ForumIAS announcing GS Foundation Program for UPSC CSE 2025-26 from 19 April. Click Here for more information.
Contents
- 1 Introduction
- 2 How is the rural healthcare structured in India?
- 3 What is the current status of rural healthcare infrastructure?
- 4 What is the need for robust rural healthcare infrastructure?
- 5 What steps have been taken by the Government to augment rural healthcare infrastructure?
- 6 What support was given during the Pandemic?
- 7 What are the factors hindering delivery of rural healthcare?
- 8 What more steps can be taken?
| For 7PM Editorial Archives click HERE → |
Introduction
Rural India is the backbone of our nation as more than 60% of India’s population resides in rural regions. The high proportion places a greater responsibility on the Government towards the health and wellbeing of the rural population. Considering this, the Government has started several schemes and is promoting numerous awareness programs to ensure health for all. There has been a special focus on rural India where the Government has pitched for providing several health facilities especially for women and children.
However the rural healthcare infrastructure has been constrained by budgetary limits, shortage of staff and other shortcomings that has made healthcare an inaccessible for many people. This warrants a more proactive approach towards the sector (rather than restricting only to reactive measures) as shown by the Government during the pandemic .
How is the rural healthcare structured in India?
The healthcare facilities in rural areas under the National Rural Health Mission (as part of the National Health Mission) have been developed as a three-tier system.
It includes Sub-Centres (SCs), Primary Health Centres (PHC) and Community Health Centres (CHC).
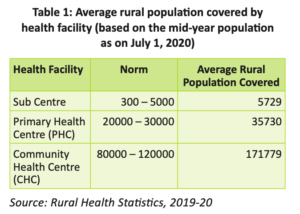
An SC being the first contact point, has one male and one female healthcare worker and a health advisor is entrusted with the task of supervising six SCs. One SC is envisaged to serve up to 5,000 people.
PHC units consist of a medical officer supported by 14 paramedical staff and are equipped with six patient beds and other basic facilities. The PHCs have been envisaged to provide an integrated curative and preventive health care with an emphasis on preventive and promotive aspects of health care. A PHC is equipped to serve up 20,000-30,000 people.
CHCs have four medical specialists (surgeon, physician, gynecologist and pediatrician) supported by 21 paramedical staff and are equipped with 30 patient beds with one Operation Theatre, X-ray, labour room and laboratory facilities. A CHC covers approximately 80,000-120,000 people.
An existing CHC (or a District Hospital, Sub-divisional Hospital) can be declared a fully operational First Referral Unit (FRU) only if it is equipped to provide round-the-clock services for emergency obstetric and New Born Care, in addition to all emergencies that any hospital is required to provide.
Source: Kurukshetra
What is the current status of rural healthcare infrastructure?
As per Rural Health Statistics 2019-20, there are 1,55,404 Rural Sub-Centres including 18,610 Ayushman Bharat Health and Wellness Centres – Sub Centres (AB-HWC-SCs).
Further, there are 24,918 Rural Primary Health Centres (PHCs) including 16,635 AB-HWC-PHCs and 5,183 Community Health Centres (CHCs).
The number of ANMs (auxiliary nurse midwife) at Sub Centres and PHCs has increased from 1,33,194 in 2005 to 2,12,593 in 2020.
Similarly, the number of allopathic doctors at PHCs has increased from 20,308 in 2005 to 28,516 in 2020, which is about 40.4% increase.
What is the need for robust rural healthcare infrastructure?
Disease Control and Prevention: Properly equipped healthcare facilities in a proximate range would ensure that common health concerns, such as viral diseases, maternal issues, child health problems etc. are addressed in an expedited manner.
Targeted Population: With more than 60% of India’s population living in rural areas, the importance of rural healthcare facilities cannot be overemphasised.
Reduce Health Expenditure: Currently the out-of-pocket expenditure in India is more than 60% which places a heavy burden on the rural poor. Robust health infrastructure will help in treating the disease at the primary level. It will save a lot of money and resources that are further spent at secondary and tertiary level health care.
Greater Vulnerability: The region comprises people who are not as affluent and resilient as their urban counterparts. Their ability to absorb extreme situations like a pandemic is very less due to inadequate financial cushions.
Economic Stability: The rural sector provides human resources for sectors such as retail, construction, manufacturing, hospitality, education and transportation.
Further, continued consumption expenditure by the rural population creates demand for multiple goods and boosts the overall economy. However none of this would be possible if individuals are not fit and healthy.
What steps have been taken by the Government to augment rural healthcare infrastructure?
Ayushman Bharat: Under this, the existing Sub-Centres (SCs) and Primary Health Centres (PHCs) are being transformed into 1.5 lakh AB-HWCs (Ayushman Bharat-Health and Wellness Centers). They would deliver 12 packages of Comprehensive Primary Health Care (CPHC) that includes preventive, promotive, curative, palliative and rehabilitative services.
