attention, funds, and time.
Importance of COVID 19 learnings in fight against tuberculosis
Synopsis: The COVID 19 pandemic has given an opportunity to India for combating other respiratory diseases like Tuberculosis (TB). The learnings from the pandemic can be used to control the spread of TB.
Background:
- The first case of COVID 19 was reported on 30th January 2020. After that, the disease claimed the lives of 1,54,000 people and infected 10.7 million in India.
- However, with robust efforts, the government managed to control its spread. Due to this, the country is not facing a brutal second wave as suffered by other countries.
- The number of active cases is decreasing since mid-September and people are getting back to their normal lives.
- The focus should now be shifted to other respiratory diseases like TB.
About Tuberculosis:
- It is a contagious infection that usually attacks your lungs. But can infect other parts like your brain and spine.
- It is a bacterial disease caused by Mycobacterium tuberculosis and affecting mankind for 3000 years.
- Furthermore, it is a disease with the ability to damage multiple organs which enhances mortality risks.
Issues with Tuberculosis:
As per World Health Organisation (WHO), India has more than 10 million active cases of TB. 4 lakh lives are lost per year due to TB and shares 1/4th of the global burden.
- First, It causes a disproportionate impact on the poor who live in overcrowded spaces and lack proper nutrition.
- Second, numerous myths and stigma are associated with the disease which discourages reporting and proper treatment.
- Third, it has become very difficult to control if multi-drug resistance gets developed or a person is already suffering from diabetes or HIV.
Using COVID 19 Lessons to combat TB:
- First, the PM must take a lead to sensitize the masses about the disease. It was done by him in the case of COVID 19, to induce behaviour change.
- Second, the concept of physical distancing can be effective in curtailing the spread. The droplets from one person will not reach another if the due distance is maintained.
- Third, patients, as well as nearby family members, must wear masks to curb the spread of infection.
- Fourth, improved detection techniques developed during COVID can be used to replace the traditional sputum tests. This would ensure better diagnosis and quick results.
- Fifth, in order to improve tracking and contact tracing, the focus should be on instant notification techniques.
- Sixth, awareness is developed around respiratory diseases. It can be used to build community-led participation and burst the stigma surrounding TB.
- Lastly, the enthusiasm shown by media and coordination shown by governments in tackling COVID-19 should also be carried forward to TB.
India has set a target TB elimination by 2025 which is 5 years prior to the sustainable development goals target. This can be achieved if COVID 19 learnings are aptly adopted in combating TB.
PM suggested “Special Visa Scheme” for medical staff in South Asia
What is the News?
During an address to 9 neighboring countries, PM suggested Special Visa Scheme. The address was part of a workshop on “COVID-19 management: exchange of good practices in tackling pandemic and the way forward”.
Participation: The countries that participated in the workshop include: Afghanistan, Bangladesh, Bhutan, Maldives, Mauritius, Nepal, Pakistan, Seychelles, and Sri Lanka.
Key Takeaways from the address:
- Special Visa Scheme: PM suggested considering a special visa scheme for doctors and nurses. It will help them to travel quickly within the region during health emergencies at the request of the receiving country.
- Regional Air Ambulance: The Civil Aviation Ministries from the neighboring countries can coordinate a regional Air Ambulance agreement for medical contingencies.
- Data on COVID-19 vaccines: The countries could come together to create a regional platform for collating, compiling, and studying data about the effectiveness of COVID-19 vaccines among our populations.
Source: The Hindu
A robust ‘health and well-being budget for 2021-22’
Synopsis: The government has come up with an integrated health and well-being budget for 2021-22. It would help meet the current and upcoming challenges created by the COVID-19 pandemic.
Background:
- The pandemic struck India in March 2020 and exposed the vulnerabilities of the Indian health care system.
- Although India’s performance in tackling the pandemic was better than various developed countries. But its impact on the economy and society was significant.
- It was therefore imperative to come up with a strong health and wellbeing budget to develop resilience against the ill effects of the pandemic. The health budget was prepared in this context of Atma Nirbhar Bharat Abhiyan.
Government measures for strengthening ‘health and wellbeing’:
- A Production linked incentive scheme is announced to boost the manufacture of pharmaceutical and medical devices.
- 35000 crore rupees has been allocated for the development of COVID-19 vaccine. Mission COVID Suraksha has been launched to improve indigenous vaccine testing and development. Further coverage of pneumococcal vaccine will also be enhanced.
- Pradhan Mantri Garib Kalyan Yojana (PMGKY) was launched to provide free food grains to 800 million beneficiaries.
- One Nation One Ration Card (ONORC) will target 690 million beneficiaries covering 32 states/UTs.
- Jal Jeevan Mission (JJM) has been given substantial allocation.
- There would be an expansion of health and wellness centres under Pradhan Mantri – Atmanirbhar Swasth Bharat Yojana (PMANSBY). It would also involve using a 13,192 crore Finance Commission grant for strengthening the primary health system.
- Allocation for the Pradhan Mantri Jan Arogya Yojana (PM-JAY) has not changed in comparison to last year.
- There has been a 40% increase in Budget of the Ayurveda, Yoga & Naturopathy, Unani, Siddha and Homoeopathy (AYUSH) ministry.
Significance:
- First, the nature of allocation strengthens the vision of making India Atma Nirbhar.
- Second, initiatives like Mission COVID Suraksha will help India sustain its position of being the vaccine hub of the world. Significant allocation towards vaccine development will also ensure all the citizens are able to get vaccinated in due time.
- Third, PMGKY and ONORC will help in ensuring food and nutritional security in the country.
- Fourth, a reduction in diseases namely Malaria, Polio and Diarrhoea would be seen due to substantial allocation towards JJM. This is explained by a report released by the Johns Hopkins Bloomberg School of Public Health in 2019.
- Fifth, focusing on capital expenditure through schemes like PMANSBY is a welcome step for strengthening the health system. Earlier the capital expenditure used to constitute only a small fraction of health allocation.
- Sixth, an improvement in AYUSH ministry’s budget will allow the country to focus more on preventive care and integrated treatment.
- Lastly, integration of health with well-being (Water, Sanitation and Nutrition) would help in improving the outcomes. Both National Health Policy, 2017 and Economic Survey have stressed the interdependence of these sectors.
Way Forward:
India’s commitment towards health has allowed it to successfully deliver 8 million doses of COVID vaccine to health and frontline workers. This is the fastest vaccination drive in the world.
- Allocation towards schemes like PM-JAY should be enhanced. A 20% decline was seen in infant mortality rate (IMR) between 2015-20 in states which adopted the scheme in comparison to a 12% in IMR decline in states which didn’t adopt it as per the economic survey.
- The states must increase their health spending to 8% of their respective budgets by 2022 as recommended by the National Health Policy and Finance Commission. This would reduce the burden on the Centre and ensure effective spending.
The Union Budget has effectively prepared the ground for tackling the upcoming challenges in the health sector. This should be coupled with other reforms so that the resilience capacity of the country gets enhanced. This would help in achieving the vision of universal health coverage by 2030 as part of sustainable development goals.
Significance of Telehealth services like Remote SMAs
Synopsis: The COVID-19 pandemic disrupted Normal health Services in India. The telehealth services like Remote Shared Medical Appointments (SMAs) should be used.
Background:
- The March 2020 lockdown reassigned healthcare professionals towards COVID-19 specific duties.
- This deviated the focus from other healthcare domains in India and across the world.
How Covid-19 disrupted normal Health care services:
- As per a survey of WHO, Essential services like immunization and childcare got disrupted in the majority of the 105 countries surveyed.
- Around 45% of low-income countries witnessed a disruption in 75% of services. While this figure for high-income countries was only 4%.
- Impacts on India:
- Fear of transmission and lockdown resulted in the fall of diagnostic services. In tuberculosis detection cases 50% fall was reported from April-December 2020. Whereas, in antenatal care visits 56% decline was observed during the first half of 2020.
- The inequalities got widened when people in rural and remote areas were not able to travel to cities for getting specialized care.
- However, the use of technology helped to mitigate the impact.
Virtual Consultation India
- The E-Sanjeevani platform of the Indian Government provides virtual consultations to patients. It includes patient-to-provider and provider-to-provider consultation.
- A hub and spoke model used for this platform. It connected smartphone-equipped rural wellness centres to specialist doctors located in cities.
- Private players and non-governmental organizations also used the technology for reaching out to patients.
However, given the scale of India’s population which is devoid of healthcare, a switch towards remote shared medical appointments is needed.
About Remote Shared Medical Appointments:
- Remote Shared Medical Appointments virtualizes the process of in-person shared medical appointments (SMAs). It is an effective practice in the US for more than 2 decades.
- Thus, It involves the virtual interaction of a doctor with multiple patients having similar issues.
- Advantages:
- Patients get more time with doctors.
- This process develops a sense of bonding among patients.
- This process provides better productivity as patients learn from each other’s questions.
Utility for India:
- SMAs have been very effective in the case of diabetes. It is notable that India is home to the largest number of diabetes patients.
- Aravind hospital in Puducherry has shown the potential of SMAs to combat glaucoma, a disease that causes gradual blindness.
- Offering this facility through the E-Sanjeevani platform can help the country meet the healthcare gap in rural India.
- SMAs will encourage people interaction and attract supplementary providers like physiotherapists and optometrists.
- The current COVID-19 vaccine drive will also be strengthened as providers can offer sessions to burst the myths related to vaccine efficacy.
Way Forward:
- The switch to a new technique of healthcare delivery will require adequate training and mentoring of both providers and patients.
- Collaboration with training platforms like ECHO is desired to encourage the adoption of virtual SMAs. It trains primary healthcare providers in multiple states.
- India is blessed to have very low data rates where 1.5 GB data/day is easily affordable for many Indians. This automatically gives the country a significant edge towards augmenting telehealthcare.
- Further, the strengthening of digital health services will also be in line with WHO’s Global strategy on Digital health. It would help in realizing the dream of ‘Health for All”.
Vaccination of manual scavengers must be prioritised
Synopsis: The government is focussing on the vaccination of frontline sanitation workers. However, the most vulnerable among them, Manual scavengers, did not gethe attention they deserve.
Introduction
India is far behind in understanding sanitation workers and their different categories. Manual scavengers belong to the lowest strata of unprotected sanitation workers.
Many people in India believe that manual scavenging is already eliminated since it is legally banned. However, the ground reality is very different.
- Sanitation workers can be categorized into Faecal sludge handlers, Sewage treatment plant sanitation workers, Toilet sanitation workers, public transportation site sanitation workers (railway, roads), Sewer and drain sanitation workers, Sanitation-waste intersection workers, Etc.
- Manual Scavengers are workers discarding human excreta manually, in any form.
The risk involved in septic cleaning among manual scavengers is the highest. One sanitation worker dies every five days. Waste recovery sanitation workers perform the work of manual scavenging as they come in regular contact with unprotected bio-medical waste, animal faeces.
Why sanitation workers should be included in priority population for vaccines?
Vaccination of sanitation workers should be prioritized due to following reasons:
- First, several laws banning this practice are not working properly on the ground. Sewer deaths continue to happen. Caste and economics have a role to play in the deprivation.
- Second, the absence of a policy for the protection of the sanitation workers resulted in the loss of many lives during the initial days of the pandemic. These cases are not even mentioned in the records of the National Commission of the Safai Karmachari (NCSK). The Safai KarmacharI Andolan (SKA) has had far better data.
- Third, there is no social security, no accountability in the actual expenses of the rehabilitation schemes. Even no definite provision for healthcare or pension is provided.
- Fourth, the representation of sanitation workers is not involved during creation of policies for them.
- Fifth, sanitation workers are prone to long-term diseases. In many cases, they don’t even live till the age of retirement. Their children suffer from malnutrition, TB, and cholera because of their habitation around the waste generated by the cities.
- Lastly, the sanitation workers worked full time to ensure safety for the people during the pandemic.
Way forward
The government must urgently prioritize vaccination for manual scavengers without giving the argument that they have already developed “herd immunity”.
“Traffic Crash Injuries and Disabilities” -World Bank report on road accidents in India
What is the News?
The World Bank released a report titled “Traffic Crash Injuries and Disabilities: The Burden on Indian Society”. It highlights the Socio-Economic impacts of road accidents in India.
About the Report:
- Published by: World Bank in collaboration with SaveLIFE Foundation.
- The report highlights the socio-economic impact of road accidents. It analyses the Medical care access and post-accident financial distress of various categories of people.
- The data was collected from Uttar Pradesh, Bihar, Tamil Nadu, and Maharashtra — a State each from northern, southern, western, and eastern regions.
Key Findings:
Road accidents in India:
- India tops the world in road crash deaths and injuries. It has 1% of the world’s vehicles but accounts for 11% of all road crash deaths. It is witnessing 53 road crashes every hour and killing 1 person every 4 minutes.
- India has seen around 4.5 lakh road accidents in the past year. It resulted in at least 1.5 lakh deaths over the past few years.
- According to a 2018 World Health Organization report, India tops the world in road crash deaths, with more than 400 fatalities per day.
Socio-Economic Impact of Road accidents in India:
- There are more fatalities from road crashes among poor families compared to rich families. The risk of a victim undergoing disability after a crash was also 2 times more likely among poor families.
- The socio-economic burden of road crashes is disproportionately borne by poor households. Accidents result in a decline of 75% of total household income among low-income groups. Whereas, the decline among high-income groups is only 54%. It underlines poor access to insurance schemes among the less privileged.
- Impact on Women: About 50% of women were severely affected by the decline in their household income after a crash. About 40% of women reported a change in their working patterns post-crash. While around 11% reported taking up extra work to deal with the financial crisis.
- Urban-Rural Divide: The severe impact of the decline in income was highest among poor households in rural areas (56%) compared to those in urban areas (29.5%).
- Insurance Coverage: There is an asymmetry in insurance coverage. About 1/4th of respondents from high-income households (24%) said that they received compensation. Whereas, among poorer respondents, only 14% received compensation.
Recommendations:
- There is a need to institutionalize post-crash emergency care and make health infrastructure and coverage more accessible and inclusive.
- The central and state governments should provide a social security net for crash victims from low-income households through state support.
- The Central government should create schemes to increase insurance coverage and penetration for low-income households.
Source: The Hindu
Budget 2020-21 didn’t address the core issues of ailing health sector
Source: Indian Express
Gs2: issues Relating to Development and Management of Social Sector/Services relating to Health.
Synopsis: Four important issues ailing the health sector did not find a place in the budget.
Background
- The budget allocation for the health sector in 2021-22 was (24 lakh crore) 137 % more than the previous year (69,000 crores).
- However, the actual share of Health and Family Welfare was only a third of the total allocation of Rs. 24 lakh crore.
