ForumIAS announcing GS Foundation Program for UPSC CSE 2025-26 from 19 April. Click Here for more information.
Contents
| For 7PM Editorial Archives click HERE → |
Introduction
Mental disorders are now among the top leading causes of health burden worldwide, with no evidence of global reduction since 1990. Suicides rates in India are amongst the highest when compared to other countries at the same socio-economic level. The latest survey by India’s National Institute of Mental Health and Neurosciences (NIMHANS) found that nearly 150 million Indians are in need of mental healthcare services, but fewer than 30 million are seeking care. This shows several issues with mental healthcare in India including access and social attitude to mental health. The Government has taken several initiatives to improve access to mental healthcare services in addition to gradually changing the discourse on mental health. However, as evident in the data, there is a need for further effort to address the issues.
What is the status of Mental Health in India?
The WHO defines Mental Health as, “Mental health is a state of mental well-being that enables people to cope with the stresses of life, realize their abilities, learn well and work well, and contribute to their community. It is an integral component of health and well-being that underpins our individual and collective abilities to make decisions, build relationships and shape the world we live in“.
The WHO calls Mental health as a basic human right. And it is crucial to personal, community and socio-economic development.
According to the WHO, mental illness makes about 15% of the total disease conditions around the world. In 2019, India’s suicide rate was at 12.9 per 1,00,000 persons. This was higher than the regional average of 10.2 and the global average of 9.0. Suicide has become the leading cause of death among those aged 15–29 in India.
In 2017, an estimation of the burden of mental health conditions for the States across India revealed that as many as 197.3 million people (~14% of the population) required care for mental health conditions. This included around 45.7 million people with depressive disorders and 44.9 million people with anxiety disorders.
According to the National Mental Health Survey conducted by NIMHANS in 12 States, the prevalence of mental morbidity is high in urban metropolitan areas. Nearly 1 in 20 persons suffer from depression. 0.9 % of the surveyed population were at high risk of suicide.
According to the NCRB data, 1,64,033 people committed suicide in 2021, a 6.2% rise in comparison to 2020.
What are the harmful effects of poor Mental Health?
Impact on Physical Health: A study found that positive psychological well-being can reduce the risks of heart attack and stroke. On the other hand, poor mental status can lead to poor physical health or harmful behaviour. Depression has been linked to many chronic illnesses. These illnesses include diabetes, asthma, cancer, cardiovascular disease, and arthritis.
Impact on Relationships: Mental-health conditions during adolescence and young adulthood can have a significantly negative impact on the development of safe and healthy relationships with peers, parents, teachers, colleagues and partners.
Impact on Productivity: It impacts a person’s ability to concentrate and engage in productive activities.
The WHO Report on Mental Health and Development (2010) highlighted the risks of a cyclical relationship between vulnerability and poor mental health, in which people with such conditions are a vulnerable group subject to stigma, discrimination, violence, marginalization and other violations of their human rights.
What are the reasons for poor status of Mental Health in India?
