ForumIAS announcing GS Foundation Program for UPSC CSE 2025-26 from 19 April. Click Here for more information.
Contents
| For 7PM Editorial Archives click HERE → |
Introduction
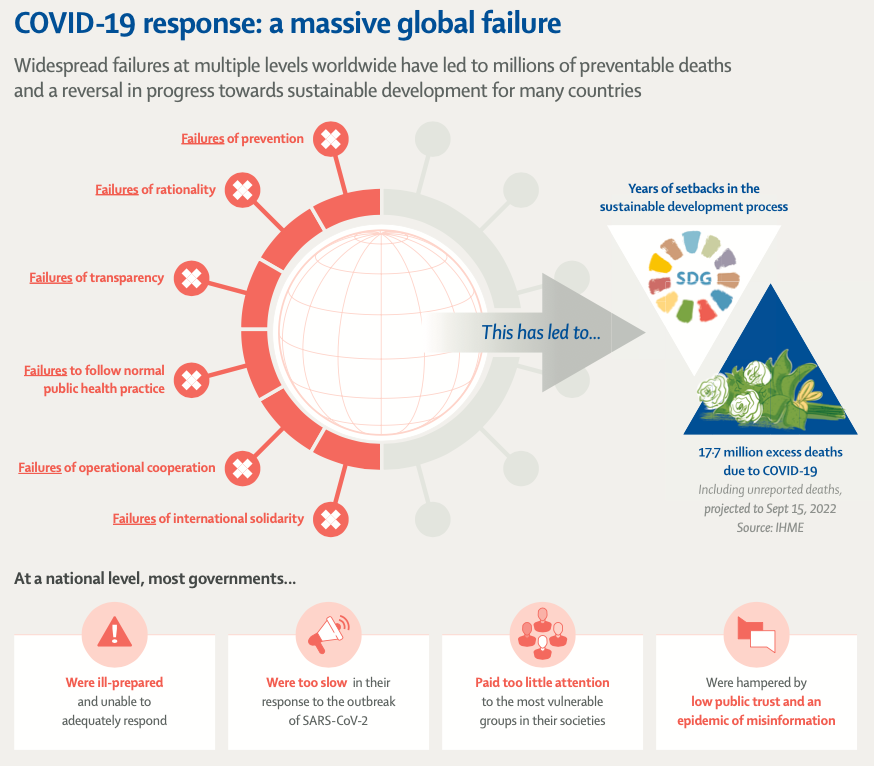
According to the Institute for Health Metrics and Evaluation (University of Washington, US), there have been 6·9 million ‘reported deaths’ and 17·2 million ‘estimated deaths’ from COVID-19, as of May 2022. The Lancet Commission Report on COVID-19 Pandemic has examined the global response to the pandemic in the two years since 2020. The Report has cited widespread failures in prevention, transparency, rationality, basic public health practise, operational cooperation, and international solidarity that resulted in an estimated 17.2 million deaths. The report also finds that most national governments were unprepared and were slow to respond. They paid insufficient attention to their societies’ most vulnerable groups, and were hampered by a lack of international cooperation and an epidemic of misinformation.
What are the Key Findings of the Lancet Commission Report on COVID-19?
Origin of the Pandemic: The report notes that there are two leading hypothesis regarding origin of SARS-CoV-2. (a) The virus emerged as a zoonotic spillover from wildlife/farm animal, possibly through a wet market whose location is still undetermined; (b) The virus emerged from a research related incident, during the field collection of viruses or through a laboratory-associated escape.
Both hypothesis require further scientific investigation. Identification of the origin of the virus will help to prevent future pandemics and strengthen public trust in science and public.
Slow Initial Response of the WHO: The WHO acted too cautiously and too slowly on several important matters. The include: (a) Warn about the human transmissibility of the virus; (b) Declare a Public Health Emergency of International Concern (PHEIC); (c) Support international travel protocols designed to slow the spread of the virus; (d) Endorse the public use of face masks as protective gear; (e) Recognise the airborne transmission of the virus.