- This is because, the increase in budget for ‘Health wellbeing’ also included funds for drinking water, sanitation, nutrition, AYUSH, health research, vaccination as well as grants assigned by the 15th Finance Commission.
- Also, a new centrally-sponsored scheme PM Aatmanirbhar Swasthya Bharat Yojana was announced as a part of Budget 2021-22.
- Even in this case, the funds allocated to this new scheme will be materialized only when the programmes are implemented.
What are the critical issues that have not been addressed by the Budget 2021-22 in the health sector?
Despite the above measures introduced in the Budget 2021-22, it has failed to address the four critical issues ailing the health sector. They are
- First, the Budget has failed to find a solution to bring down the costs of outpatient treatment.
- Under Aayushman Bharat, 50 crores of eligible poor people are entitled to cashless hospitalisation. However, the cost of drugs, the high cost of high-end diagnostics leads to high out-of-pocket expenditure before a patient needs hospitalisation.
- This ultimately reduces the number of people using affordable health care services. It defeats the very purpose of Aayushman Bharat.
- Second, Insurance coverage for the middle class is not adequate. Under the Ayushman Bharat health Programme, only 50-crore poor people are covered.
- Whereas another 10 per cent organised sector employees are covered by different government or employer generated medical coverage schemes.
- Still, around 30 crore Middle-Class Indians are without any state-supported medical insurance.
- Third, the Budget has failed to give effect to the 2017 National Health Policy recommendation. The Policy recommended for grading of clinical establishments to protect consumers rights. The states are not implementing the model Clinical Establishments Act 2010.
- Fourth, the need for a separate Empowered Medical Tribunal as recommended by 2017 National Health Policy, is not been addressed. The complexities of medical negligence or malpractice cannot be addressed by The Consumer Protection Act 1986. Thus, a separate health regulator on the lines of the State and Central Regulatory Commissions is critical for the health sector.
What needs to be done?
- A viable solution is required to reduce out of pocket expenditure in outpatient care services. This will make public health services affordable.
- Some international models can be analysed for health care funding:
- In Germany and France, health care is funded through mandatory contributions of both employer and employees.
- The Canadian model: The Canada Health Act of 1984 makes federal cost-sharing a government responsibility. Healthcare entitlements in Canada are also portable across the country.
- The Employees State Insurance Corporation scheme created in 1948 could also be modified and used to cover white-collar employees in the unorganized sector.
- Public health and hospitals can be brought on the concurrent list of the Constitution as recommended by the 15th Finance Commission. This will bring uniform principles and regulations throughout the state and ensures standards in consumer protection.
Men access “KIRAN mental health rehabilitation helpline” more
What is the News?
According to a report by the Ministry of Social Justice and Empowerment(SJE), 70% of callers to KIRAN (mental health rehabilitation helpline) are male.
Kiran helpline(1800-599-0019):
- Launched by: It was launched by the Department of Empowerment of Persons with Disabilities(DEPwD). The Department works under the Ministry of Social Justice and Empowerment (SJE).
- Purpose: It aims to offer support for mental health through experts. Support includes early screening, psychological support, distress management, mental wellbeing psychological crisis, and referrals to mental health experts.
- It offers this support in 13 languages for any individual, family, NGOs, parent associations, professional associations, rehabilitation institutes, hospitals, etc.
Key Findings of the report:
- The helpline received 13,550 new calls of which 70.5% were from males and 29.5% from females.
- The majority of callers (75%) were in the age group of 15 to 40 years, while others were older, in the 41 to 60 age group.
- Majorly the challenges faced by the callers were related to anxiety, depression, pandemic-related challenges, suicidal tendency, substance abuse, and miscellaneous.
- Most of the calls were from the North zone, followed by West, South, East, and North East.
Source: The Hindu
PM Atma Nirbhar Swasth Bharat Yojana
What is the News?
The Finance Minister has launched a new scheme titled “PM Atma Nirbhar Swasth Bharat Yojana”. In general, The scheme aims to develop capacities in the health care system over 6 yrs.
PM Atma Nirbhar Swasth Bharat Yojana:
- Type: It is a Centrally Sponsored Scheme
- Aim: The scheme aims to
- Improve primary, secondary, and tertiary care health systems,
- Strengthen existing national institutions in Health sector
- Create new institutions, to cater to detection and cure of new and emerging diseases.
- Duration of the Scheme: Six Years
- Features of the Scheme: The scheme will support in the setting up of
- Rural, Urban Health and Wellness Centres
- Integrated Public Health Labs
- Critical health care hospital blocks
- National institution for One Health
- Regional research platform for WHO South-East Asia Region,
- 9 Biosafety Level III laboratories and 4 regional centres of National Institutes for Virology.
- Strengthening National Centre for Disease Control (NCDC) and 5 regional branches of it
- Expanding the integrated health information panel.
Source: The Hindu
ICMR’s 3rd serological survey: Need to rethink on vaccination strategy
Synopsis: The recent findings of ICMR’s 3rd serological survey can be used to revalidate the vaccination policy of India.
Background
- The ICMR’s third serological survey findings were published at a press conference recently.
- However, the specific details of the course of the infection are not released. It will be made public later, in a peer-reviewed journal.
What is Serological Survey?A serological survey is conducted to assess the prevalence of a disease in a population. It is done by detecting the presence of specific antibodies that are produced against the virus.
What are the latest findings of ICMR’s 3rd serological survey?
- The findings show that nearly one out of five Indians (270 million) may have been infected.
- The report finds a three-fold rise in infections compared to August.
- Also, people who got infected in the age group of 10-17 years has increased 5 times (in percentage terms) compared to August.
- The serological survey of doctors, nurses, and paramedical staff reveals that nearly 25% of them had been infected. This is significantly above the national average.
- The survey findings cautioned that “Still, 80% of Indians are vulnerable”.
- But there is no information on the efficacy of antibodies against mutating virus strains.
What can be inferred from this result?
- Despite, the Experts pointing towards the declining trend in infections and increasing herd immunity among the population. We need to accept that the danger is still there.
- The survey highlights the need for vaccination and continuing with physical distancing and masking norms.
- There is also a rise in the spread of infection among teenagers and children. Rural India also facing an increase in infections. So the vaccine policy needs a course correction.
- So, it would be wise to rethink the vaccination policy to prioritize vaccination for children along with old age people, frontline workers, and peoples with morbidity.
“ICMR Serological Survey” -One in five Indians have been exposed to coronavirus,
What is the News?
Indian Council of Medical Research(ICMR) has released the third round of the Serological Survey.
Facts:
- Serological Survey: It is conducted to assess the prevalence of a disease in a population. It is done by detecting the presence of specific antibodies that are produced against the virus.
- How was the survey conducted? The survey used an antibody test. The test was designed specifically to check for antibodies produced against the spike protein.
- Spike Protein: Coronaviruses including SARS-CoV-2 get their name from the “corona” or crown shape, created by the protein “spikes” on their surface. These spike proteins bind with human proteins to initiate the process of infection.
Key Findings:
- Nearly one in five Indians which is around 21.5% had been infected by the coronavirus until December 2020.
- Urban Slums: The urban slums have reported the highest seroprevalence with 31.7% and was followed by urban non-slums(26.2%). The lowest was in rural areas at 19.1%.
- Children: The seroprevalence among children aged 10-17 years was around 25.3%.
- Health Care Workers: Nearly 26% of doctors and nurses and 25.4% of paramedical staff have coronavirus antibodies. It underlines their higher risk of being exposed to coronavirus infections than the general population.
- Women vs Men: There were more women (22.7%) as compared to men (20.3%) who were found to have antibodies against the Covid-19 virus.
Source: The Hindu
Vaccine battle among countries
Source: Click here
Syllabus: GS 2 – Health related issues
Synopsis: Countries should refrain from engaging in vaccine battles and focus on global cooperation.
Introduction
Almost all countries across the globe are in need of access to vaccines. But the developed countries are mindlessly collecting approved vaccines.
Only the countries in the global south like China and India are helping out other countries.
How are rich countries engaging in vaccine battles?
As per a few reports, the advance purchase contracts made by some countries for potential vaccine procurement are way above their need. It would vaccinate their population many times.
- For example, the EU population can be vaccinated two times, the US and the UK four times, and Canada six times.
- 82% of Pfizer’s production in 2021 and 78% of Moderna’s have already been advance purchased by leading countries.
Advanced countries are engaged in vaccine battles as they believe that an early vaccination will bring back normalcy in their countries. Concepts of Public good and global cooperation are missing from the scene.
What is India’s stance?
On the other hand, India is exporting a major percentage of the approved doses. Its initial shipment to the least developed countries will be free of cost.
Exports from India are helping other nations, especially its neighbouring countries. For example, Brazil has received 2 million doses of vaccine from India.
India’s approach supports the need for coordinated international efforts to bring COVID-19 under control.
Solutions
The COVAX project is a program based on funding from high and middle-income countries. It is a global risk-sharing mechanism for shared obtaining and fair distribution of COVID-19 vaccines.
This project aimed to deliver 2 billion doses by the end of 2021. But it is facing challenges from rich countries due to their excessive vaccine procurement, directly from suppliers.
But now as U.S. President Joe Biden has decided to join the COVAX project, expectations from the project are high. India, which is a hub of cost-effective vaccines, would be instrumental in its success. For example, Covishield, the Oxford University-AstraZeneca vaccine produced in India costs only $3 per dose; Covaxin is priced at $4.2.
The way forward
The development of vaccines should have shown global cooperation between the North and the South. But the democratic world is suffering from increasing democratic tendencies.
Medical boards for access to abortion untenable: Report
What is the News?
The Centre for Justice, Law and Society(CJLS), Jindal Global Law School has undertaken a study to analyse the feasibility of setting up Medical Boards. Boards are proposed in the Medical Termination of Pregnancy(MTP) (Amendment) Bill, 2020.Background:
- MTP Amendment Bill,2020: The Bill seeks to amend Medical Termination of Pregnancy (MTP) Act, 1971. It was passed in the Lok Sabha in 2020 and is likely to be brought before the Rajya Sabha during the Budget Session.
- Medical Board: The Bill proposes the constitution of a Medical Board in every State and Union Territory. These boards will decide on abortions in cases of foetal abnormalities where pregnancies are over 24 weeks. Each Board will have a gynaecologist, a radiologist or sonologist, a paediatrician, and other members prescribed by the governments.
Key Findings of the study:
- It found that the constitution of a Medical Board to decide on the termination of pregnancy is unfeasible. 82% of these posts are lying vacant in the country,
- Between 2015 and 2019, the shortfall in specialists posts was between 71% and 81.8%.
- The shortfall was more in the North-East states of Sikkim, Mizoram and Manipur. Arunachal Pradesh and Meghalaya had a 100% shortage of paediatricians.
Additional Facts:
Other key Features of MTP Amendment Bill, 2020:
- Abortion: The Bill allows abortion to be done on the advice of one doctor up to 20 weeks, and two doctors in the case of certain categories of pregnancies between 20 and 24 weeks.
- Special Categories: It has enhanced the gestation limit from 20 to 24 weeks for ‘special categories’ of women. It includes survivors of rape, victims of incest and other vulnerable women like differently-abled women and minors.
- Protection of Identity: It also states that the name and other particulars of a woman whose pregnancy has been terminated shall not be revealed.
Source: The Hindu
Lessons for India after one year of first Covid case
Source: click here
Syllabus: GS 3
Synopsis: One year has been passed when the first confirmed case was reported in India. What are the lessons that India Should learn from this Pandemic?
Introduction
India’s first confirmed case of Sars-CoV-2 was reported exactly a year ago. Experts with the help of a modeling-based study predicted that the country could have hundreds of millions of cases and a few million deaths by July 2020.
What were the challenges faced by people during the pandemic?
There was a sudden decrease in economic activities, low job opportunities, slowing of the economy. Impacts further worsened due to lockdowns.
- One of the most disturbing visuals that came from the pandemic was the migrants walking back to their villages on the highways.
- People who tested positive for the virus and the frontline workers were discriminated against in society.
- An excessive amount of unreliable information i.e. “infodemic” became a major obstacle in effective response to the pandemic.
What were the steps taken to deal with the pandemic?
Pandemic highlighted the need for strengthening the Indian health system and boost public health services.
- Firstly, COVID-19 specific services which include testing, contact tracing and treatment facilities were scaled up.
- Secondly, in order to achieve self-sufficiency, the production of personal protective equipment (PPE) coverall, testing kits, and ventilators was increased in India.
- Thirdly, researchers and scientists worked together to develop new testing kits, to conduct clinical trials on treatment procedures and vaccines.
- Fourthly, two SARS CoV-2 vaccines were approved in India and vaccination started at the beginning of 2021. The COVID-19 vaccines manufactured in India are being used in other countries as well.
What are the lessons learnt from the pandemic?
India has reported nearly 10.7 million confirmed cases and 1,53,000 deaths in the last year. Five lessons which should be learnt are mentioned below:
- First, the pandemic has widened the inequalities in the society as the poor and vulnerable sections were the worst affected. The government should urgently increase investment in strengthening health systems to address inequities and reduce poverty.
- This will prepare the country for future pandemics and help in accelerating economic growth.
- Second, Stronger health infrastructure is possible by interventions in various areas, such as:
- Governance and leadership.
- Health financing and health information system.
- Providing services and delivery.
- Health infrastructure and workforce.
- Medicines, diagnostics, and vaccines.
- Third, the hospital-dominated medical care system needs to be changed to a more inclusive health system for the lower section.
- Community clinics could be set up along with a strengthened primary healthcare system in both rural and urban areas.
- Fourth, states and the union government should spend more on health care and public health services. Laboratories and disease surveillance systems should be well-developed. The provision of mental health services via teleconsultation can be effectively used.
- Fifth, sustain the three-way partnership between policymakers, technical experts, and community members which have been formed for pandemic response.
- This would help in ensuring that health policies are informed, effectively implemented, and services widely used by the community. People’s participation and community engagement was important and need to be continued post the pandemic.
Way forward
- These learnings should be used to create a stronger healthcare system in India, which will provide accessible, available, affordable, and quality healthcare services to each and every citizen of this country.
What is Covid Performance Index?
What is the News?
The COVID Performance Index has been released by the Lowy Institute, an Australian think-tank.
Facts:
- COVID Performance Index: The index aims to rank the best-performing countries in their response to the pandemic. It measures the impact of geography, political systems, population size, and economic development on COVID-19 outcomes, for a conclusion.
- Measuring Indicators: To assess the performance of countries, the index tracked six measures of COVID-19 in the 98 countries for which data was available. The six indicators are:
- Confirmed cases
- Confirmed deaths
- Confirmed cases per million people
- Confirmed deaths per million people
- Confirmed cases as a proportion of tests
- Tests per thousand people.