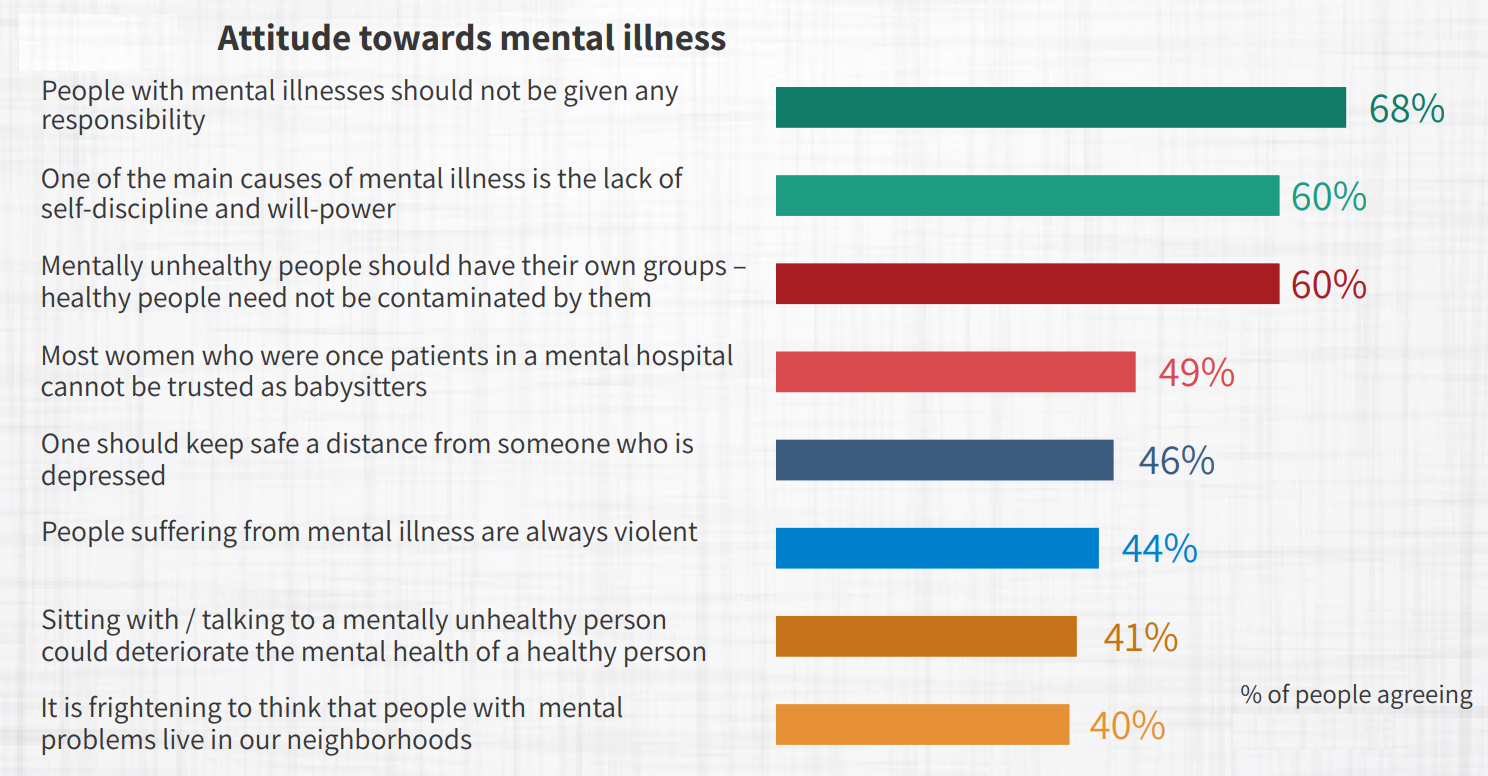
Lack of Awareness and Sensitivity: In India, mental health issues are not considered as healthcare issues. Any person suffering from mental issues is considered weak. Stigma and discrimination often undermine social support structures. Persons suffering from such issues are often tagged as ‘lunatics’ by the society. This leads to a vicious cycle of shame, suffering and isolation of the patients.
