ForumIAS announcing GS Foundation Program for UPSC CSE 2025-26 from 19 April. Click Here for more information.
Contents
- 1 Introduction
- 2 What are the key provisions of the Drug and Cosmetics Act, 1940?
- 3 What are the key provisions of the Drugs, Medical Devices and Cosmetics Bill, 2022?
- 4 What is the significance of the Drugs, Medical Devices and Cosmetics Bill, 2022?
- 5 What are the shortcomings of the Drugs, Medical Devices and Cosmetics Bill, 2022?
- 6 What more can be done?
- 7 Conclusion
| For 7PM Editorial Archives click HERE → |
Introduction
The Ministry of Health and Family Welfare has released a draft of the proposed Drugs, Medical Devices and Cosmetics Bill, 2022 . The Bill seeks to replace the existing Drugs and Cosmetics Act, 1940, and several sets of rules which are currently followed by the industry. It focuses on regulating medical devices as a separate entity, makes provision for fines and imprisonment for injury and death related to clinical trials or investigations, and seeks to regulate e-pharmacies. The new Bill has been drafted to keep pace with changing needs, times and technology.
What are the key provisions of the Drug and Cosmetics Act, 1940?
The Act establishes regulatory control over the import, manufacture, distribution, and sale of drugs and cosmetics in India. It makes the sale of substandard drugs a punishable offence, as these drugs are capable of bringing harm to patients.
It also established the Central Drugs Standard Control Organization (CDSCO) for discharging functions assigned under the Drugs and Cosmetics Act. The State Health department has to regulate the manufacturing, sales, and distribution of drugs. Drug Inspectors control the implementation at ground level.
Further, if the drugs are found to be substandard, then the drugs can be recalled from the market and the manufacturer has to conduct a root cause analysis for the faulted reason. The Act also has provisions to compensate the families of victims of adulteration. It calls for the penalty to be extracted from a convicted manufacturer and given to families of the victims.
When is the medicine considered substandard, adulterated, and spurious?
|
What are the key provisions of the Drugs, Medical Devices and Cosmetics Bill, 2022?
The Bill proposes new definitions for clinical trials, over-the-counter drugs, manufacturers, medical devices, new drugs, bioavailability studies, investigational new drugs and imported spurious drugs, among others e.g., diagnostic equipment, their software, implants, devices for assistance with disabilities, life support, instruments used for disinfection, and reagents come under the ambit of medical devices. The 1940 Act has medical devices as one of four categories of “drugs”.
It seeks to introduce regulation for online pharmacies and medical devices. Though there is no separate chapter on e-pharmacies, the Bill suggests that the Union government should formulate rules to regulate online pharmacies.
It proposes to empower the Drugs Control Officer with prior approval of the controlling authority to enter any premises related to clinical trials to inspect the facilities, records, data, documents, books and drugs.
It proposes stringent penalties such as imprisonment and compensation in case of injury or death during clinical trials for drugs. It lays the onus of providing medical management for any injury arising due to the trial on the investigators.
A Drugs Technical Advisory Board (DTAB) and a Medical Devices Technical Advisory Board (MDTAB) are planned to submit recommendations to the Government from time to time on policy matters.
The draft proposes to allow the Union government to waive the requirement of conducting clinical investigations for the manufacture or import of a new medical device in public interest.
What is the significance of the Drugs, Medical Devices and Cosmetics Bill, 2022?
First, it is a positive move by the Government to update an over 60-year-old law on drugs. India is third-largest pharmaceutical producer in the world. It is important that the regulatory legislation keeps pace with the changing times.
Second, a separate Medical Devices Technical Advisory Board (MDTAB) will help in catering to the specific and varied needs of the medical device sector vis-a-vis drugs.
Third, online pharmacies are currently working completely outside the law. Most of the websites have perhaps a license for a physical shop or storage unit. In case of a violation, drug inspectors are unaware of the provisions of the law or Rule under which they can proceed against the websites. Further, drug inspectors often find that the licenses these websites hold are from another state, over which they have no jurisdiction. Sometimes the websites don’t have any licenses at all, and actually use the license of the pharmacies with which they have tied-up. This makes it even more difficult to take any action.
Thus their inclusion in the new bill was a much needed step.