- An average across indicators was then calculated for individual countries in each period and normalized to produce a score from 0 (worst performing) to 100 (best performing).
Rankings:
- India: India has been ranked at 86 out of 98 countries in the index.
- Topped by: New Zealand has topped the index followed by Vietnam, Taiwan, Thailand, and Cyprus.
- Bottom Countries: The United States has been placed at 94 and Brazil at the bottom of the index.
- South Asia: Sri Lanka was the best performing nation in South Asia ranking at 10, while the Maldives was at 25, Pakistan at 69, Nepal at 70, and Bangladesh at 84.
- Region-wise: The countries in the Asia-Pacific region did a better job at controlling the pandemic while Europe and the US were quickly overburdened by the COVID-19 cases.
- China was not included in the index due to a lack of publicly available data on testing.
Factors that played the role in the Performance of countries:
- Population size: Smaller countries with fewer than 10 million people consistently outperformed their larger counterparts throughout 2020.
- Levels of economic development or differences in political systems between countries had less impact on the handling of Covid-19 outcomes.
- Democratic countries have found to be marginally more successful than other forms of government in their handling of the pandemic.
Source: The Hindu
India ranks 10th in Asia-Pacific Personalised Health Index
Why in News?
Economist Intelligence Unit (EIU) has released the ‘Asia-Pacific Personalized Health Index’.India has been ranked 10th out of 11 Asia Pacific countries in the index.
Facts:
Asia-Pacific Personalised Health Index
- The index measures the progress of Asia Pacific countries in adopting personalised healthcare. It includes enabling the right care to be tailored for the right person at the right time.
- Countries covered: The index ranks 11 countries of Asia Pacific namely Australia, China, Japan, India, Indonesia, Malaysia, Singapore, South Korea, Taiwan, Thailand, and New Zealand.
- Indicators: It measures performance against 27 different indicators of personalised health across four categories called ‘Vital Signs’. These include:
- Health Information Indicator: It takes into account data, infrastructure, and technical expertise driving personalized healthcare.
- Health Services Indicators: It takes into account planning, organization, and delivery of services with respect to personalized healthcare.
- Personalized Technologies indicator: It takes into account the devices, applications, platforms, and reimbursement structures that will drive personalized healthcare based on the needs of stakeholders.
- Policy Context indicator: It takes into account the polities, frameworks, partnerships, people, and drivers that will facilitate personalized healthcare.
Other Takeaways from the index:
- Topped by: Singapore has topped the index followed by Taiwan (2nd), Japan (3rd), and Australia (4th).
- Bottom in the index: Indonesia was ranked 11th in the index.
Source: Indian Express
Every fourth senior citizen in India rates health as poor: LASI
Why in News?
The Ministry of Health & Family Welfare has released the Longitudinal Ageing Study of India (LASI) Wave-1 Report.Facts:
About LASI:
- About the study: It is a full-scale national survey of scientific investigation. It investigates the health, economic and social determinants and consequences of the ageing population in India. It was commissioned in 2016.
- Conducted by: The National Programme for Health Care of Elderly, Ministry of Health & Family Welfare. It undertakes the Study through International Institute for Population Sciences(IIPS), Mumbai in collaboration with Harvard School of Public Health, University of Southern California, USA, United Nations Population Fund(UNFPA) and National Institute on Ageing.
Key Findings:
Self Rated Health:
- Every fourth Indian above the age of 60 and every fifth Indian above the age of 45, reported poor health.
- The prevalence of poor self-reported health (SRH) in those above 60 (24%) is twice than in the 45-59 age group.
- Among these age groups, a higher percentage of women and individuals from rural areas reported poor health.
Disabilities among ageing Population:
- About 8% of Indians aged 45 years and above, reported having at least one form of impairment. The prevalence is almost twice among senior citizens(10.5%) than those between 45 years and 59 years.
- A high percentage of senior citizens in rural areas had a physical or mental impairment than their urban counterparts.
- The major disabilities reported are locomotive impairments (five per cent), followed by visual (three per cent), mental (two per cent), hearing (two per cent) and speech impairments (one per cent).
- Karnataka and Dadra & Nagar Haveli have the highest proportions of senior citizens with disabilities. Meghalaya, Lakshadweep, Haryana and Himachal Pradesh reported the least.
Additional Facts:
- According to the Elderly in India: Profile and Programmes, 2016, senior citizens comprised 21% of Indians with some form of disability.
- Disability: It is an umbrella term for impairments and physical limitations hindering the smooth activity and participation in daily social life.
- A decade of Healthy Ageing: The United Nations has declared 2021-2030 as the “Decade of Healthy Ageing”. It called upon governments, civil society, international agencies, and others to come together to improve the lives of older people in their families and the communities in which they live.
Source: Down To Earth
How should India handle the new virus variants?
Source: click here
Syllabus: GS 3
Synopsis: Mutation of the coronavirus has become a new threat for the world. India must take precautionary measures to deal with it.
Introduction
New SARS-CoV-2 variants have emerged independently in several countries and the virus is changing very quickly. If it continues to change, currently available vaccines will become ineffective.
Why do viruses mutate?
All the viruses carry a genetic code in the form of RNA or DNA. The DNA is replicated as the cells multiply and this process may cause random errors in the new DNA.
Errors in DNA can be corrected by the enzymes present in the cell. However, RNA doesn’t contain enzymes, thus errors caused in RNA cannot be corrected. It causes more genetic changes (mutations)in RNA than DNA viruses.
How are vaccines tested for efficiency against emerging variants?
- Indirect tests are conducted in labs. It will find if variant virus escapes antibodies developed after natural infection or vaccination.
- Antibodies that neutralize the original virus are tested on the variant viruses.
Are the emerging variants vulnerable to vaccines?
- The emerging variants from South Africa could pose a challenge to current vaccines. Not enough information is available yet for the Brazil variant.
- However, the studies have only tested antibody responses. Vaccines also increase cellular immunity to eliminate infection which has not been tested.
The evidence currently does not suggest that vaccines are failing.
- However, Moderna and Pfizer/BioNTech have agreed that their vaccines have had reduced protection against the South African variant. Both the companies are now working on developing new vaccines to fight these variants.
What steps should India take in this situation?
There is no local transmission of the new variants in India until now. Only the UK variant viruses have been found in travellers coming to India.
- Firstly, India should strictly implement masks and limit crowds. It should also do the contact tracing of people infected with the new UK variant.
- Secondly, India should also put a ban on travel from South Africa and Brazil just like the US did. India must also be cautious of people with a history of travel to South Africa since October 2020, and Brazil since December 2020.
- Thirdly, the most efficient way to catch emerging variants is increased genomic surveillance. So far, there are only about 5,000 SARS-CoV-2 sequences from India in public databases, which accounts for only 0.05 percent of confirmed cases.
The setting up of an inter-ministerial group -Indian SARS-CoV-2 Genomics Consortium (INSACOG) to increase genomic surveillance is a step in the right direction. India should take more such steps.
“BBV154” A Bharat Biotech’s Intranasal Vaccine vaccine
What is the news?
An expert body is looking into Bharat Biotech’s application for testing its Covid-19 vaccine, BBV154. This is an Intranasal Vaccine.What is Intranasal Vaccine?
- Vaccines are administered as injectable shots into the muscles(intramuscular). Or the tissue just between the skin and the muscles(subcutaneous).
- However, with intranasal vaccines, the solution is sprayed into the nostrils and inhaled instead of injecting it.
Benefits of Intranasal Vaccine:
- The nasal route has excellent potential for vaccination due to the organized immune systems of the nasal mucosa.
- It is non-invasive, Needle-free.
- Ease of administration – does not require trained health care workers.
- Elimination of needle-associated risks (injuries and infections).
- High compliance (Ideally suits for children and adults).
- Reduces the overall cost of a vaccination drive as for example BBV154 requires a single-dose regimen.
Potential Setbacks of Intranasal Vaccine:
- Past attempts to develop intranasal vaccines, including for measles flu, have not been very successful.
- These vaccines use live, weakened viruses, but have never cleared clinical trials.
- Only a live attenuated influenza flu vaccine has been licensed through this route of delivery.
Source: Indian Express
“Covaxin” is effective against U.K. virus variant
What is the News?
Indian Council of Medical Research (ICMR) and the National Institute of Virology(NIV) study found Covaxin effective against the new UK variant of Covid-19.About the Study:
- The study has found that Covaxin has a good neutralization capacity against the U.K variant of the COVID-19 virus. This capacity was the same against the strain used for making the vaccine.
How were the neutralization studies carried out?
- Under this study, the virus isolated from people is grown in the lab using cell lines. When viruses successfully grow in them, the pathogenic effects of the viruses are observed in the cells.
- The sera (the protein-rich liquid separated from blood after it is clotted) taken from vaccinated people are then added to the cell line culture system and its ability to prevent the virus from causing pathogenic effects is observed.
- In this case, the sera taken from vaccinated people were able to neutralize the virus and hence prevent pathogenic effects being produced in the cell lines containing the virus.
Source: The Hindu
Co-WIN platform upgraded
Why in News?
The Ministry of Health and Family Welfare has announced the upgradation of Co-WIN software. It is to cater to more sessions per site and change in site location.
Facts:
- CoWIN App: It is a digitalised platform by the Ministry of Health and Family Welfare (MoHFW).
- It allows Indian citizens to apply for a Covid-19 vaccine shot and helps agencies in keeping a track of Covid-19 vaccination programmes.
- Modules: The Co-WIN app comes with five modules namely –
- Administrator module: The admins will be able to track the information provided by citizens of India. They will also be responsible for creating sessions. By this app, respective vaccinators and managers will receive relevant notifications and alerts on the relevant information.
- Registration Module: Citizens who are not frontline health workers can register for the vaccine via the ‘Registration Module’. Photo identity will be required for registration.
- Vaccination module: It will verify the beneficiary details and update vaccination status.
- Beneficiary Acknowledgement Module: It will send SMS to beneficiaries and also generate QR-based certificates after one gets vaccinated.
- Report Module: It will prepare reports of how many vaccine sessions have been conducted, how many people have attended those, how many people have dropped out etc.
- What are the new features in the enhanced version?
- The enhanced version allows planning and scheduling the sessions for the entire week and works for the enhanced safety of the beneficiaries. These new features are being enabled in the vaccinator module.
Vaccine Maitri: India Vaccine diplomacy exercise
Why in News?
India will officially start its vaccine diplomacy with the name “Vaccine Maitri” under its Neighborhood First policy.
- Vaccine Diplomacy: It is the use of vaccines to increase a country’s diplomatic relationship with other countries.
Key Features of Vaccine Maitri
- India will supply Made-in-India Covid-19 vaccines to its neighboring and key partner countries Under its Neighborhood First policy.
- Bhutan and Maldives will be the first to get the vaccines followed by Bangladesh, Nepal, Myanmar and Seychelles.
- Sri Lanka, Afghanistan and Mauritius will also get doses once they give necessary regulatory approvals.
- Pakistan has not been named as a neighboring country which will get the vaccine.
- Vaccine will be Supplied to the partner countries in a phased manner, keeping in mind the demand.
Earlier Diplomacy measures by India:
- India had earlier supplied Hydroxychloroquine, Remdesivir and Paracetamol tablets as well as diagnostic kits, ventilators, masks, gloves and other medical supplies to a large number of countries during the pandemic.
- Under the Partnerships for Accelerating Clinical Trials(PACT) programme, India has also provided training to several neighbouring countries to enhance and strengthen their clinical capabilities
Additional Facts:
- PACT programme: It has been launched for supporting COVID-19 vaccine development activities in partnering countries.
- The initiative is being implemented by Biotechnology Industry Research Assistance Council(BIRAC) and Clinical Development Services Agency(CDSA) under the aegis of the National Biopharma Mission and Ind-CEPI Mission of DBT.
Need and ways of Decongesting Indian prisons
Synopsis: Health Experts are calling federal prisons a “breeding grounds for uncontrolled transmission” of the virus. There is an urgent need of decongesting them. What are the ways to decongest Indian prisons?
Background
- In India there are around 1,400 prisons, ‘housing’ over 5 lakh prisoners. These prisoners are facing the threat of Covid pandemic, with no organisational support.
- Whereas, in the countries such as U.K and U.S, activists are strong enough to influence public policy and voice against human rights abuse in prison.
- Also, these Countries have accurate data over the impact of pandemic on prisoners in public domain. For example
- The data from Texas state shows that the pandemic has killed more than 230 people in prisons, 80% of whom had not been convicted of a crime.
- Similarly, The United Kingdom Ministry of Justice figures shows that prisoners testing positive in October stood at 1,529, with five deaths.
- However, India lacks such crucial data on Prison Statistics in public domain and also such statistics are not being demanded of our criminal justice system.
How a lack of effective criminal laws is affecting under-trial prisoners in India?
According to the Prisons Act of 1894, prisons come under the exclusive responsibility of State governments. Over the years, despite being upgraded to the status of correctional homes, these prisons are facing the challenge of Congestion of Under Trial Prisoners (UTPs).
- According to the National Crime Records Bureau’s report for 2019 out of 4.5 lakh prisoners, 3.3 lakh are ‘under-trial prisoners’, i.e., investigation or trial is supposed to be ‘in progress’.
- These UTPs are detained under Section 167 of the Code of Criminal Procedure (CrPC) which provides for “Procedure when investigation cannot be completed in 24 hours”.
- The original Cr.PC of 1898 specified the period of detention as 15 days. Later, through amendments, it was extended to periods that can go up to 90 days and, in some exceptions, to an indefinite period.
- Out of 3.3 lakh, about 2.2 lakh are either not likely to be even charge-sheeted, or they are likely to be acquitted.”
- This is a huge violation of the basic human rights of UTPs, who are already facing the issue of inadequate healthcare facilities and torture by other rowdy prisoners.
- Moreover, it is a huge injustice to the families of the UTPs. For example, their children are denied a normal childhood, proper education, and are exploited by a cruel section of the society and are forced to take to the path of crime.
What needs to be done?
Pandemic provides an opportunity for an immediate review of all prisoners’ vulnerability to the epidemic,
- First, we need to conduct repeated testing in all prisons, especially sub-jails. An arrangement for the isolation and hospitalization of who testing positive needs to be planned.
- Second, to de-congest prisons, the Code of Criminal Procedure (Amendment) Act, 2005, which contains the much-needed Section 436-A needs to be activated.
- it provides for an under-trial to be released on a personal bond, with or without sureties if the under-trial has spent half of the period of prescribed imprisonment in detention.