Slow response of the Governments: The outbreak became known globally in early January 2020. However, most governments around the world were too slow to acknowledge or act with urgency in response.
Poor Coordination among Governments: Coordination among governments was inadequate on policies to contain the pandemic, including; (a) Travel protocols to slow the global transmission of the virus; (b) Testing strategies; (c) Public health and social measures; (d) Commodity supply chains; (e) Data standards and reporting systems; (f) Advice to the public.
Public Opposition: Epidemic control was hindered by substantial public opposition to routine public health and social measures, such as the wearing of properly fitting face masks and getting vaccinated. This opposition reflects: (a) A lack of social trust; (b) Low confidence in government advice; (c) Inconsistency of government advice; (d) Low health literacy; (e) Lack of sufficient behavioural-change interventions; (f) Extensive misinformation and disinformation campaigns on social media.
Absence of Behavioural Aspects in Public Policies: Public policies have also failed to draw upon the behavioural and social sciences. Doing so would have led to more successful implementation of public health interventions and helped to increase social trust, pro-sociality and equity. In many cases, policies and decision making have not been informed by robust and continuously updated evidence syntheses.
Inability to address Inequalities: Public policies did not adequately address the pandemic’s profoundly unequal effects.
Heavily burdened groups include: (a) Essential workers (disproportionately concentrated in more vulnerable minority and low-income communities); (b) Children and Women who face employment, safety, and income losses, exacerbated by the adverse consequences of school closures; (c) People living in congregate settings, such as prisons or care homes, especially for older populations; (d) People living with chronic conditions and disability; (e) Migrants, refugees, and displaced populations; (f) People without access to quality and affordable health care.
Countries with Resilient Healthcare Systems fared better: High-income countries that have a strong and resilient national health system have generally fared better at addressing COVID-19 and maintaining non-pandemic-related health services.
Benefit of Community Healthcare and Prior Experience: In low- and middle-income countries (LMICs), health systems tend to be under-resourced and fragmented. Better outcomes were seen when previous experiences with outbreaks/epidemics were built upon, and when community-based resources (like community health workers) were used to support screening and contact tracing capacity and trust-building within communities.
Inequitable Access to Vaccines: Rapid vaccine development indicates success of robust R&D system and is the result of long-standing public and private investment and cooperation. However, the lack of a multilateral and coordinated approach by governments to manage intellectual property rights, technology transfer, international financing, the allocation of vaccines from multinational pharmaceutical companies, and the support for vaccine production in LMICs for use in those countries, has come at a great cost in terms of inequitable access to vaccines.
Economic Recovery: Economic recovery depends on sustaining high rates of vaccination coverage and low rates of new infections. It is also dependent on fiscal and monetary policies to mitigate the socioeconomic effects of the pandemic and prevent a financial crisis. Emergency global financing from the International Monetary Fund, the World Bank, and regional development banks had a positive impact, although much larger financial flows from high-income to low-income regions were needed.
Impact on Sustainable Development: The sustainable development process has been set back by several years, with a deep under financing of investments needed to achieve the Sustainable Development Goals (SDGs) and the aims of the Paris Climate Agreement. In most countries, the pandemic diverted resources and policy attention away from longer-term goals, thereby reversing progress towards the SDGs in many countries.
Source: The Lancet
What are the Key Recommendations of the Lancet Commission Report on COVID-19?
