ForumIAS announcing GS Foundation Program for UPSC CSE 2025-26 from 19 April. Click Here for more information.
ForumIAS Answer Writing Focus Group (AWFG) for Mains 2024 commencing from 24th June 2024. The Entrance Test for the program will be held on 28th April 2024 at 9 AM. To know more about the program visit: https://forumias.com/blog/awfg2024
Contents
- 1 Introduction
- 2 What is the Mosquirix vaccine?
- 3 What other vaccines are in the development phase?
- 4 What is Malaria?
- 5 Why it took so long to develop the Malaria vaccine?
- 6 What is the impact of Malaria on the global level and India?
- 7 What are the global and national initiatives to curb Malaria?
- 8 What are the challenges in eliminating Malaria from India?
- 9 How India can reduce the Malaria burden?
| For 7PM Editorial Archives click HERE → |
Introduction
The new vaccine “RTS,S/ASO1 (RTS.S)” with its trade name “Mosquirix” was endorsed by the World Health Organisation (WHO) recently. This is the first and only Malaria vaccine to have shown the capability of significantly reducing malaria, and life-threatening severe malaria, in tests done on young African children.
WHO’s recommendation is based on the advice of two of its global advisory bodies, one for immunization and the other for malaria. The decision is significant as the strategic delivery of the vaccine just prior to the high malaria transmission season can optimize impact and markedly reduce mortality, especially when combined with other recommended malaria control interventions.
What is the Mosquirix vaccine?
It has been developed by the British pharmaceutical company GlaxoSmithKline in partnership with the PATH Malaria Vaccine Initiative.
The vaccine acts against P. falciparum, the most deadly malaria parasite globally, and the most prevalent in Africa. It targets a protein called circumsporozoite in Plasmodium falciparum. It is a recombinant protein vaccine, which includes DNA from more than one source.
The vaccine is formulated with an adjuvant called AS01. It is designed to prevent the parasite from infecting the liver, where it can mature, multiply, and infect red blood cells, which can lead to disease symptoms.
The malaria vaccine should be provided in a schedule of 4 doses in children from 5 months of age for the reduction of malaria disease and burden.
More than 800,000 children in Ghana, Kenya, and Malawi have been vaccinated, and are benefiting from the vaccine as part of a pilot program.
However, it offers no protection against P vivax malaria, which is prevalent in many countries outside Africa.
What other vaccines are in the development phase?
R21/Matrix M is in the trial phase. It is a modified version of Mosquirix and has been developed by researchers at the University of Oxford. It is expected that this vaccine will be the first to reach WHO’s goal of at least 75% efficacy.
What is Malaria?It is caused by the bite of the female Anopheles mosquito (vector) if the mosquito itself is infected with a malarial parasite. There are five kinds of malarial parasites — Plasmodium falciparum, Plasmodium vivax (the commonest one), Plasmodium malariae, Plasmodium ovale, and Plasmodium knowlesi. Click here to know more about the malarial parasites After entering the human body, parasites initially multiply within the liver cells and then attack the Red Blood Cells (RBCs) resulting in their rupture. Symptoms of malaria include fever and flu-like illness, including shaking chills, headache, muscle aches, and tiredness. But, it is preventable and curable. |
Why it took so long to develop the Malaria vaccine?
The complexity of the malaria-causing parasites’ life cycle: This cycle includes mosquitoes, human liver, and human blood stages, and subsequent antigenic variations of the parasite. According to research, these parasites are able to hide inside human cells to avoid being recognized by the immune system.
Challenges with Models and reality: The most common mouse models of malaria employ rodent-specific parasite species. The immune response patterns observed in these models are not fully transferable to humans.
Lack of Funding: Malaria affects mostly low and middle-income countries, which lack infrastructure and finance. Vaccine manufacturers have very little incentive for malaria vaccines and continued targeting vaccines for industrialized world markets. Even it did not receive the same kind of attention as other diseases as HIV/AIDS.
What is the impact of Malaria on the global level and India?
Global disease burden
According to WHO, it claims over 4 lakh lives every year. Children aged under five years accounted for 67% of all malaria deaths globally. It is most endemic in Africa, with Nigeria, Congo, Tanzania, Mozambique, Niger and Burkina Faso together accounting for over half the yearly deaths.