- Third, ‘Prisons’ is purely a ‘State subject’. But it is imperative of the centre to support the states as the Constitutional responsibility of handling infectious and contagious diseases listed in the Concurrent List.
It is the duty of the state to vaccinate inmates at the ‘Hospitals of Correction’. It is similar to anyone in a state hospital may rightly expect to be vaccinated on a priority against the virus.
Covaxin not to be used in certain cases
News: Bharat Biotech has come out with a fact sheet about the process involved and who should avoid taking the Covaxin vaccine.
Facts:
- Covaxin: It has been indigenously developed by Hyderabad-based Bharat Biotech in collaboration with the Indian Council of Medical Research(ICMR).
- Type of vaccine: It is an inactivated vaccine. It means it is made by using particles of the coronavirus that were inactivated by making them incapable to infect or replicate. Injecting particular doses of these particles serves to build immunity by helping the body create antibodies against the dead virus.
Who should not get the Covaxin?
- During the first phase, experts are analyzing the behaviors of vaccines among different types of patients. They have recommended not to vaccinate if a person:
- has any history of allergies
- has a fever
- has a bleeding disorder or are on a blood thinner.
- is immune-compromised or are on a medicine that affects your immune system
- is pregnant or breastfeeding.
- has received another COVID-19 vaccine
- Has Any other serious health related issues as determined by the Vaccinator/Officer.
Article Source
Over 2.24 lakh vaccinated in 2 days, 447 adverse events: Centre
News: The Ministry of Health and Family Welfare has released the data on COVID-19 vaccination.
Facts:
Key Highlights of the Data:
- India has vaccinated the highest number of persons on the first day under its COVID-19 vaccination program. This is much higher than many other countries such as the USA, the UK and France.
- Around 2.24 lakh beneficiaries have been given COVID-19 vaccines in the first two days of India’s countrywide vaccination drive against the novel coronavirus infection.
- 447 cases of AEFI (Adverse event following immunization) have been reported. Most of the cases are minor and only three of the cases required hospitalization.
- According to WHO, Any untoward medical occurrence which follows immunization and does not necessarily have a causal relationship with the usage of the vaccine is known as AEFI.
Smokers, vegetarians are at lesser risk of getting infected by COVID-19: CSIR serosurvey
News: Council of Scientific and Industrial Research(CSIR) has conducted a pan-India Sero-survey tracking nearly 10,000 employees to study the prevalence of Covid-19. The study concluded Smokers and vegetarians were found to have lower seropositivity. So they may be at a lesser risk of getting infected by the coronavirus.
Facts:
Key Highlights of the Survey:
Source: The Hindu
Presence of Antibodies: The survey took samples of 10,427 adult individuals working in its laboratories or institutions and their family members to assess the presence of antibodies to SARS-CoV-2.It found 1,058 (10.14%) had antibodies against Covid.
- However, the neutralising antibodies that protect against the virus waned after infection but were at detectable levels even after six months — a proxy for the period of effectiveness of future vaccination and general immunity.
- Symptoms: About three-fourths of the respondents could not recall having experienced a single one of the symptoms commonly associated with the disease.
- Lesser Risk Group: Smokers and vegetarians were found to have lower seropositivity indicating that they may be at a lesser risk of getting infected by coronavirus.
- Blood Group: Those with blood group ‘O’ may be less susceptible to the infection, while people with ‘B’ and ‘AB’ blood groups were at a higher risk.
- Class Bias: There was also a distinct class bias in those affected. Those who work from home and able to access private transport were nearly twice less likely to be exposed to the virus than the outsourced staff involved with sanitation and security and using public transport.
Factsheet for administration of COVID-19 Vaccine released
Synopsis: Government has released a Vaccine Fact sheet that contains guidelines for administering both vaccines (Covaxin and Covishield).
Background
- Union Health Ministry has sent a comprehensive fact sheet for both vaccines (Covaxin and Covishield) to all states and immunisation officer.
- The Centre has also asked the states and immunisation officers to disseminate the fact sheet to all programme managers, cold chain handlers, and vaccinators before the rollout.
What is this fact sheet?
The fact sheet contains the general guidelines that should be followed during the initial phase of the Covid-19 vaccination drive, while vaccinating the priority group (3 crore people).
The fact sheet contains the guidelines on the following aspects,
- Physical specifications such as dosage, cold chain storage requirements.
- Specific guidelines on contraindications (a factor due to which the vaccine is to be withheld to certain categories of people)
- Guidelines on adverse events
- Details on special precautions.
Now we will examine in detail, the exceptions, precautions, and possible adverse events that are mentioned in the fact sheet.
First, the general guidelines in the fact sheet contain the following directives to ensure that proper care is taken while administering the vaccine.
- Only people over the age of 18 years are eligible for vaccination.
- Since 2 doses of vaccines are required per person, every Person should be administered the same vaccine in both the dosage. It is to deal with the issue of possible interchangeability.
- While administering the vaccine to a person with a history of any bleeding or coagulation disorder, platelet disorder, clotting factor deficiency, or coagulopathy, it should be done with caution.
- Both Vaccines have to be stored at +2°C to +8°C and needed to be protected from light. If it is found frozen it has to be discarded.
Second, the specific guidelines on contraindications. The three categories of people for whom the vaccine should not be administered. They are,
- Persons who have shown a history of an allergic reaction.
- People who show an immediate or delayed onset of an allergic reaction to vaccines or injectable therapies, pharmaceutical products, and food items.
- Pregnant and lactating women.
Third, guidelines on temporary contraindications. 3 categories of persons for whom vaccination is to be deferred for four-eight weeks. They are,
- Persons showing active symptoms of SARS-CoV-2 infection.
- Covid-19 patients who have been treated with anti-SARS-Cov-2 monoclonal antibodies or convalescent plasma.
- Acutely unwell and hospitalised patients (with or without intensive care) due to any illness.
Fourth, the fact sheet under not contraindicated, specifically mentions that persons suffering from following health conditions can get vaccinated. However, the response to the Covid-19 vaccine may be less in these individuals. They are;
- Persons with a past history of Covid-19 infection.
- Persons with a history of chronic diseases and comorbidities (cardiac, neurological, pulmonary, metabolic, and malignancies).
- Persons with immunodeficiency or HIV, and patients on immune suppression due to “any condition” can be administered with the Covid-19 vaccine.
Fifth, the fact sheet has also separately mentioned the Possible Adverse Reactions for both the vaccines along with the required precautions to be taken during the adverse reaction.
Guidelines provide the list of mild adverse events and rare adverse events that may follow the vaccination from both Covishield and Covaxin. It also provides for the precautions and medication that will be required in the above cases.
For example; In case of Mild adverse events for Covishield like myalgia (deep muscle pain), malaise (a feeling of overall discomfort), common painkiller paracetamol may be used.
How Covid-19 vaccines administered in other countries have performed till now?
Though the overall performance is found to be safe so far, there were few adverse events recorded in a small section of the population. For example, in the case of the US,
- The US Centers for Disease Control (CDC), monitoring by the Vaccine Adverse Event Reporting System detected 21 cases of anaphylaxis (a severe, life-threatening allergic reaction that occurs rarely after vaccination) out of a reported 1,893,360 first doses of the Pfizer-BioNTech vaccine.
- Whereas in the case of Modern’s mRNA vaccine, which was authorized for emergency use in the US, the CDC said data is still limited.
Strategic guidelines for COVID vaccine program: Challenges and suggestions
Synopsis: Government has issued strategic guidelines for the effective rollout of COVID vaccine program. There are challenges in the way of the Vaccine program that should be tackled as soon possible.
Strategic guidelines for COVID vaccine programme
With limitations of Vaccine related to efficiency and efficacy in mind, government has framed strategic guidelines for COVID vaccine programme
- Guidelines were framed using the knowledge acquired over three decades of implementing the Universal Immunisation Programme. It aims to aims to cover 30 crore people by July 2021.
- It has specified involvement of 19 departments, donor organisations and NGOs at the national, state, district and block level in the roll out of COVID vaccine programme.
- The guidelines have also clearly mentioned the priority criteria. Citizens eligible for the first round of COVID vaccine programme includes the following,
- The caregivers and front-line workers working under the department of health, defense, municipalities, and transportation.
- Persons above the age of 50.
- And persons below the age of 50 who suffers from comorbidities such as diabetes, hypertension, cancers, and lung diseases are all included.
- The strategic guidelines have also clearly stated in detail,
- The skills, roles, and responsibilities of the required human resources.
- The quantum of logistics required for delivering vaccines at point of use.
- The requirement of physical infrastructure, monitoring systems based on digital platforms, and feedback systems for reporting adverse events.
However, it has been criticised that the guidelines are ideal and have failed to provide solutions for real-time issues of our health system.
What are the challenges involved in effective rollout of COVID vaccine programme?
There are many challenges to roll out COVID vaccine programme. They are,
- First, unequal distribution of cold storage facilities among states. For example, out of the 28,932 cold chain points, half are in the five southern states, Maharashtra and Gujarat.
- Whereas the eight states in the North and Odisha that account for over 40 per cent of the country’s population have only 28 per cent of the cold chain points.
- Second, pertaining issues in our health care sector such as poor human resources, a weak private sector, poor safety and hygiene standards, frequent power outages, poor infrastructure will reduce the capacity to implement the vaccine programme with speed, quality, and accuracy.
- Third, a massive immunization programme for 30 crore people can distort the routine health service delivery and affect other immunisation drives, and can lead to exhaustion of health care workers.
- Fourth, acquiring the data for under the 50s with comorbidities will be challenging though we have data for the above-50-year-olds in the electoral rolls.
- Fifth, there are also challenge of tackling Fudging, false certification, and siphoning off vaccines to private facilities in the event of vast price differences between private hospitals and public hospitals.
- Sixth, the non-availability of efficacy data could result in huge wastage and gives scope for errors and duplication during the procurement and supply of vaccines.
- Seventh, the trust among the people on COVID vaccines are decreasing leading to suspicions and fears due to various reasons such as
- Non-transparency of data on either of the two vaccines proposed for use in the program.
- Opacity with which the licenses were given etc. For example, have not completed the Phase 3 trials that confirm the safety and efficacy of the vaccine.
- Above all, India hasn’t signed the advance purchase agreements for vaccines that have completed Phase 3 trials from other countries.
What is the way forward?
- First, avoid the complexity of listing the priority groups throughout our country. It should be replaced by covering the complete area in one go, instead of sequencing them into different groups.
- The areas could be ranked on the basis of a vulnerability index based on disease burden, caseload of COVID infections, demographic profile, health-seeking behavior and availability of infrastructure, etc.
- Second, to create confidence in the community we need to establish an independent team of experts under the aegis of the WHO to ensure adherence to recruitment standards, consent conditions, adverse event record management, compensation standards.
- Third, to build trust about vaccination programme we need to plan for large–scale public education and information programme through State- and local-level networks where people are informed, sensitised and their feedback was taken.
- Fourth, People should be involved in decision-making. For this Local leader from public figures, religious leaders, self-help groups, the media, and even educational institutions need to participate to help citizens understand its importance and build trust
- Fifth, Science, evidence, and data analytics need to be extensively used for effective policymaking.
- Finally, vaccination is not a complete solution to end the epidemic. We need to adopt safe behavior through a communication strategy. For this, the government can use its experience of controlling the HIV/AIDS epidemic.
The need of the hour is a winning strategy against epidemic that has drained us economically, socially and psychologically. Government needs to understand that the effective way of improving uptake of the vaccine while reducing costs is by creating participatory frameworks of engaging experts and communities and building effective and reliable public information, and transparency.
BARC Develops India’s First Ruthenium 106 Plaque For Effective Eye Cancer Treatment
News: Bhabha Atomic Research Centre(BARC) Mumbai has developed an Eye Cancer therapy. It was the first indigenous Ruthenium 106 Plaque for the treatment of Ocular Tumors.
Facts:
- Ruthenium-106: It is a radioactive form of the rare heavy metal ruthenium. It is a “platinum group” metal similar to platinum.
- How is it produced? It is produced from the fission or splitting of uranium-235, the type of uranium used in nuclear fission reactors, so it’s found in spent nuclear fuel.
- Uses: It is used in medicine for cancer radiation therapy, especially for eye and skin tumors. It is also used in radioisotope thermoelectric generators that power satellites.
- Harmful to Humans: High doses of ruthenium are toxic and carcinogenic when ingested. The material is strongly retained in the bones.
Issues in the process of COVID Vaccine trial
Synopsis: Many issues have been highlighted in the Phase-3 trial of Bharat Biotech’s COVID-19 vaccines. Those issues could have been avoided after HPV vaccine trial controversy.
Introduction
In a previous case, Human papilloma virus (HPV) vaccine trial was carried out on nearly 23,500 girls in the 10-14 age group in Vadodara, Gujarat and Khammam without proper consent. Almost eight years later the Supreme Court of India criticized the government for its inability to take action on illegal clinical trials carried out in India by multinational countries.
Present situation of the approval process in India suggests nothing much has changed.
- The phase-3 clinical trial of Bharat Biotech’s COVID-19 vaccine resembles the HPV vaccine because it seems that the trial is suffering from serious violations.
- The ICMR which has assigned the task of promulgating research ethics guidelines is also the cosponsor of the Covaxin trial.
What are the problems in the Covaxin phase 3 trial?
After the 2013 SC order, The Indian regulator made audio-video recording of the informed consent of each individual participant mandatory in 2019. Written consent from the participant had to certainly be taken before the audio-video recording.
However, the process was not followed properly;
- Firstly, no efforts were made to explain and inform the participants about the pros and cons of taking part in the trial instead; they were deceived by the trial site to think they were getting a COVID-19 vaccine for free.
- Secondly, many participants didn’t know about their rights to get free medical care in case of any adverse events.
- Many aware participants sought medical help from private practitioners whereas some of the participants don’t possess mobile phones, thus medical follow-up was not possible.
- Thirdly, not enough time was given to discuss with the family before signing the consent form. At least in a few instances, the consent was taken after vaccination, which is a serious violation.
- Participants were not given a copy of the consent form and other documents to prove their participation.
- Fourthly, 700 participants in the trial were illiterate and there is no evidence that an impartial witness was present during the entire informed consent process to attach his/her signatures to the consent form.
- Fifthly, communities living close to the hospital have told the media that they were offered ₹750, and luring people in trial for money is unethical.
- Although the company maintained that the amount was the reimbursement for the transportation and loss of wages, an open announcement of remuneration was unethical.
- Lastly, it is not yet confirmed that institutional ethics committee approved the advertisement for inviting people to the trial, in lieu of money.