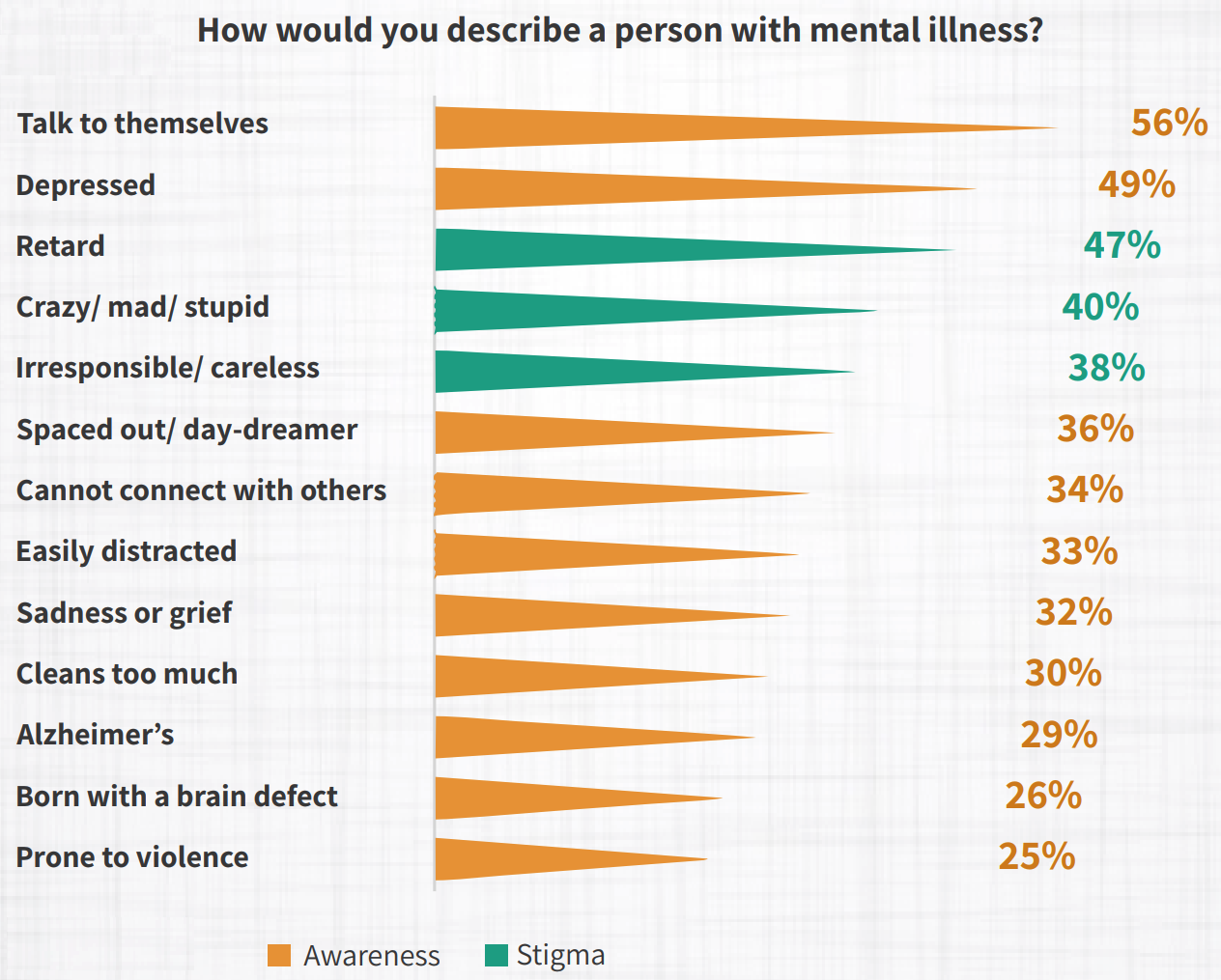
A survey conducted in 2018 showed that while 87% of the respondents showed some awareness of mental illness, 71% also used terms associated with stigma.
Lack of Mental Healthcare Personnel: There is a severe shortage of mental healthcare workforce in India. According to the WHO, in 2011, there were 0.301 psychiatrists and 0.047 psychologists for every 100,000 patients suffering from a mental health disorder in India. In contrast, the ratio in most developed countries is in excess of 10.
Gap in Treatment: At present, only 20-30% of people with mental illnesses receive adequate treatment. One major reason for such a wide treatment gap is the problem of inadequate resources.
Low budget Allocation: Developed countries allocate 5-18% of their annual healthcare budget on mental healthcare, while India allocates roughly 0.05% (Organization for Economic Co-operation and Development, 2014) of its healthcare budget. This is the lowest among all G20 countries. Despite a rise in mental illness issues, the Union Ministry of Health allocated less than 1% of its budget to directly deal with psychological illnesses in 2022.