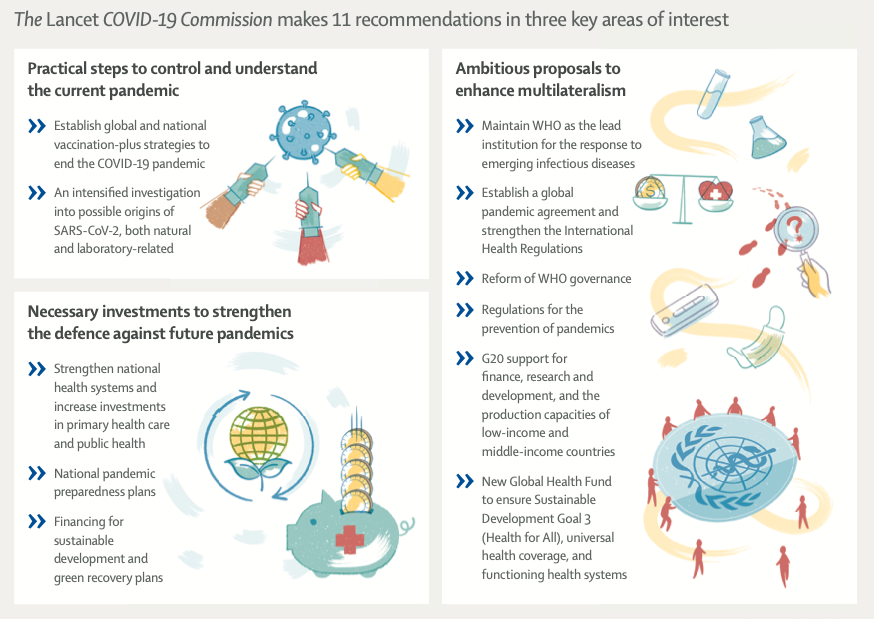
Globally Coordinated Efforts: There is a need for globally coordinated efforts to bring an end to the COVID-19 pandemic on a rapid and equitable basis. Countries should maintain a vaccination-plus strategy that combines: (a) Mass vaccination; (b) Availability and affordability of testing; (c) Treatment for new infections and long COVID (test and treat); (d) Complementary public health and social measures (including the wearing of face masks in some contexts); (e) Promotion of safe workplaces; (f) Economic and social support for self-isolation. A vaccination-plus strategy with the goal of protecting populations should be implemented on a sustainable basis, rather than as a reactive policy that is abruptly turned on and off.
Trace the Origin: The WHO, Governments, and the scientific community should intensify the search for the origins of SARS-CoV-2, investigating both a possible zoonotic origin and a possible research-associated origin. The search for origins requires unbiased, independent, transparent, and rigorous work by international teams in virology, epidemiology, bioinformatics, and other related fields.
Expand the WHO Science Council: The WHO should expand the WHO Science Council to apply urgent scientific evidence for global health priorities, including future emerging infectious diseases. This Council should include experts from diverse fields and should include younger people and have gender parity. Establishing an understanding of exposure routes and the highest-risk environments for transmission should always be among the first essential steps for scientists in response to future disease threats. This knowledge should determine effective control strategies for reducing risk.
WHO Science Council The Science Council was established in April 2021 by the Director General of the World Health Organization to provide guidance on the science and research strategy of the organization. It directly advises the Director-General about high-priority scientific issues. It is aimed at identifying current and new science and technology issues that WHO needs to address, including global health threats, and new advances with a potential for direct or indirect impact on global health. |
Stronger Means of Coordination: The Governments, represented at the World Health Assembly (WHA) by their national health ministers, should establish stronger means of cooperation and coordination in the response to emerging infectious diseases. Strengthened cooperation should be incorporated in a new pandemic agreement and in updated International Health Regulations (IHR), as were adopted in 2005 after the outbreak of SARS and which now need updating.
| Read More: Need for a Global Pandemic Treaty – Explained, pointwise |
Strengthen the WHO: The WHA should create a WHO Global Health Board with representation from all regions. Reforms of WHO should include a substantial increase of its core budget. The world community should not establish new centres of global health policy and finance that would compete with or undermine, the central role of WHO.
Preventing future infectious diseases: The Lancet Commission Report on COVID-19 recommends a dual track to prevent future emerging infectious diseases.
To prevent natural spillovers, governments should coordinate on the global surveillance. There is also need to regulate trade of domestic and wild animals and take stronger measures against dangerous practices.