Ayushman Bharat Health Infrastructure Mission: It envisages increased investments in public health and other health reforms to provide better access to health in rural areas. It has an outlay of Rs. 64,180 crore to be spent till 2025-26.
National Rural Health Mission: Under the NRHM, support is provided to the States for ensuring a range of free services related to maternal health, child health, adolescent health, family planning, universal immunization etc..
One of the key components of the Mission is to provide every village in the country with a trained female community health activist – ASHA (Accredited Social Health Activist). An ASHA acts as the interface between the community and the public health system in rural India.
Other major initiatives supported under NRHM include Janani Shishu Suraksha Karyakram (JSSK), Rashtriya Bal Swasthya Karyakram (RBSK) etc.
| Read More: Steps taken to meet the challenges of healthcare in India |
What support was given during the Pandemic?
COVID-19 Health System Preparedness and Emergency Response Package: It is aimed at containment and management of the pandemic providing for augmentation of infrastructure, oxygen supported beds, isolation beds, ICUs and Human Resources, supply of drugs, etc..
Phase 2 package amounting to Rs. 23,123 crore is under implementation from July 1, 2021 to March 31, 2022.
Support in Kind: The Ministry of Health and Family Welfare helped the states by procuring and distributing oxygen cylinders, Truenat COVID Test Cartridges, X-pert COVID cartridges, N-95 masks, PPE kits, Remdesivir and ventilators etc.
Special Oxygen Support: For making oxygen available in healthcare facilities, the government has sanctioned 1573 Pressure Swing Adsorption Oxygen generation plants, including in rural areas. Out of these, as of 20th July, 2021, 316 plants have been commissioned.
What are the factors hindering delivery of rural healthcare?
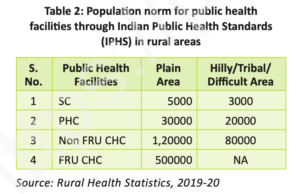
Shortage of infrastructure: The country doesn’t have the requisite number of SCs, PHCs and CHCs as per the demand. Due to the shortage, an average facility is serving much more people than it is equipped to serve.
Source: Kurukshetra Magazine
Lack of personnel: As per Rural Health Statistics 2019-20, there is a shortfall of 76.1% specialists at the CHCs as compared to the requirement for existing CHCs. Altogether, 56,581 positions of doctors and other health staff are vacant in rural areas. Further, the shortage of trained doctors has led to a proliferation of unqualified quacks.
Budgetary Constraints: India spends way too less on health in comparison to other developed nations like the U.S and Japan.The Economic Survey 2020-21 has strongly recommended an increase in public spending on healthcare services from 1% to 2.5-3%.
Awareness Deficit: The rural masses are not well aware of the facilities provided in the nearby centres. Further there lack of education inhibits outcomes of national programs as seen by development of vaccine hesitancy during the COVID-19.
Centralized Control: The centralized structure of administration and operation inhibited the degree of positive health outcomes in many rural regions during the pandemic.
What more steps can be taken?
First and foremost, the number of healthcare facilities should be enhanced. There is a need for at least two sub-centres in one village panchayat as the first point of access for patients.
Further, every two village panchayats can share one PHC and around four to six village panchayats should have one well-equipped CHC at their disposal.
Second, a permanent toll-free number can be established for healthcare whereby for every zone the CHC can be the point of operation. CHCs can have rapid response teams to address urgent concerns and requirements received over the toll-free calls.
Third, CHCs could also facilitate the creation of mobile medical units (MMUs) to facilitate health care in remote areas, especially tribal villages. MMUs can have paramedics supported by one or two nursing staff equipped with basic machinery and general medicines.
Fourth, several stakeholders within the village community like Accredited Social Health Activists (ASHA) Workers, Primary School Teachers, Religious/Spiritual Leaders etc. should be mobilized. They can help in disseminating essential information about the disease, precautions to be observed, and its cure.
Fifth, village-level resource mapping exercises can be conducted with the support of the above stakeholders. They can pass on the information to block development officers (BDOs).
BDOs would identify and monitor health issues of each gram panchayat within their jurisdiction and report it to the sub-division officers (SDOs). This would make the process more decentralized.
Sixth, states should adopt flexible norms for engaging healthcare workers for public health facilities by various mechanisms like ‘contracting in’ and ‘contracting out’ of specialist services under NHM. They can offer negotiable salaries to attract specialists including flexibility in strategies such as ‘’You quote, we pay”.
| Read More: How to fix India’s creaking health infrastructure? |
There is a need to focus on improving rural healthcare infrastructure in order to ensure that Indian citizens living even in the most remote places have access to effective healthcare. This would be in synchronization with the commitments that India possesses as a welfare state and also help in achievement of SDG 3 i.e Health for All.