Fourth, the Bill prohibits clinical trials or clinical investigations of drugs and medical devices without permission from the central licensing authority. While companies have to seek permission from the regulator to conduct trials even now, this is not specifically mentioned in the existing law.
Fifth, the current clinical trial Rules have fines, but a fine of few lakh rupees is not enough to deter a big pharma company. However, the provisions for imprisonment under the draft Bill might act as a deterrent.
What are the shortcomings of the Drugs, Medical Devices and Cosmetics Bill, 2022?
First, industry’s aspirations for a separate act for medical devices has not been addressed and startups, developers and engineers will still need to grapple with a complex joint law. Further, it can become a barrier to Make in India or Innovate in India initiatives.
Second, the draft Bill completely misses post-marketing surveillance, especially for medical devices, because implants can remain within a patient’s body for years. There should also be provisions for recalling medicines or devices if any issues are detected.
Third, the draft Bill defines provisions for imprisonment or fines for ‘adulterated’ or ‘spurious’ medical devices. The draft states that a medical device will be considered to be adulterated if it is rusted, corroded, filthy, putrid, or decomposed, packed or stored in unsanitary conditions etc. However, many experts believe that these are engineering products, not homogeneous powders, tablets, or liquids that can be adulterated. Therefore, treating a rusted part of a medical device as adulterated and a criminal offence is absurd.
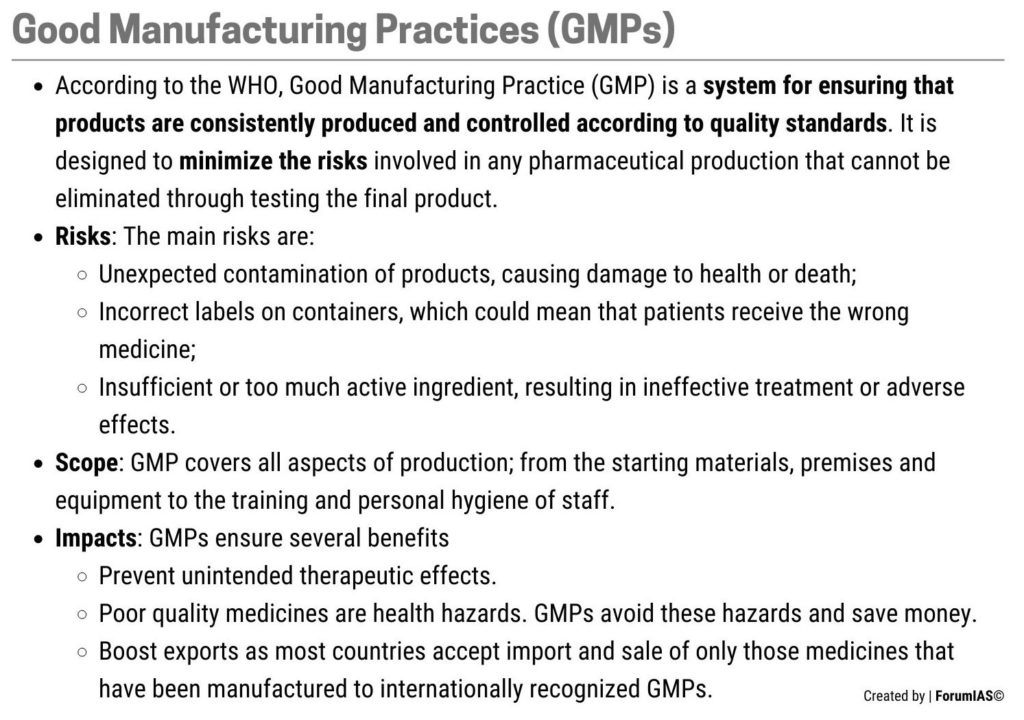
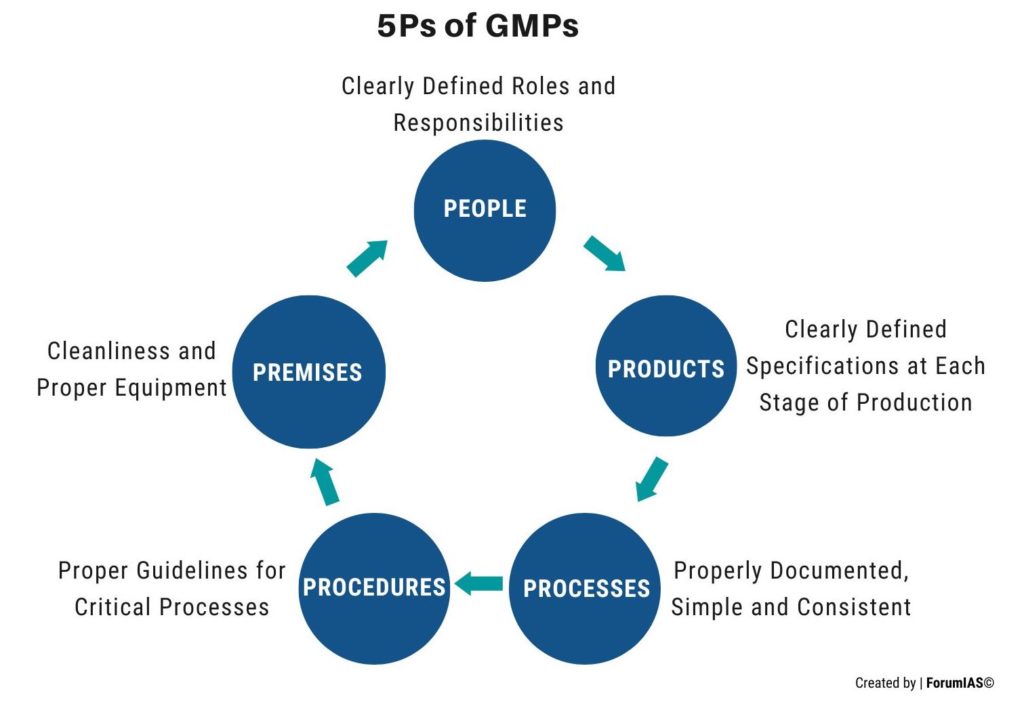
Fourth, The new Bill does not provide for the enforcement of provisions of good manufacturing practices (GMPs). GMPs are necessary to ensure quality of the pharmaceuticals. In the US, the drugs manufactured in a facility that fails to comply with GMPs is considered ‘adulterated’. The US Drug Inspectors are mandated to publish their inspection reports. In contrast, the Draft Bill envisages no criminal penalties for pharmaceutical companies failing to comply with GMPs. At most, licenses may be canceled, but since inspection reports are never published, citizens have no idea if drug inspectors are conducting GMP compliance-related inspections.