Way forward
- India has already approved 2 vaccines for restricted use and the virus spread slowing down, so enrolling participants will be more challenging. Therefore, a thorough and impartial inquiry will bring back confidence in clinical trials.
Union Minister inaugurates 5th National Kayakalp Awards
News: Union Minister of Health and family Welfare has inaugurated the 5th National Kayakalp Awards.
Facts:
- National Kayakalp awards: It was launched by the Ministry of Health and Family Welfare in 2015 as part of the Swachh Bharat Abhiyan to ensure hygiene, sanitation and cleanliness in Public Health Facilities in India.
- Aim: The award recognises and facilitates those District Hospitals, Sub-divisional hospitals, Community Health Centres, Primary Health Centres and Health & Wellness Centres in the public healthcare system who have achieved high levels of cleanliness, hygiene and infection control.
- Parameters: The parameters on which the performance of the facility would be judged are as follows: 1) Hospital/Facility Upkeep 2) Sanitation and hygiene 3) Waste Management 4) Infection control 5) Support Services and 6) Hygiene Promotion.
- Assessment: The assessment of these parameters are done sequentially through a three tier system – internal assessment followed by peer assessment and then external assessment.
- Significance: The success of Kayakalp has been internationally applauded during the 72nd World Health Assembly, held on 20-28th May 2019. The success of Kayakalp was also duly recognized in Global Baseline Report 2019 published by WHO, UNICEF and JMP.
Additional Facts:
- Swachh Swasth Sarvatra: It was instituted by the Ministry of Health & Family Welfare (MoHFW) & Ministry of Drinking Water and Sanitation (MDWS) in 2016 under Swachh Bharat Mission.
- Aim: To strengthen Community Health Centres in open defecation free (ODF) blocks across the country along with behavioural change to enable them achieve higher levels of cleanliness and hygiene with the goal of making India free of open defecation.
- Objectives: The Three broad objectives of this scheme are:-
- Enabling Gram Panchayat where Kayakalp awarded PHCs are located to become ODF.
- Strengthening Community Health Centre (CHC) in ODF blocks to achieve higher level of cleanliness to meet Kayakalp standards through a support of Rs 10 Lakh under NHM.
- Build capacity through training in Water, Sanitation and Hygiene (WASH) Of nominees from covered PHC and CHC.
Formalising the work of community workers
Synopsis: Government should strive to formalise the work of community workers such as Anganwadi, ASHA and National Health Mission workers to make them accessible for various social security benefits such as safety, insurance, risk allowance and fixed wages etc.
Background
- In India, there are about a lakh ASHA worker, 1.3 million Anganwadi workers and another 1.2 million Anganwadi helpers. (Community workers)
- At present, community workers are classified as “honorary workers” and are denied of minimum wages, leave and other conditions that is available to formal workers.
- Even in the best paid states, this honorarium is not even close to the government-mandated minimum wages offered to workers doing comparable jobs.
- Also, the state by preferring to call them as “volunteers “denies the opportunity to recognise their crucial work as care service providers.
- This led to the two-day nationwide strike by Anganwadi, ASHA and National Health Mission workers demanding safety, insurance, risk allowance and fixed wages during the pandemic
What is the importance of community workers to society?
- Firstly, during the COVID-19 the Accredited Social Health Activists (ASHA) and Anganwadi workers, women “volunteers” functioned as the frontline warriors in the battle against the pandemic.
- Second, these community workers serve as the connecting link between the community and the state machinery. This was very much visible when there was uncertainty and fear of the virus.
- Third, the services of community workers are essential to facilitate localised approaches to problems as they have robust contacts at the grass roots.
What is the way forward?
- Firstly, there is an urgent need to recognise Community workers as workers. It can be done by Implementing the recommendation of Parliamentary Standing Committee on Labour to formalise the work of community workers.
- Second, Recognition of care work in the public sphere could also help in settling the issue of gendered and unequal division of house work and unpaid care burden.
It is high time that the state recognises the contributions of these women and accept them as workers. The recognition of ASHA and Anganwadi volunteers as workers will be a tribute to their contribution during the pandemic and also it gives a fresh start towards the structural understanding of women’s labour and their status in the labour market leading to Gender sensitive policy making
Explained: The return of bird flu
News: After bird flu (avian influenza) was confirmed in Kerala, Rajasthan, Madhya Pradesh, Haryana, and Himachal Pradesh, high alert has been sounded in several states which have been reporting deaths of birds, including crows and migratory species.
Facts:
- Bird flu or avian influenza: It is the name used to describe a viral infection that is reported mostly in birds but has the potential to affect humans and other animals.
- Common Strain: The most common strain of the virus that causes severe respiratory disease in birds is H5N1; various other strains like H7, H8 too, cause infection.
- Origin: The virus was first reported in geese in China in 1996.Since then, outbreaks have been reported periodically across the world. India reported the presence of the virus in Nandurbar, Maharashtra, in 2006.
- Human Transmission: The H5N1 virus can jump species and infect humans from the infected bird. The first case of H5N1 infection in humans was reported in Hong Kong in 1997 when a poultry farm worker caught the infection from infected birds.
- Human-Human Transmission: The high mortality rate in humans almost 60% is the main cause of concern about the spread of bird flu. However, in its present form, human-to-human infection is not known — human infections have been reported only among people who have handled infected birds or carcasses.
- Current Situation in India: Currently, samples from Rajasthan, Madhya Pradesh, and Kerala have tested positive for the A (H5N8) strain of the virus, while samples from Himachal Pradesh have shown the presence of A (H5N1).Most infections have been reported either in wild birds, crows or migratory birds.
- Is India’s Population Vulnerable to Bird Flu? Experts have said that the chances of the H5N1 virus infecting humans is comparatively low in India as compared to South East Asian countries mainly because both meat and eggs in India are eaten well-cooked which sees them being exposed to over 100 degrees Celsius. Thus the chances of humans contracting the virus from eating chicken and eggs is extremely rare.
How to deal with Avian influenza?
Synopsis: Avian influenza must be stopped before continuous spread amongst humans.
Influenza type A viruses cause Bird flu, a highly contagious viral disease. Normally birds are carriers of this virus, takes it across the continent, though unaffected themselves, affect a large population of other birds.
These viruses mainly affect poultry birds such as chickens and turkeys. Although rare, this virus sometimes also affects mammals such as pigs, horses, cats, and dogs.
H5N8 and H5N1 are subtypes of avian influenza Virus:
- H5N8 has been found in crows in Madhya Pradesh and Rajasthan.
- H5N1 strains have been found in ducks in Kerala and migratory birds in Himachal.
Introduction
The highly pathogenic avian influenza subtypes named as H5N1 and H5N8, have been reported in Rajasthan, Madhya Pradesh, Himachal Pradesh, and Kerala.
- Death count of poultry birds in Haryana is in thousands followed by Jharkhand and Gujarat. The cause of death in these three States is still unidentified.
- Crows in Rajasthan and Madhya Pradesh, migratory birds in Himachal Pradesh, and poultry in Kerala have been targeted by the two subtypes of the virus.
- Tests have confirmed H5N1 is responsible for the deaths of over 2,000 migratory birds in Himachal Pradesh.
- H5N8 has been recognized as the cause of deaths of thousands of poultry in Kerala, and hundreds of crows in Rajasthan and Madhya Pradesh.
What is the origin of the spread of the virus and its causes?
A European Food Safety Authority report revealed that 561 avian influenza discoveries were made between August-December in 15 European countries and the U.K.
- H5N1 and H5N8 were two of three subtypes found in Europe, these were mainly found in wild birds along with a few poultry and captive birds.
- Migratory birds have been largely responsible for spread of the virus into India during winter. It spreads further through movement of local residential birds and poultry.
- Genetic analysis suggested that a tenacious transmission of this virus strain is coming from wild birds in Asia to west-central Europe.
- Movement of men and material from poultry farms has also been a cause for the further blowout.
What is being done to stop the spread?
- Firstly, more than 69,000 birds which included ducks and chickens were culled in Alappuzha and Kottayam in accordance with India’s 2015 national avian influenza plan, in an attempt to stop the spread.
- Secondly, all the states have been asked to be watchful of any unusual deaths or disease outbreak signs amongst birds, particularly migratory ones as they are considered to be one of the causes of the spread.
- Thirdly, states have been asked to disinfect and dispose of the dead birds properly, biosecurity of poultry farms needs to be strengthened.
Conclusion
- It is very rare that avian influenza viruses cross the species barrier and directly infect humans but mutations in the virus can create a new avian influenza virus which can result in continuous transmission between humans, leading to genesis of pandemic influenza.
- Hence, it is suggested to carry out genome sequencing of virus samples to track the evolution of the virus.
Preparing workforce for COVID vaccination
Synopsis:India is near vaccine roll out, but it lacks trained healthcare workers for the job.Introduction
The permission of two COVID-19 vaccinats for emergency use is nearing. There is now hope of an end to the pandemic. But for the administration of vaccination and treatment properly and skillfully, a trained and effective workforce is required.
Present strength of healthcare workers in India
- In India, over 4,00,000 frontline workers have been trained to respond to COVID-19.
- However, this includes people with no prior experience also. Thousands have been trained for (1) contact tracing, (2) quarantine strategies, (3) ventilator management, (4) personal protective equipment, and (5) psychological issues.
In this context, Project Echo provides a cost effective way if ncreasing our workforce – both number wise and qualitywise.
What is project ECHO?
India was a recipient of an effective global innovation called Project ECHO.
- ECHO is a low-cost way out for growing the size of health workers in underserved communities to offer patients with the best possible care and facilities.
- ECHO was utilised as a strategy for treating Hepatitis C in the beginning but now is being used for newly trained experts in HIV, malaria, tuberculosis, addiction, mental health, and many other conditions.
- Under this project, health workers, nurses and doctors are trained through video conferencing technology. They learn speciality care from subject matter experts and from each other’s community informed knowledge.
- ECHO provides the ability to spread healthcare workers in the most remote areas of the country and give them training similar to what a healthcare worker in one of our largest cities would receive.
What needs to be done before the vaccine arrives?
India is led by the Serum Institute of India which has the largest manufacturing capacity in the world. However, certain aspects need to be figured out and planned before the COVID-19 vaccine becomes widely available:
- Firstly, real skills need to be cultivated for planning out the following:
- Delivery system of these vaccines needs to be figured out.
- Storage and handling of the vaccines.
- India needs to overcome cultural and religious obstacles for those who are unwilling to accept a vaccine.
- People need to be counselled about the side-effects of the vaccine.
- Secondly, more trained health experts are required to support vaccine treatment.
- Thirdly, further preparation of the ECHO model can be done to identify new healthcare workers who can be trained to be COVID-19 experts.
NFHS-5 data suggest improvement on various social indicators
Synopsis: Overall trends of NFHS data suggest an improvement in population control, use of modern contraception, reproductive and child health, immunisation and social determinants of health.
Introduction
The National Family Health Survey-round 5 (NFHS-5) covers about 6.1 lakh sample households to provide estimates for 707 districts. In the first phase, data from 22 states and UTs has been released from the latest survey conducted in 2019-2020.
What are the major findings in the first phase of the report?
- One, the data on Total Fertility Rate (TFR) has come down to 2.1 or below (replacement level) in all states and UTs. Bihar (3), Meghalaya (2.9) and Manipur (2.2) are exceptions in this.
- Two, the data shows that the overall use of modern methods of contraception has increased in 20 out of 22 states. The most dominant method being female sterilisation.
- Three, the data confirms that the number of women marrying before the legal age has reduced in 17 out of 22 states and UTs, with Nagaland, Maharashtra, Jammu & Kashmir and Sikkim as the top performers.
- Indicators on teenage marriage and childbearing have also improved in 17 states/UTs.
- Four, 17 of 22 states/UTs saw an increase in antenatal care visits during the first trimester (Nagaland, Bihar and West Bengal saw the highest rise).
- Five, the data shows consumption of IFA tablets by pregnant women for 180 days or more has increased in almost all states/UTs (except Karnataka) albeit this has not resulted in reduction in anaemia levels among pregnant women.
- There is a need to consider adding IFA tablets which contain more natural sources of iron, folic acid and other micronutrients in the diet.
- Six, 14 out of 22 states and UTs had more than 90 percent of new-borns delivered in institutional facilities and 14 out of 22 states/UTs have seen a drop in neonatal mortality.
What does the NFHS data suggest on the indicators of women empowerment?
Women’s empowerment is a widespread concept. However, indicators like household decision making, control over personal hygiene choices and possessions like bank accounts and mobile phones are decent indirect means for evaluation.
- The data indicates that the majority of women (80 percent) participated in at least three household decisions.
- Hygienic methods of protection during menstruation are being used by more than 64 per cent of younger women in each of the 22 states/UTs, except Bihar at 59 per cent.
- Personal possessions such as mobile phone and bank account have increased to over 70 per cent across each of the 22 states/UTs of India (except Nagaland) in 2019-2020 amongst women.
What does the NFHS data indicate about the public health in India?
- All states and UTs show a drastic increase in the number of households with a constructed toilet, improved drinking water and clean cooking fuels which are the indicators critical in improving public health in India.
- There has been a rise in malnutrition rates, wasting and underweight children in half of the states which reported an increase in exclusive breastfeeding and adequacy of diets.
- Stunting can be affected by multiple factors such as indicators of the mother a child, financial situation, adequacy of diets, water and sanitation facilities, as well as interventions for nutrition promotion and health.
- NFHS-5 data also show an increase in the rates of obesity in children and risk factors for chronic diseases in adults like hypertension and blood glucose.
Conclusion
One should not simplify these results for the whole country because data from phase 2 is yet to come and summary figures may oversee how relative health and nutritional results of the population can be.
Read more : National Family Health Survey
Status of Avian Influenza(AI) in India
News: In a bid to curb the spread of the bird flu or avian flu viruses, Central Government has set up a control room in the national capital to monitor the situation and take stock on a daily basis of the preventive and control measures undertaken by the state authorities.
Facts:
- What is Bird Flu or Avian Influenza? It is a highly contagious viral disease caused by Influenza Type A viruses which generally affects poultry birds such as chickens and turkeys.
- How does the bird flu spread? Wild aquatic birds such as ducks and geese are the natural reservoir of Influenza A viruses and the central players in the ecology of these viruses.
- Many birds carry the flu without developing sickness and shed it in their droppings.Since birds excrete even while flying, they also provide a nice aerosol of influenza virus, shedding it all over the world.
- Symptoms: Unlike in birds, where it generally infects the gut, the avian influenza attacks the respiratory tract of humans and may cause severe respiratory illnesses such as pneumonia or Acute Respiratory Distress Syndrome (ARDS). Its early symptoms include fever, cough, sore throat, and sometimes abdominal pain and diarrhoea.
