ForumIAS announcing GS Foundation Program for UPSC CSE 2025-26 from 19 April. Click Here for more information.
Contents
What is the news?
In a move to encourage private hospitals to take part in Ayushman Bharat-Jan Arogya Yojana (JAY), the government is planning to rationalise the rates of health benefits packages under the scheme and also resolve issues with payments.
About the scheme:
Ayushman Bharat-Jan Arogya Yojana (JAY)
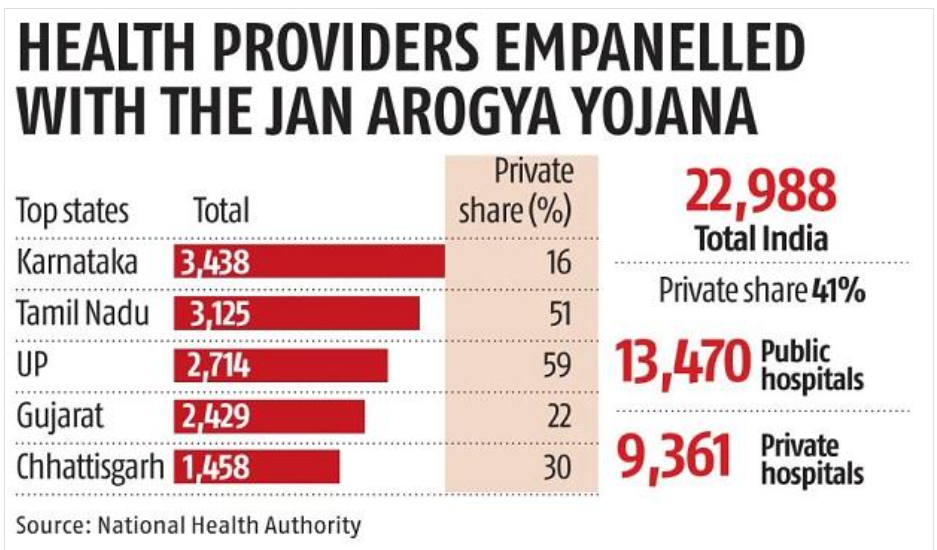
The scheme was launched by the Prime Minister in 2018. So far, 23,000 hospitals have been empanelled under the scheme, 40 percent of which are from the private sector.
The government has so far issued 160 million Ayushman cards and plans to issue another 100 million during 2020-21.
What are the issues in the scheme:
Private hospitals have raised concerns with the health ministry that the rates of treatment under the health scheme are not viable and becoming a hindrance for their participation in the initiative.
About the Government move:
- The health authority plans to set up standardised rates and treatment protocols across hospitals so that the total spent by the exchequer can also be ascertained easily.
- The health authority will also start joint review missions, headed by a retired government official, to increase monitoring and evaluation of the scheme.
- In order to resolve payment issues and enable faster disposal of claims, the government is considering setting up a green channel for hospitals with a clean track record.
- The government is also planning to set up beneficiary facilitation agencies in empanelled public hospitals to increase the uptake.
Benefits of the move:
All these moves will make Fifty percent of the claims of hospitals can be cleared immediately. Further, It will encourage them to ensure proper billing as well.