Changed Lifestyle: Increased use of certain kinds of social media is exacerbating stress and mental illness, especially among the young people. Social media detracts from face-to-face relationships, which are healthier, and reduces investment in meaningful activities. More importantly, it erodes self-esteem through unfavourable social comparison. In addition, some experts contend that the shift to nuclear families has reduced the avenues of relieving one’s anxieties as family members are not emotionally available at most crucial times.
Income Inequalities: Mental issues are closely linked with poverty. People living in poverty are at greater risk of experiencing mental health conditions. On the other hand, people experiencing severe mental health conditions are more likely to fall into poverty through loss of employment and increased health expenditure.
What steps have been taken to improve Mental Health in India?
Legal Measures
The Mental Healthcare Act, 2017: The Act makes several provisions to improve the state of mental health in India. The Act rescinds the Mental Healthcare Act, 1987 which was criticised for failing to recognise the rights and agency of those with mental illness. The Act seeks to ensure rights of the person with mental illness to receive care and to live a life with dignity. It provides the Right to Access to Healthcare: Every person shall have a right to access mental health care and treatment from mental health services run or funded by the appropriate Government. It also empowers person with mental illness to make an advance directive that states how he/she wants to be treated for the illness.
The Act decriminalised suicide stating that whoever attempts suicide will be presumed to be under severe stress, and shall not be punished for it.
Rights of Persons with Disabilities Act, 2017: The Act acknowledges mental illness as a disability and seeks to enhance the Rights and Entitlements of the Disabled and provide an effective mechanism for ensuring their empowerment and inclusion in society.
Schemes and Initiatives
National Mental Health Programme (NMHP): Keeping with the WHO’s recommendations, the programme was introduced in 1982 to provide mental health services as part of the general healthcare system. The District Mental Health Programme (DMHP) component of the NMHP has been sanctioned for implementation in 704 districts for which support is provided to States/UTs through the National Health Mission.
Facilities made available under DMHP at the Community Health Centre (CHC) and Primary Health Centre (PHC) levels, include outpatient services, assessment, counselling/ psycho-social interventions, continuing care and support to persons with severe mental disorders, drugs, outreach services, ambulance services etc. In addition to above services there is a provision of 10 bedded in-patient facility at the District level.
Generating Awareness: To generate awareness among masses about mental illnesses Information, Education and Communication (IEC) activities are an integral part of the NMHP. At the District level, sufficient funds are provided to each District under the DMHP (under the Non-communicable Diseases flexi-pool of National Health Mission) for IEC and awareness generation activities in the community, schools, workplaces, with community involvement.
Under the DMHP various IEC activities such as awareness messages in local newspapers and radio, street plays, wall paintings are undertaken by the States/UTs.
National Tele Mental Health Programme: The Government has announced a National Tele Mental Health Programme in the Budget of 2022-23, to further improve access to quality mental health counselling and care services in the country.
Kiran: A 24/7 toll-free helpline called Kiran was established by the Ministry of Social Justice and Empowerment in 2020 to offer support to those dealing with anxiety, stress, depression, suicide thoughts, and other mental issues.
Manodarpan: Students will receive psychosocial help as part of an effort under the Atmanirbhar Bharat Abhiyan, with the goal of improving the students’ mental health and overall well-being. Its components include Advisory Guidelines for students, teachers and faculty of School systems and Universities along with families; National level database and directory of counsellors; Toll-free helpline; Handbook on Psychosocial Support etc.
Issuance of Guidelines/Advisories: Guidelines/ advisories on management of mental illness have been issued by the Government. All the guidelines, advisories and advocacy material can be accessed on the website of the Union Ministry of Health and Family Welfare under ‘Behavioural Health – Psychosocial Helpline’.
What steps can be taken further?
There is a need of an urgent and well-resourced ‘whole-of-society’ approach to protect, promote and care for the mental health of people. This should be based on the following pillars.
First, there is a need to address the deep stigma surrounding such issues which prevents patients from seeking timely treatment and makes them feel shameful, isolated and weak.