- Treatment: Antiviral drugs, especially oseltamivir, improve the prospects of survival in humans.
- Bird Flu in India: India notified the first outbreak of avian influenza in 2006.Infection in humans is not yet reported in India though the disease is zoonotic.There is no direct evidence that AI viruses can be transmitted to humans via the consumption of contaminated poultry products.
- In India, the disease spreads mainly by migratory birds coming into India during winter months i.e. from September – October to February – March.The secondary spread by human handling (through fomites) cannot be ruled out.
Action Plan for Prevention, Control & Containment of Avian Influenza:
- Department of Animal Husbandry and Dairying (DAHD) had prepared an action plan in 2005 which was revised in 2006, 2012 , 2015 and 2021 for guidance of State Government for prevention, control and containment of Avian Influenza in India.The action plan calls for:
- Strengthening the biosecurity of poultry farms, disinfection of affected areas, proper disposal of dead birds/carcasses
- Timely collection and submission of samples for confirmation and further surveillance
- Intensification of surveillance plan as well as the general guidelines for prevention of disease spread from affected birds to poultry and humans.
- Coordination with the forest department for reporting any unusual mortality of birds was also suggested to the States.
- To keep a vigil on any unusual mortality amongst birds and to report immediately to take necessary measures.
Pune hub to track vaccine chain across 41 key cities
News: A command and control centre has been set up at Airports Authority of India Cargo Logistics and Allied Services Company Limited(AAICLAS) to monitor the movement of COVID-19 vaccines.
Facts:
Source: The Hindu
- What will AAICLAS do? It will be the nodal body for coordinating air transportation of the vaccines across a network of 41 airports with Pune — where vaccine manufacturer Serum Institute of India is located — as the hub.
- Process of Vaccine Transportation:
- The 41 airports or cities where transportation efforts will be focused include Karnal, Mumbai, Chennai and Kolkata, each of which has a Government Medical Stores Depot (GMSD) of the Central government’s Ministry of Health and Family Welfare.
- Once vaccines dispatched by the manufacturers arrive at these four big depots, they will be further distributed across 37 State depots.
- Thereafter, they will be sent to district depots and finally to the primary health care centres.
- Each of these centres has a temperature tracker which will upload temperature data on a central server for real time monitoring.
Swasth Vayu Non-invasive Ventilator receives regulator nod
News: Swasth Vayu Ventilator has received the approval of the expert committee constituted by Director General of Health Services, Ministry of Health & Family Welfare, Government of India.
Facts:
- Swasth Vayu: It is a ‘Made in India’ non-invasive (involves use of masks or similar device) ventilator developed by the National Aerospace Laboratories(NAL),Bengaluru.
- Key Features:
- It is a microcontroller based precise closed-loop adaptive control system with a built-in biocompatible 3D printed manifold and coupler with HEPA filter (Highly Efficient Particulate Air Filter).
- It also has several advanced features like Bi-level mode(BiPAP), Continuous Positive Airway Mode(CPAP) and Spontaneous modes with provision to connect Oxygen concentrator or Enrichment unit externally.
Read Also : current affairs for upsc
- Significance:
- The ventilator is ideal for treating Covid-19 patients in wards, makeshift hospitals, dispensaries and homes.
- The major advantage of this machine is also that it is simple to use without any specialized nursing, cost effective, compact and configured with majority of indigenous components.
Kerala on alert after bird flu in two districts
News: Kerala was placed on high alert after an outbreak of bird flu was confirmed in Kottayam and Alappuzha districts.
Facts:
Source: The Hindu
- Bird Flu: It refers to the disease caused by infection with avian (bird) influenza(flu) Type A viruses.These viruses occur naturally among wild aquatic birds worldwide and can infect domestic poultry and other bird and animal species.
Read more:-UPSC Syllabus 2021
- Can it infect Humans? It can occasionally infect humans as well, although human-to-human transmission is unusual.
- How does it spread to Humans? By close contact with a) Infected Poultry b) Pigs and c) Surfaces Contaminated by Infected Birds and their droppings.
- Common Symptoms of Bird Flu in Humans: Fever, Sore Throat, Cough, Muscle Aches, Difficulty in Breathing, Pneumonia, Pain in abdomen, diarrhoea among others.
National Medicinal Plants Board launches consortia of medicinal plants
News: National Medicinal Plants Board (NMPB), Ministry of AYUSH has launched a Consortia of Medicinal Plants.
Facts:
- Why was the NMPB Consortium launched? The NMPB Consortia aims to address/deliberate on the following issues: Quality planting material, Research & Development, Cultivation and Trade of medicinal plants/market linkage.
- Medicinal Plant Species Covered: In the first phase NMPB consortia is proposed for following medicinal plant species:
- Ashwagandha (Withaniasomnifera)
- Pippali(Piper longum)
- Aonla (Phyllanthus Emblica)
- Guggulu (Commiphorawightii)
- Shatavari (Asparagus racemosus).
- Seed to Shelf Approach: To establish the linkage between the farmers and manufacturers, a ‘Seed to Shelf’ approach is also being introduced. Wherein, aspects related to Quality Planting Materials(QPM), Good Agricultural Practices(GAP’s), Good Post Harvest Practices (GPHP’s) would be addressed.
Additional Facts:
- National Medicinal Plants Board(NMPB): It was established in 2000 under the Ministry of AYUSH (Ayurveda, Yoga & Naturopathy, Unani, Siddha & Homoeopathy).
- Aim: Its main objective is the development of the medicinal plants sector through developing a strong coordination between various ministries/ departments/ organizations for implementation of policies / programs on medicinal plants.
India approves two COVID-19 vaccines for emergency use
News: Central Drugs and Standards Committee(CDSCO) has approved the COVID-19 vaccines COVISHIELD and COVAXIN for restricted use in emergency situations. Initially, the 3 crore medical personnel considered at the highest risk for COVID-19, would be given the vaccine for free.
Facts:
Source: The Hindu
COVISHIELD:
- It is a vaccine developed by the Serum Institute of India based on the Oxford AstraZeneca vaccine named ChAdOx1 vaccine (also christened AZD1222) i
- Type of vaccine: It is made from a weakened version of a common cold adenovirus that causes infections in chimpanzees.
- Effectiveness: The overall efficacy of the vaccine was found to be 70.42% — well below vaccines from Pfizer and Moderna but above the 50% threshold set by many regulators.
- Dosage, protection duration and storage: The vaccine has been recommended for the approval of two full doses administered around 4-6 weeks apart. Immune response could last at least a year. The vaccine can be stored at temperatures between 2°C and 8°C.
COVAXIN:
- It has been indigenously developed by Hyderabad-based Bharat Biotech in collaboration with the Indian Council of Medical Research(ICMR).
- Type of vaccine: It is an inactivated vaccine and is made by using particles of the coronavirus that were killed making them unable to infect or replicate. Injecting particular doses of these particles serves to build immunity by helping the body create antibodies against the dead virus.
- Effectiveness: The vaccine is safe and provides a robust immune response. The vaccine is yet to complete late-stage human clinical trials in India and no efficacy rate has yet been made public.
- Dosage, protection duration and storage: The vaccine will be administered in two doses and stored at 2-8° degrees Celsius. The efficacy of the vaccine is to be determined only after 14 days post the second dose.
Approval to Covaxin, and Covishield Vaccines: Concerns and way forward
This article has been developed based on the Indian Express article “Turning point”.
Synopsis- The Drug Controller General of India (DCGI) approved two vaccines — the indigenously developed Covaxin, and Covishield. There are several concerns associated with the hasty approval of vaccines.
About Vaccines
COVISHIELD:
- This vaccine is incubated in the laboratories of Oxford University and Swedish-British pharma firm, AstraZeneca. It is manufactured by the Serum Institute of India.
- Type of vaccine: It is made from a weakened version of a common cold adenovirus that causes infections in chimpanzees.
COVAXIN:
- It has been indigenously developed by Hyderabad-based Bharat Biotech in collaboration with the Indian Council of Medical Research (ICMR).
- Approval of this vaccine has raised many concerns as the Vaccine was still undergoing phase-3 clinical trials.
As per the regulators, Phase I and Phase II clinical trials were conducted on approximately 800 subjects and the results have demonstrated that the vaccine is safe and provides a robust immune response.
An efficacy trial of this vaccine was initiated in India on 25,800 volunteers, and the data provided till now has been found to be safe, according to regulators.
However, there is no clarity about the type of data available.
Conditions associated with approval
- The emergency use approval is conditional on the vaccine developers submitting details of any adverse effect to the drug regulator, every 15 days.
- A factsheet with safety details will also be provided to those receiving the first lot of vaccines.
Accelerated approval process in India
The term “Emergency Use Authorisation (EUA)” has been used mainly by regulatory agencies like FDA in the US and some other countries.
The term Emergency Use Authorisation (EUA) has not been used anywhere in rules in India. However, 2019 rules provide for an “Accelerated Approval Process” for granting approval to a drug that is still in clinical trials. The definition of a new drug in the 2019 Rules includes a vaccine.
Conditions for Accelerated Approval Process
- There should be a prima facia case that the drug is of Therapeutic benefits.
- “Accelerated approval may also be granted to a new drug if it is intended for the treatment of a serious, or life-threatening condition, or disease of special relevance to the country, and addresses unmet medical needs,”.
- Approval can be granted even if “remarkable” effectiveness is reported even from phase-II trials.
Approval granted to drugs or vaccines that are still in clinical trials is temporary, and valid only for one year.
Read more – Emergency Use authorisation of vaccines
What are the concerns associated with the hasty approval of vaccines?
India which is regarded as a manufacturer of vaccines, has put its credibility at a stake by this hasty approval of vaccine. It has raised a wave of concerns by scientific and healthcare communities about a “public rollout of an untested product.
- First, Covaxin has been approved without clinical efficacy data. This vaccine was on the 3rd stage, which is always a key to prove its efficiency. Government’s approval to this vaccine might hurt India’s credibility in case of any adverse impacts.
- Efficacy data is an indication of how effective the vaccine is in preventing the virus attack.
- Second, As regulators have themselves evaded their rules, credibility of regulator at stake- This lack of transparency could lead to a lack of trust in the vaccine. There are several issues with the way the approval has been granted, which can lead to people losing confidence in the regulatory system.
- Third, approval an untested vaccine makes it nearly impossible to conduct a proper phase-3 trial.
- It will be unethical to expect volunteers to participate in a trial where there is only a 50% chance of being administered the actual vaccine, when they have the option of the real dose elsewhere.
- Fourth, While Pharmaceutical giants like Pfizer, Moderna, and AstraZeneca have given a go-ahead only after partial results of vaccine’s abilities in their own populations, In India Covishield has not been tested for vaccine ability among Indian population.
- As it is a possibility that vaccine response among Indian population may not be the same as among the European Population.
- Fifth, several data and reports have suggested the Vaccine hesitancy among people due to Emergency Use authorization. Approval without even base-level data will only strengthen this hesitancy among the public.
The rush to approve the COVID-19 vaccine without proper clinical trial may do more harm than good. So, it would be better to wait for the preliminary data from the phase-III trials to come in, and then grant the approval.
What is the way forward?
- Government needs to strengthen its vaccine distribution and administration mechanism to meet the need of 1/4th of the population it is looking to vaccinate in the first phase.
- Immunogenicity of both the vaccines could vary, thus there is a need to understand the adverse effects.
- Prioritising the elderly people needs to be re-examined because the elderly are less mobile and have a lower level of social interaction, they are less likely to spread the virus. So, in the long run, prioritizing the elderly people may not actually minimize the total social and economic cost inflicted by the virus.
- Surveillance and monitoring systems will require to be tweaked as per the efficiency and effectiveness data of the Vaccine.
- Vaccinators required to be educated on the finer details of the two vaccines.
Concerns of hasty approval to COVID-19 vaccine
Synopsis- Concerns regarding hasty approval granted to the COVID-19 vaccines despites the lack of adequate efficacy data.
Background-
- The Drug Controller General of India (DCGI) approved the Subject Expert Committee’s recommendation for emergency use of Serum Institute of India’s Covishieldand Bharat Biotech’s Covaxin.
- Covishieldis the same vaccine as developed by Oxford- AstraZeneca, which has got emergency use approval in the UK.
- In the case of Covaxin, concerns have been raised about the absence of efficacy data, which is generated during Phase 3 of human clinical trials.
However, experts have voiced their concerns on the approval process and the lack of publicly released efficacy data for Covaxin.
How India’s credibility as manufacturer of vaccine is at stake?
The hasty nod for Covaxin has put India’s credibility as a manufacturer of vaccines is at a stake and has raised eyebrows in the scientific and healthcare communities about a “public rollout of an untested product.
- First, Covaxinhas no clinical efficacy data- Bharat Biotch’s Covaxin vaccine is still in stage 3 clinical trials in India and the final results are yet to be released. The recommendation comes despite the lack of efficacy data for Covaxin.
- Efficacy data is an indication of how effective the vaccine is in preventing the virus attack.
- Moreover, the decision is a violation of the criteria in the draft regulatory guidelines for the development of COVID-19 vaccines published by CDSCO, in which it is clear that safety and efficacy data is required for approval of vaccine, but the indigenous vaccine from Bharat Biotech does not have efficacy details because the trials are underway.
- Second, credibility of regulator at stake-This lack of transparency could lead to a lack of trust in the vaccine. There are several issues with the way the approval has been granted, which can lead to people losing confidence in the regulatory system.
- Third, approval an untested vaccine makes it nearly impossible to conduct a proper phase-3 trial.
- It will be unethical to expect volunteers to participate in a trial where there is only a 50% chance of being administered the actual vaccine, when they have the option of the real dose elsewhere.
- Fourth, Pharmaceutical giants like Pfizer, Moderna and AstraZeneca have given a go-ahead only after partial results of vaccine’s abilities in their own populations.
- Whereas in India similar data for vaccine ability among Indian population has not been published. As it is a possibility that vaccine response among India population may not be the same as among the European Population.
The rush to approve COVID-19 vaccine without proper clinical trial may do more harm than good. So, it would be better to wait for the preliminary data from the phase-III trials to come in, and then grant the approval.
What is the way forward?
- In light of the intense concerns arising from the absence of efficacy data, the Use of Covaxinshould be treated as extended clinical trials.
- For the larger scale implementation of vaccines, Government needs to carefully monitor immune response to different vaccines and assess the efficacy across populations.
Expert panel grants emergency use authorisation for Oxford vaccine
News: The subject expert committee of Central Drugs Standard Control Organization(CDSCO) has recommended COVID-19 vaccine, Covishield for emergency use authorisation.