To prevent research-related spillovers, WHO should be given new oversight authority regarding the biosafety, biosecurity, and bio-risk management of national and international research programmes that are engaged in the collection, testing, and genetic manipulation of potentially dangerous pathogens.
Bolster R&D and Production Capacities: The WHA, in conjunction with the G20 countries, should adopt a 10-year global strategy to bolster research and development capacity and commodity production capacity (including for vaccines), including in the low-income regions. WHO should help several low-income and middle-income countries (LMICs) to achieve WHO’s stringent regulatory authority status.
Strengthen National Health Systems: Countries should strengthen national health systems on the foundations of public health and universal health coverage. The systems should be grounded in human rights and gender equality. Strong public health systems should include: (a) Strong relationships with local communities and community organisations; (b) Surveillance and reporting systems; (c) Robust medical supply chains; (d) Health-promoting building design and operation strategies; (e) Investments in research in behavioural and social sciences to develop and implement more effective interventions; (f) Promotion of prosocial behaviours; (g) Strong health education for health promotion, disease prevention, and emergency preparedness; (h) Effective health communication strategies; (i) Active efforts to address public health disinformation on social media.
National Pandemic Preparedness Plans: Each country should determine and expand national pandemic preparedness plans to prevent and respond to newly emerging infectious diseases. Preparedness plans should include (a) Improved surveillance and monitoring; (b) Definition and protection of vulnerable groups; (c) International notifications; (d) Cooperation within WHO regional groups; (e) Emergency financing; (f) Guidelines on behavioural, social, and environmental interventions, travel protocols, and safe schools and workplaces; (g) Robust health-commodity supply chains (e.g., personal protective equipment, diagnostics, therapeutics, and vaccines); (h) Effective risk communication and active opposition to misinformation and disinformation; (i) Training of public health professionals; (j) Provision of adequate staffing.
Global Health Fund: A new Global Health Fund should be created. This Fund should combine and expand the operations of several existing health funds and add new funding for 3 windows of financing: (a) Commodities for disease control; (b) Pandemic preparedness and response; (c) Primary health system strengthening in LMICs. The Fund should have decentralised programme design and implementation to reflect regional needs and priorities rather than being under top-down control from a few donor countries.
Scale-up Financing for LMICs: The UN member states, (particularly G20 countries), should adopt a new financial architecture to scale up financing for LMICs to meet the urgent challenges of pandemic preparedness, the Paris Climate Agreement, and the Sustainable Development Goals. The new financial architecture should include increased sustainable development funding from all sectors: official institutions, the private sector, foundations, and civil society.
Source: The Lancet
What are the 5 Pillars to fight emerging infectious diseases suggested by the Lancet Commission Report on COVID-19?
Prevention: To stop an outbreak before it occurs by taking effective measures to prevent the emergence of a new and dangerous pathogen.
Containment: To eliminate the transmission of disease from infected individuals to susceptible individuals after a disease has emerged.
Health services: To save the lives of people with the disease and ensure the continuity of other health services, including those for mental health.
Equity: To ensure that economic and social burdens are shared among the population and that the most vulnerable groups and individuals are protected.
Global innovation and Diffusion: To develop, produce, and distribute new therapeutics and vaccines in an equitable and efficient manner.
Conclusion
The Lancet Commission Report on COVID-19 Pandemic has provided some key insights about the failures at the global level, that led to massive loss of lives and social disruption. The Report has provided valuable recommendations to combat future pandemics and calls for strengthened multilateralism centred on a reformed and strengthened World Health Organization (WHO). It has also recommended scaling-up investments, refined planning for national pandemic preparedness and health system strengthening with special attention to vulnerable populations. Strong action on these recommendations through a coordinated global effort can prepare the world for a much better response to any future pandemic.
Syllabus: GS II, Issues relating to development management of Social Sector/Services relating to Health, Education, Human Resources; GS II, Effect of policies and politics of developed and developing countries on India’s interests; GS III, Disaster and Disaster Management.
Source: Indian Express, The Hindu, The Lancet