Disease burden in India
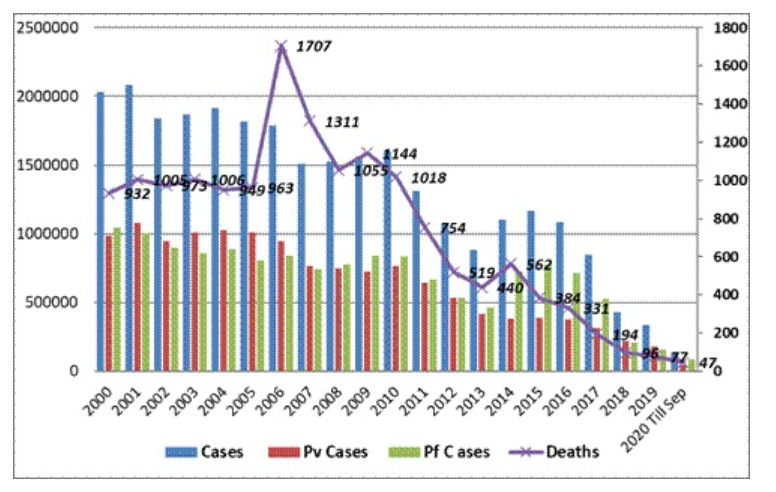
India is also one of the worst affected countries by malaria. Although there is a decrease in death cases now (93 deaths in 2020 from 1,018 in 2010) the infection rate continues to be in millions. The burden has been reduced through interventions such as antimalarial drugs, mosquito nets and insecticides:
According to the World Malaria Report 2020, cases of Malaria in India dropped from about 20 million in 2000 to about 5.6 million in 2019.
What are the global and national initiatives to curb Malaria?
Global Initiatives
E-2025 Initiative: The E-2020 initiative was launched by WHO in 2017. Building on the successes of the E-2020, WHO has launched the E-2025 initiative. As part of this initiative, WHO has identified 25 countries that have the potential to eliminate malaria within a 5-year timeline.
The countries will receive technical and on-the-ground support from WHO and its partners, in their work towards the target of zero malaria. In return, the countries will audit their elimination programs annually, participate in elimination forums, conduct surveillance assessments, and share malaria case data periodically.
High Burden to High Impact (HBHI): It was launched by WHO in 11 high malaria burden countries, including India. The initiative has four key response elements: (i) Political will to reduce malaria deaths (ii) Strategic information to drive impact (iii) Better guidance, policies, and strategies, and (iv) A coordinated national malaria response.
In India, the Implementation of the HBHI initiative started in four states West Bengal, Jharkhand, Chhattisgarh, and Madhya Pradesh in July 2019.
Asia Pacific Leaders Malaria Alliance (APLMA): It has set a target for malaria elimination in all countries of the Asia Pacific region by 2030 as per its Malaria Elimination Roadmap. India is also a member of APLMA.
National Initiatives
National Framework for Malaria Elimination in India (2016-2030): It aims to eliminate malaria nationally and contribute to improved health, quality of life and alleviation of poverty.
National Strategic Plan for malaria elimination (2017-2020): Under the plan, the country has been stratified into four categories based on the malaria burden – category 0 to category 3 and have different targets for each categories.
National Vector Borne Disease Control Programme (NVBDCP): It was launched in 2003-04 by merging the National anti-malaria control programme, National Filaria Control Programme and Kala Azar Control programmes.
Malaria Elimination Research Alliance-India (MERA-India): It was launched by the Indian Council of Medical Research (ICMR). It is a conglomeration of partners working on malaria control. The aim is to harness and reinforce research in a coordinated way in order to achieve a tangible impact on malaria elimination.
What are the challenges in eliminating Malaria from India?
Weak surveillance system: A key impediment to eliminating malaria is a weak surveillance system. India and Nigeria, two major contributors to the global burden of malaria, were able to detect only 8% and 16% of cases, respectively, via the system.
More Plasmodium vivax cases: Nearly half of plasmodium vivax cases were traced in India. This could at least be partially explained by resistance to chloroquine, the first-line treatment to p. vivax infections, that have been detected in pockets of the country earlier this decade.
Note: The Mosquirix offers no protection against P vivax malaria.
Porous borders and migrant movement: The North-eastern states share their border with neighbouring countries such as Myanmar and Bangladesh where malaria is still prevalent and there is a persistent threat of an influx of malaria cases from these countries.
Prevalence of Urban Malaria: Increased population pressure, insufficient capacity of the civic bodies to deal with water supply, and sewage and solid waste disposal have led to increased transmission of malaria in urban areas.
How India can reduce the Malaria burden?
It is important to address human resource challenges to effectively implement malaria control programs. Training programmes at the national and sub-national level for entomologists, epidemiologists and physicians should be provided.
A cross-border malaria strategy with the neighbouring countries is crucial to maintain and achieve the aims of malaria elimination.
It is important to conduct systematic drug resistance studies and monitoring. Antimalarial drug policies should also seek to address operational issues such as surveillance, diagnosis, compliance, health-seeking behaviour of the malaria-affected communities.
Though the Mosquirix does not offer protection to Plasmodium vivax cases, India can start vaccinating the citizens, especially in the HBHI regions of the country to reduce the P. falciparum type. This will significantly reduce India’s disease burden.