Facts:
- COVISHIELD: The Oxford vaccine “AZD1222” is being called Covishield in India. Serum Institute of India(SII) has entered into a manufacturing partnership with Oxford University and Pharma major AstraZeneca to produce this vaccine in India.
- Technology: Covishield is made of a weakened and modified version of adenovirus (a common cold virus) that causes infections in chimpanzees and contains the genetic material of the SARS-CoV-2 virus spike protein. After vaccination, the surface spike protein is produced, priming the immune system to attack the SARS-CoV-2 virus if it later infects the body.
- Efficacy: Researchers claimed the vaccine protected against Covid in 62% of those given two full doses and in 90% of those initially given a half dose.
- Safety: The Lancet publication, a leading medical journal has confirmed that the vaccine was well-tolerated and there were no serious safety events confirmed related to the vaccine.
- Storage: The vaccine can be stored, transported and handled at normal refrigerated conditions (2°C to 8°C) for at least six months.
Health Ministry plans communication strategy
News: Union Health Ministry has released a communication strategy to support the Covid-19 vaccine rollout in India that seeks to disseminate accurate and transparent information by alleviating apprehensions and ensuring its acceptance.
Facts:
- About the strategy: The key areas that will be addressed as part of interventions under the strategy are:
- Giving information on Covid-19 vaccines
- Addressing vaccine hesitancy
- Building vaccine eagerness along with maintaining and sustaining Covid appropriate behaviour.
Key Features of the Communication Strategy:
- Using Social Influence: The strategy focuses on using social influence or endorsements from experts and official voices to spell out the process of immunisation, emphasise on the safety and efficacy of vaccines and explain the decision to conduct the drive in a phased manner.
- National Media Rapid Response Cell(NMRRC): A Media Response Cell will be established under its ambit to ensure preparedness through media monitoring and social listening to respond in real time.It will also unfold media and public discourse through extensive monitoring of print, electronic and digital media.
- Involving Community Based Platforms: Government will involve community mobilisers and frontline workers to engage with the community at various levels to build trust and enable greater confidence in the Covid-19 vaccine.
- Adverse Effects due to immunisation: In case of any adverse effects following immunisation (AEFI), the strategy emphasises on supporting the mobilisers and health workforce in managing crisis situations by appealing to the community to stay calm while waiting for a proper diagnosis and prevent aggressive behavior against health workers.
Read Also:-CURRENT AFFAIRS 2020-2021
- About the strategy: The key areas that will be addressed as part of interventions under the strategy are:
Government launches Indian SARS-CoV-2 Genomic Consortia(INSACOG) Group
News: Government of India has launched the Indian SARS-CoV-2 Genomic Consortia Group(INSACOG).
Facts:
- INSACOG: It has been established to monitor the genomic variations in the SARS-CoV-2 on a regular basis through a multi-laboratory network.
- Composition: It comprises 10 labs (NIBMG Kolkata, ILS Bhubaneswar, NIV Pune, CCS Pune, CCMB Hyderabad, CDFD Hyderabad, InSTEM Bengaluru, NIMHANS Bengaluru, IGIB Delhi and NCDC Delhi).
- Coordinated by: The group is coordinated by the Department of Biotechnology (DBT) along with the Ministry of Health and Family Welfare(MoH&FW), ICMR and CSIR.
- Nodal Unit for Maintaining Database: National Centre for Disease Control(NCDC) will be the nodal unit for maintaining a database of all samples of the new variants of public health significance. The data will be epidemiologically analysed, interpreted, and shared with states for investigation, contact tracing and planning response strategies.
- Other key Functions of the INSACOG:
- It will establish sentinel surveillance for early detection of genomic variants with public health implications and to determine genomic variants in unusual events or trends such as super-spreader events.
- Knowledge generated through this vital research consortium will also assist in developing diagnostics and potential therapeutics and vaccines in the future.
- The group will also closely work with NCDC on activities like SOPs, data annotation, data analysis, data release among others.
More genome sequencing to study the spread of the variants
Synopsis- There is need for more genome sequencing from samples from all over the world in order to come up with effective approaches to control and prevent COVID-19 infections.
Background-
- A new variant of the pandemic SARS-CoV-2 coronavirus is spreading rapidly in Britain and prompting high levels of concern.
- Six samples of the recent U.K. returnees have been found to be positive with a variant of SARS- CoV-2 virus.
- From 25 Nov-23 Dec, about 33,000 passengers landed at various Indian airports from the U.K. So far, only 114 have been found positive and samples have been sent to 10 INSACOG (Indian SARS-CoV-2 Genomics Consortium) labs for genome sequencing.
Thus, only through detailed epidemiological studies combined with genome sequencing data can we confirm the presence and spread of the variant in India.
What are the findings related to new stain of coronavirus and will it cause concern in India?
The genomic analysis undertaken by the COVID-19 Genomics U.K. Consortium found that-
- First. The new variant of coronavirus is named “VUI 202012/01” and is defined by a set of 23 changes or mutations. Among the 23 mutations, the two of which are particularly worrisome and specifically N501Y makes is more transmissible.
- It includes a genetic mutation in the “spike” protein that can lead to an easy and immediate spread of the virus, making it deadlier. This new variant has 17 mutations that affect the shape of the virus.
- Second, It is about 70% more transmissible- The variant has the potential to increase the number of people a person can infect by over 0.4
However, it might not be able to spread wildly in India as a sizeable percentage of people are already infected.
Read more – Mutation in Coronavirus
Why it is important to undertake more genome sequencing of the virus?
The genome sequencing study would determine if the COVID patients are carrying the existing strain of SARS-CoV-2 or the mutant strain.
- First, to understand the evolving nature of the virus–So far, we are doing very less frequent genomic sequencing compared to western nations. For instance, in England, around 10 percent of the infected virus samples are sequenced to study the nature of the virus.
- Second, to find an immune escape variant of the SARS-CoV-2, [which means a mutation in the virus that allows it to evade the immune system]
- One of the immune escape variants found in genomes from India, known as N440K variant — was found to be in 2.1 percent of the gene sequences in India.
- Third, The N501Y mutation can arise independently here in India. Hence more genome sequencing and genomic epidemiology is needed.
Steps were taken by the Indian Government regarding this-
- The genomic surveillance consortium (INSACOG) has been recommended for laboratory and epidemiological surveillance of circulating strains of the SARS-CoV-2 in India.
- Under this initiative, 5 percent of the positive cases will be tested for Whole Genome Sequencing, from all the States and UT.
Read Also : Current affairs for upsc
What is the way forward?
Genome sequencing is very much important of the higher percentage of the samples to understand the evolving nature of the virus.
Mutated virus does not cause more fatalities: report
Source: The Hindu
News: According to a study by Public Health England, the new mutated variant of the novel coronavirus does not appear to cause more severe illness than other variants.
Facts:
About the Study:
- Under the study, researchers compared 1,769 people infected with the new variant with the same number of people who had different Covid variant. The two groups were matched 1:1 on the basis of age, sex, area of residence and time of testing.
- The study found that 12 of 1,340 (0.89%) people infected with the new variant died within 28 days compared with 10 of 1,360 (0.73%) people infected with virus not belonging to the new variant. Hence, the study has concluded that the difference in case fatality between the two groups is not significant.
- However, the secondary attack rate or the proportion of contacts of confirmed cases that develop disease themselves was higher in people infected with the new variant.
Additional Facts:
- What is a mutation? A mutation means an alteration in genetic material. In an RNA virus such as SARS-CoV-2, proteins are made of a sequence of amino acids. Such a virus contains some 30,000 ‘base pairs’ which are like bricks placed next to each other to form a structure. An alteration in this base can be a mutation, effectively changing the shape and behaviour of the virus.
For Further Read on New Mutant Virus: https://forumias.com/blog/mutated-covid-19-strain-of-uk-spreads-faster/
Union Health Minister nominated to the Board of GAVI, The Vaccine Alliance
Source: PIB
News: Union Health Minister of India has been nominated by the Global Alliance for Vaccines and Immunisation(GAVI) as a member of the GAVI Board.
Facts:
- Union Health Minister will be representing the South East Area Regional Office(SEARO)/ Western Pacific Regional Office (WPRO) constituency on the GAVI Board from 1st January,2021 until 31st,December 2023.
What is GAVI?
- Gavi is an international organisation – a global Vaccine Alliance created in 2000.
- It brings together public and private sectors with the shared goal of creating equal access to new and underused vaccines for children living in the world’s poorest countries.
- GAVI has observer status at the World Health Assembly.
- As part of its mission to save lives, reduce poverty and protect the world against the threat of epidemics, GAVI has helped vaccinate more than 822 million children in the world’s poorest countries preventing more than 14 million future deaths.
GAVI Board:
- The GAVI Board normally meets twice a year in June and November/ December and holds an annual retreat, normally in March or April.
- The board is responsible for strategic direction and policy-making, oversees the operations of the Vaccine Alliance and monitors programme implementation.
- With membership drawn from a range of partner organisations, as well as experts from the private sector, the Board provides a forum for balanced strategic decision making, innovation and partner collaboration.
Dry Run and Challenges of Vaccines distribution in India
Synopsis: Indian is one of the world’s leading vaccine manufacturer, thus will have better access to vaccines, but the distribution of manufactured vaccine will prove to be a formidable task.Dry run to test preparedness for the nationwide roll-out of a COVID-19 vaccine kicked off in four States — Assam, Andhra Pradesh, Gujarat and Punjab.
What is dry run of Vaccines?
- A dry run is aimed at testing the planned operations and the laid out mechanisms for Covid-19 vaccination in the state. It will provide insights into any gaps or bottlenecks so that those could be addressed before the commencement of the actual drive.
- Intended beneficiaries of each State, registered on Co-WIN’ app, have been sent text messages, containing info about the time and place of their “COVID-19 vaccination”.
Read – About Co-Win app and platform
- All the beneficiaries will have to register themselves compulsorily on Co-Win platform and provide a photo ID proof upon asking.
- Authorities will prepare a report for the STF, after conducting this dry run. STF will review the report and provide feedback and guidance to the authorities on further actions.
- The report will also be submitted to the Union Ministry of health and Family Welfare.
India’s vaccine distribution infrastructure
India has created a network of Cold Chain Infrastructure for vaccines at various levels. Presently, Vaccine distribution takes place through following process and infrastructures;
- Vaccines are produced by Manufacturers or procured by suppliers through agreements and arrangements.
- These vaccines are then delivered to 4 Government Medical Store Depots (GMSDs) in Karnal, Mumbai, Chennai and Kolkata.
- From these GMSDs vaccines are delivered to state, divisional and regional vaccine stores.
- They further distribute these vaccines to District Vaccine stores (DVCs). DVCs then deliver vaccines to PHCs, CHCs and Private facilities.
- From these centers beneficiaries can get themselves vaccinated.
All these distributions take place through insulated Vans and Vaccine carriers.
Some of the important facts and figures
- In Phase-1, Government is aiming at vaccinating 300 million most vulnerable people by August 2021 i.e. 600 million doses till August.
- At present India is having About 27000 cold chain points across the country.
- India’s present distribution capacity is 360 million doses in 8 months for both government and private facilities. It includes the Capacity of Private Cold Chain infrastructure at 200 million and government capacity at 160 million.
- The above capacity includes the infrastructure of the current immunization program, if leveraged for the covid vaccination.
- Due to the electronic vaccine intelligence network (eVIN) system, a real-time supply chain management system, India’s vaccine management has improved
What are the challenges in vaccine distribution in India?
- Firstly, to complete the aims of the first phase of the covid vaccination drive, the public sector distribution capacity will need to be expanded 2-3 times.
- Secondly, there are gaps in the vaccine distribution system. As per the Audit of health ministry in 2017-18, 26% of eVIN cold chain points reported instances of stock out during the period of assessment. More than a fifth of facilities reported wastage of vaccines.
- Third, Interstate disparity in the distribution of cold chain infrastructure across the country. For instance, roughly 4 cold chain points serve 100,000 population in Gujarat, whereas there is just one cold chain for the same number of people in Jharkhand.
- Fourth, unique requirements of the COVID-19 Pandemic such as Identifying beneficiaries, ensuring they show up on the day of vaccination, and administering a second dose after a month, provide vaccine across age groups instead of current programmes focus on particularly vulnerable sections, etc. All these require micro-level planning with a proper collaboration from the top.
- Fifth, Post-vaccination challenges such as documentation of vaccination and the tracking and investigation of vaccine safety events, all are equally important to create positive public opinion about vaccination.
- Sixth, India has performed poorly on the analysis by WHO-UNICEF in 2018, it ranked among 89 countries in 51-75 percentile range on effective vaccine management.
- Seventh, If the present infrastructure of universal immunization programme is used as planned, what will happen to the regular immunization drive, is also a big challenge in front of government.
India is one of the biggest producers of vaccines in the world. Serum Institute of India (SII) alone is a producer of more than 1.5 billion vaccine doses every year and is expected to produce 1 billion doses of the Novavax vaccine by 2021.
As now, the vaccine is being authorized by Emergency Use Authorisation method, Need is to augment the capacity of vaccine distribution on an urgent basis.
Essentiality of Dry run for COVID vaccines
Synopsis: Dry runs aimed at testing the planned operations are essential for Covid 19 vaccination process.
Background
- In the coming weeks, the Phase-3 data of two COVID-19 vaccines tested by Indian manufacturers are expected to be submitted for emergency use approval.
- A countrywide rollout to immunize the four high-risk groups will begin soon in India if any of the vaccines gets the approval.
- So, to be prepared in hand the government has rightly decided to undertake a dry run for vaccine administration. The dry run is expected to be initiated this week in four States of Andhra Pradesh, Assam, Gujarat, and Punjab.
Why the Dry run is essential?
- Though, India has been vaccinating millions of young children with a variety of vaccines each year the aspects of the COVID-19 vaccination Programme are new.
- Firstly, this is the first time a vaccine to be administered outside the universal immunisation Programme and specifically for adults belonging to specific groups.
- Second, there is a need for administering two doses of the vaccine a few weeks apart and enrolling the recipients which is different compared to our running vaccination drives.
- Third, it will allow the administrators to check the usage of the Co-WIN IT platform for management of the entire vaccination process including data entry, allocation of date and time and a drill of session sites with test beneficiaries.
- Fourth, it will also help to test the linkages between planning, implementation and reporting mechanisms.
What are the measures that needs to be ensured during Dry run exercise?
- The first task is to register the recipients of vaccine identified from the from the high-risk groups on the Co-WIN platform to avoid inclusion and exclusion errors.
- When more than one vaccine becomes available, it is essential to ensure that people receive the same vaccine twice and the exercise should confirm that the Co-WIN platform is able to generate the date and time when people can receive the second dose.