Second, mental health should be made an integral part of the public health programme to reduce stress, promote a healthy lifestyle, screen and identify high-risk groups and strengthen interventions like counselling services. Special emphasis should be given to schools. In addition, special focus should be on groups that are highly vulnerable to mental health issues such as victims of domestic or sexual violence, unemployed youth, marginal farmers, armed forces personnel and personnel working under difficult conditions.
Third, Infrastructure should be improved for mental health care and treatment. Innovative models are required to deepen the penetration of services and staff. ASHAs can be trained for this purpose. Community health workers (ASHAs) can not only educate and sensitize women and children about mental diseases but also guide them to reach the right expert in their locality.
Fourth, The above interventions will require enhanced allocation to mental healthcare in the Budget. Substantial investment will be needed to address the wide treatment gap in the health infrastructure and human resources.
Fifth, Careful mapping and research needs to be undertaken to produce quality data, that is essential to understand the size of the problem. This in turn should be utilised to implement a comprehensive approach, supported by heightened political commitment, scientific understanding and a citizen driven movement.
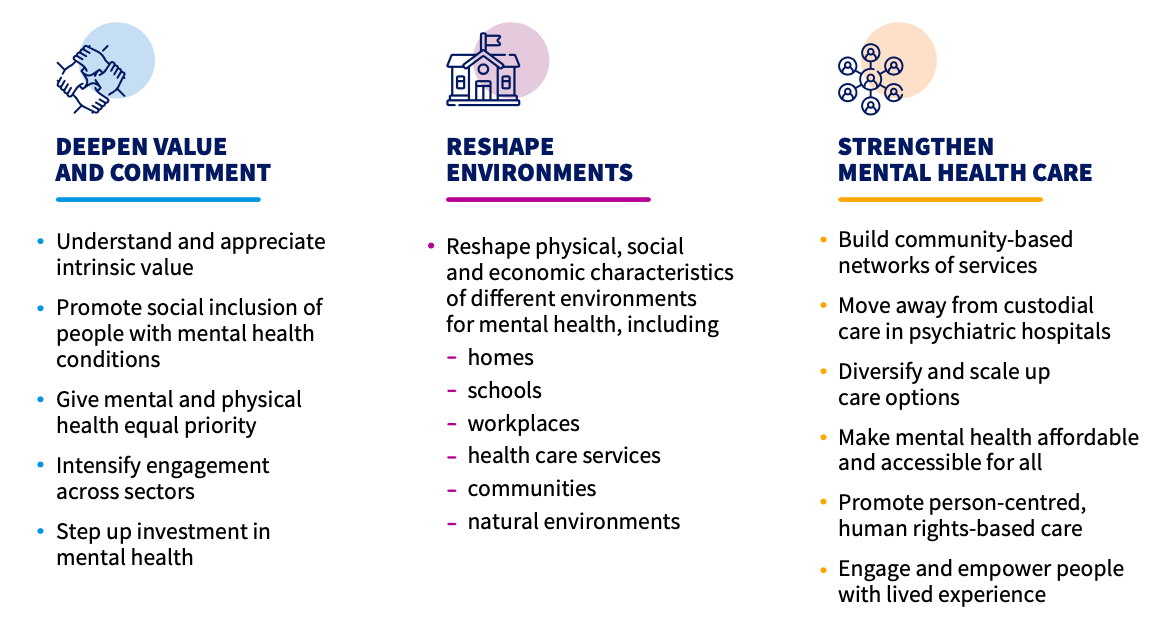
Sixth, the WHO has recommended Three Paths to transformation towards better Mental Health.
Source: WHO
Conclusion
The status with respect to mental issues has worsened since COVID-19 pandemic. The mental healthcare system in India is under-equipped to deal with the crisis. Urgent interventions, in terms of enhanced budget, increased workforce, and improved awareness are necessary to address the challenge.
Syllabus: GS II, Issues relating to development and management of Social Sector/Services relating to Health.
Source: Indian Express, Indian Express, Economic Times, PIB