Fifth, India has 37 agencies along with the Central Drugs Standard Control Organization (CDSCO), for enforcing drug regulation across the country. The Bill does not address the need for a single regulator. Critics argue that States such as Himachal Pradesh, which account for a bulk of pharmaceutical manufacturing on account of tax benefits for the industry, do a poor job in enforcing the Drugs and Cosmetics Act. The fear of scaring away investments by the pharmaceutical industry likely plays a key role in the State’s decision to not enforce the law.
Drugs manufactured in Himachal Pradesh are sold across the country and even States with relatively more competent drug regulators can do little to stop the flood of these substandard drugs.
Sixth, the Bill is silent on this critical issue of transparency because it is structured largely on the basis of the original colonial-era legislation. It vests huge discretionary power in the hands of unelected bureaucrats with very few requirements of public disclosure.
What more can be done?
First, the Mashelkar Committee in 2003 had recommended centralizing drug licensing with the central regulator. This should be created for improving efficiency as witnessed in the U.S which has a single regulator.
Second, the Bill should have provisions for proactive disclosures related to critical documentation associated with regulatory decisions like disclosure of data related to new drug approval (including clinical trial data), GMP compliance data etc.
Third, Public hearings or citizen’s petitions should be allowed to enable citizens to participate in the regulatory process and register their objections. For example, every drug approval process should be accompanied by a public hearing to allow doctors and ordinary citizens to question regulators and explain their rationale for approving the new drug.
Conclusion
The Drugs, Medical Devices and Cosmetics Bill has some promising provisions but also leaves critical gaps that must be addressed. The Government must address these gaps to make the law more holistic and inclusive in nature. A robust regulatory arrangement will further enhance the global standing of India’s pharmaceutical industry.
Syllabus: Government policies and interventions for development in various sectors and issues arising out of their design and implementation, Issues relating to development and management of Social Sector/Services relating to Health
Source: The Hindu, Indian Express, Indian Express