- As no COVID-19 vaccine has undergone long-term follow-up for safety during the trial it is very essential to Check and report on all adverse events after the vaccination.
- Regarding storage of vaccines, the existing facilities of the universal immunisation Programme in most districts can be used for storing the vaccines since the vaccines that are at an advanced stage of testing in India do not require ultra-low temperature for delivery and storage.
- Also, the exercise should look at creating additional storage capacity at these facilities to store millions of COVID-19 vaccines as the plan is to vaccinate 300 million people in the four high-risk groups for which it requires 600 million doses.
Examining the Strategies involved in Distributing Vaccines
Synopsis: The government must examine the principle underlying the triage scheme for optimised use of resources.
Background:
- Over the next 6-7 months, India plans to vaccinate 300 million people against COVID-19 by prioritizing healthcare workers, other front-line workers and everyone who is above 50 years of age.
- To vaccinate 300 million people, India requires 600 million doses as two doses are required per individual.
- However, government will not have problems in acquiring the required number of doses as it has already struck a deal with the Serum Institute to acquire 500 million doses of the AstraZeneca vaccine and also the availability of other vaccines such as Bharat Biotech’s Covaxin and the Russian Sputnik V are also high.
- But the strategies that they have planned for distribution of vaccines needs to be examined.
What are the Issues and dilemmas in the triage scheme?
- First, government’s strategy of prioritizing the elderly people need to be re-examined because,
- Vaccination drive should have two distinct objectives, one, providing protection to those vaccinated, and two to slow down the speed and spread of the viral transmission.
- Providing vaccination to healthcare professionals is not in conflict with the above objective because these are individuals who have high levels of exposure and they also act as active disease vectors since they interact with large numbers of people.
- But, prioritising the elderly people needs to be re-examined because the elderly is less mobile and have a lower level of social interaction, they are less likely to spread the virus. So, in the long run, prioritising the elderly people may not actually minimise the total social and economic cost inflicted by the virus.
- This suggests that densely populated areas for instance, the Dharavi slum should receive far more attention than they are likely to get under the current strategy.
- Second, the government should permit private suppliers to import and distribute the vaccine in India because,
- Currently, government’s procurement strategy relies entirely on public resources for distribution and the government plans to bear the entire cost of vaccination without involving private hospitals.
- But, allowing the private sector to provide additional supplies of the vaccine would not really be a bad policy decision if it would not decrease the availability of the vaccine to the poor.
- With more and more vaccines getting approval such as the Moderna vaccine in US, there will be a significant boost in the global supply of COVID-19 vaccines which mandates the need for involving private suppliers.
- Benefits that accrue owing to such decisions are, less waiting time for the less affluent as some of the richer individuals in the target group will opt out of the government distribution system and prefer to get vaccinated at some private outlet owing to increase in supply.
- Another potential benefit accruing to the entire population is that the larger the numbers who get vaccinated, the lower will be the speed of virus transmission amongst the non-vaccinated.
- Also, there are some cost benefits, for example, Belgian Minister has revealed that the European Union has agreed to pay for leading COVID-19 vaccines is substantially lower than the prices of Moderna and Pfizer. Given the large size of India’s market India has the bargaining power advantage
UNICEF launches the COVID-19 vaccine market dashboard
Source: UNICEF
News: As the designated COVAX procurement coordinator and procurement agent, UNICEF has launched the COVID-19 Vaccine Market Dashboard.
Facts:
- Purpose: The dashboard is an interactive tool for countries, partners and industry to follow the developments of the rapidly evolving COVID-19 vaccine market and the efforts of the COVAX Facility to ensure fair and equitable access for every country in the world.
- The dashboard will also provide a regularly updated overview of the global research and development pipeline, the projected production capacity, publicly announced bilateral and multilateral supply agreements as well as reported price points.
Additional Facts:
- COVAX: It is the vaccine pillar of the ACT-Accelerator. It is co-led by the Coalition for Epidemic Preparedness Innovation (CEPI), Gavi( the Vaccine Alliance), and the World Health Organization(WHO) – working in partnership with developed and developing country vaccine manufacturers and others.
- COVAX is the only global initiative that is working with governments and manufacturers to ensure COVID-19 vaccines are rapidly available worldwide to economies of all financial means.
- ACT Accelerator: It is a framework for collaboration. It is not a decision-making body or a new organization. It was set up in response to a call from G20 Leaders in March 2020 and launched by the WHO, European Commission, France and The Bill & Melinda Gates Foundation in April 2020.
- Goal: The goal of the ACT Accelerator is to end the COVID-19 pandemic as quickly as possible by reducing COVID-19 mortality and severe disease through the accelerated development, equitable allocation, and scaled-up delivery of vaccines.
The positive side of National Family Health Survey report
Synopsis: There has been a divergence in the actual NFHS data and the interpretations by the critics.
What are the features of National Family Health Survey report NHFS report 2019-20?
- The initial results of NFHS have been released for 2019-20 along with comparable data for the 2015-16 survey.
- Population coverage of approximately 700 million and 21 states have been covered under the NFHS data.
- Tabular data for 131 variables have been released for 2019-20.
- The data show that there has been significant improvement in many of these 131 indicators of social welfare.
Analysis provided by NFHS has been misinterpreted by the critics. Comment
It is important to compare India with the rest of the developing world. Trends in hunger, nutrition, inequality, and growth among others can be carefully evaluated in a comparative angle with the help of World Bank data provides. Some of the misinterpreted data is as follows:
- Firstly, Bangladesh underweight percentage in 2015 was stated as 22 per cent but the World Bank data states it to be 30.1 per cent, which makes it 4.7 percentage points (ppt) lower than India, not 12.8 ppt lower.
- Secondly, teenage pregnancies in India were 19.9 per cent in 2005 which reduced to 8.7 per cent in 2015 and further got 1 ppt lower in 2019. Hence, net improvement was about 12 ppt in 15 years.
- Whereas the level was 10 ppt higher constantly in the developing world during the same period. Even then some editorials claimed of worsening of teenage pregnancies in India.
- Thirdly, welfare improved between 2015 and 2019 according to a very large number of NFHS indicators. A summary of these data is as follows:
- Child Mortality: Data on three indicators (neo-natal, infant and under-five) show an improvement between 3 and 4 ppt.
- Immunizations: It improved drastically. For instance, the hepatitis B vaccine percentage (for children 12-23 months) increased from 64.8 per cent in 2015 to 83.6 per cent in 2019.
- Breast-feeding and diet of children 6-23 months: Average gain of 4 ppt for four indicators.
- Negative trend in seven young women indicators is 0: Modern birth control methods, age at marriage, teenage pregnancies, and sexual violence all show improvement. The average improvement in these seven indicators is 3.9 percentage points.
- Negative trend in 15 adult indicators is 0: Average gain is 4.1 percentage points.
- Other improvements: Some of the indicators show an increase of 9 percentage points and above in households with electricity (9.2 ppt), improved sanitation facilities (17.3 ppt), clean fuel for cooking (18 ppt) and women having a bank account that they use (29.8 ppt increase to a level of 77.2 per cent in 2019).
The points stated above show a large divergence in factual data and its interpretation. There is improvement in close to a 100 indicators and stagnation in less than 5 indicators.
What is National Family Health Survey (NFHS)?
The National Family Health Survey (NFHS) is a large-scale, multi-round survey conducted based on the representative samples collected from households throughout India.
The NFHS survey provides state and national information for India on various health parameters such as fertility, infant and child mortality, the practice of family planning, maternal and child health, reproductive health, nutrition, anaemia, utilization and quality of health and family planning services.
Who releases the National Family Health Survey?
NFHS is released by the Ministry of Health and Family Welfare (MOHFW).
But the MOHFW designated the International Institute for Population Sciences (IIPS), Mumbai, as the nodal agency. The IIPS is responsible for providing coordination and technical guidance for the survey.
Technical assistance for the NFHS was provided mainly by ORC Macro (USA) but various other organizations assist with specific issues.
Who will fund for National Family Health Survey (NFHS)?
The Survey of this size cannot be carried out with government funds alone. Many international agencies provide funds to carry out the NFHS. They are,
- United States Agency for International Development (USAID)
- The Bill and Melinda Gates Foundation
- Department for International Development (DFID)
- United Nations Children’s Fund (UNICEF)
- United Nations Population Fund (UNFPA)
- MOHFW, Government of India
What is the Goal of National Family Health Survey (NFHS)?
Every National Family Health Survey (NFHS) has two specific goals to fulfill. They are
- to provide essential data needed by the Ministry of Health and Family Welfare and other agencies for informed decision making and policy and programme intervention purposes.
- to provide insight regarding important emerging health and family welfare issues
Apart from these two specific objectives, NFHS also helps to monitor the progress of various Sustainable Development Goals (SDGs) especially SDG-3 (Good Health and Well-Being).
How many National Family Health Surveys (NFHS) conducted so far?
There are 5 rounds of National Family Health Surveys (NFHS) conducted so far in India. They are,
- First Round of NFHS conducted in 1992-93 (NFHS-1)
- Second Round of NFHS conducted in 1998-99 (NFHS-2)
- Third Round of NFHS conducted in 2005-06 (NFHS-3)
- Fourth Round of NFHS conducted in 2015-16 (NFHS-4)
- Fifth Round of NFHS conducted in 2019-20 (NFHS-5)
The NFHS-1, NFHS-2, NFHS-3 didn’t cover UTs except for Delhi because the objective of the survey then was to provide State-level estimates. (Source)
Since NFHS-4, the survey introduced district-level estimates for many important indicators and also included other UTs to provide holistic information.
5th round of National Family Health Survey (NFHS-5): (Source)
The MOHFW recently released Phase – I of NFHS-5 comprising data for 22 states/UTs. The Survey was earlier expected to release in July but due to the Covid-19 pandemic the release of the survey got delayed and it is finally released on 12th December 2020.
The fieldwork in the remaining 14 (Phase-II) States/UTs is currently in progress and expected to be available in May 2021.
The national-level indicators including most of the SDG health indicators are expected to be available by June/July 2021.
Important points regarding NFHS-5:
- The state factsheet released includes information on 131 key indicators.
- The district-level factsheet includes information on 104 key indicators.
- NFHS-5 uses the majority of NFHS-4 key indicators so that it would be comparable with NFHS-4 without any loss of information.
What is new in the 5th round of NFHS (NFHS-5)?
The NFHS-5 also included district-level estimates which were introduced during the NFHS-4. Apart from that NFHS-5 also included some new topics such as
- Preschool education,
- Disability,
- Access to a toilet facility,
- Death registration,
- Bathing practices during menstruation (menstrual hygiene),
- Methods and reasons for abortion.
- components of micro-nutrients to children,
- frequency of alcohol and tobacco use,
- additional components of non-communicable diseases (NCDs),
- expanded age ranges for measuring hypertension and diabetes among all aged 15 years and above etc.
What are the key findings of NFHS-5? (Source: The Hindu)
- Malnutrition: Of the 22 States and UTs, there is an increase in the prevalence of severe acute malnutrition in 16 States/UTs (compared to NFHS-4 conducted in 2015-16).
- The percentage of children under five who are underweight has also increased in 16 out of the 22 States/UTs.
- There is also an increase in the prevalence of other indicators such as adult malnutrition measured by those having a Body Mass Index of less than 18.5kg/m2 in many States/ UTs.
- Anaemia: Anaemia levels among children as well as adult women have increased in most of the States with a decline in anaemia among children being seen only in four States/UTs.
- Obesity: Most States/UTs also see an increase in overweight/obesity prevalence among children and adults, once again drawing attention to the inadequacy of diets in India both in terms of quality and quantity.
- Stunting: The data report an increase in childhood stunting in 13 of the 22 States/UTs compared to the data of NFHS-4.
- There was a 10-pp (Percentage Point) decline in stunting among children under five between 2005-06 (NFHS-3) and 2015-16 (NFHS-4), from 48% to 38%, averaging 1 pp a year. This was considered to be a very slow pace of improvement.
- Starvation: Volunteers of the Right to Food campaign have listed over 100 starvation deaths based on media and/or verified fact-finding reports since 2015.
- Food insecurity: Field surveys such as ‘Hunger Watch’ are already showing massive levels of food insecurity and decline in food consumption, especially among the poor and vulnerable households.
- In the Hunger Watch survey carried out in 11 States, two-thirds of the respondents reported that the nutritional quality and quantity of their diets worsened in September-October compared to before the lockdown.
- Jump in Vaccination: The survey has found considerable improvement in vaccination coverage among children aged 12-23 months across all States/UTs.
- Urban-Rural gender gaps in Internet use: There is an urban-rural gap as well as gender divide with respect to the use of the Internet. On average, less than 3 out of 10 women in rural India and 4 out of 10 women in urban India ever used the Internet.
- Increase in bank accounts operated by women: The number of bank accounts that women not only hold but also operate themselves has increased dramatically over the past five years.
PM to launch Ayushman Bharat PM-JAY SEHAT for J&K
Source: PIB
News: Prime Minister will launch Ayushman Bharat PM-JAY SEHAT to extend coverage to all the residents of the Union Territory of Jammu & Kashmir.
Facts:
- PM-JAY SEHAT: It aims to ensure Universal Health Coverage by providing free of cost insurance cover to all the residents of the UT of J&K.
- The scheme will cover the remaining population which has not been covered under the Ayushman Bharat Scheme.
Key Features of the PM-JAY SEHAT scheme:
- It provides financial cover up to Rs 5 lakh per family on a floater basis to all residents of the UT of J&K.
- It provides for operational extension of PM-JAY to 15 lakh (approx.) additional families.
- The scheme will operate on insurance mode in convergence with PM-JAY.
- The benefits of the scheme will be portable across the country. The hospitals empaneled under PM-JAY scheme shall provide services under this scheme as well.
- Significance: With the launch of ‘SEHAT’ Scheme, J&K will be among the first in the country to achieve Universal Health Coverage.
Additional Facts:
- Universal Health Coverage: It includes the full spectrum of essential, quality health services, from health promotion to prevention, treatment, rehabilitation, and palliative care and enables everyone to access the services, protecting people from the financial consequences of paying for health services out of their own pockets and reducing the risk that people will be pushed to poverty.
- Ayushman Bharat : It was launched in 2018.It is the world’s largest health insurance/ assurance scheme fully financed by the Centre.
- It provides a cover of Rs 5 lakh per family annually for secondary and tertiary care hospitalisation for public and private enlisted hospitals in the country.
- The two flagship programmes under Ayushman Bharat programme are (a) Health and Wellness Centre and (b) Pradhan Mantri Jan Arogya Yojana (PM-JAY).